1
Using Generative AI to Simulate Patient History-Taking in a Problem-Based
Learning Tutorial: A Mixed-Methods Study
Allison Mool, Jacob Schmid, Thomas Johnston, William Thomas, Emma Fenner, Kevin Lu,
Raya Gandhi, Adam Western, Brendan Seabold, Kodi Smith, Zachary Patterson, Hannah Feldt,
Daniel Vollmer, Roshan Nallaveettil, Anthony Fanelli, Logan Schmillen, Shelley Tischkau, PhD,
Anna T. Cianciolo, PhD, Pinckney Benedict, MFA, Richard Selinfreund, PhD
Allison Mool is a 2
nd
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0009-0006-5235-4646. (CRediT taxonomy roles: investigation,
methodology, writing original draft)
Jacob Schmid is a 2
nd
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0009-0000-8930-3718. (CRediT taxonomy roles:
conceptualization, investigation, methodology)
Thomas Johnston is a 4
th
year medical student, Southern Illinois University School of
Medicine, Springfield, Illinois; ORCID: 0009-0007-5319-9307. (CRediT taxonomy roles:
methodology, writing original draft)
William Thomas is an undergraduate student in anthropology, Southern Illinois University,
Carbondale, Illinois; ORCID: 0009-0000-8372-4183. (CRediT taxonomy roles: formal analysis,
investigation, methodology)
Emma Fenner is a 4
th
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0000-0002-9066-3507. (CRediT taxonomy roles:
conceptualization)
Kevin Lu is a 2
nd
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0000-0002-8459-5480. (CRediT taxonomy roles: investigation,
resources)
Raya Gandhi is a 2
nd
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0009-0009-1601-3838. (CRediT taxonomy roles: formal analysis,
investigation, resources)
Adam Western is a 3
rd
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0009-0009-5953-967X. (CRediT taxonomy roles:
conceptualization, resources)
Brendan Seabold is a 3
rd
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0009-0008-4494-9863. (CRediT taxonomy roles: resources)
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice.
2
Kodi Smith is a 1
st
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0009-0004-5921-9004. (CRediT taxonomy roles: formal analysis,
methodology, software, writing original draft)
Zachary Patterson is a 1
st
year medical student, Southern Illinois University School of
Medicine, Springfield, Illinois; ORCID: 0009-0008-7566-1088. (CRediT taxonomy roles: formal
analysis, methodology, software, writing original draft)
Hannah Feldt is a 1
st
year medical student, Southern Illinois University School of Medicine,
Springfield, Illinois; ORCID: 0009-0006-6189-4767. (CRediT taxonomy roles: formal analysis,
methodology, software, writing original draft)
Daniel Vollmer is an undergraduate student in computer science, Southern Illinois University,
Carbondale, Illinois; ORCID: 0009-0005-8874-4817. (CRediT taxonomy roles: software)
Roshan Nallaveettil is an undergraduate student in computer science, Southern Illinois
University, Carbondale, Illinois; ORCID: 0009-0008-7033-5814. (CRediT taxonomy roles:
software)
Anthony Fanelli, is an undergraduate student in computer science, Southern Illinois University,
Carbondale, Illinois; ORCID: 0009-0007-6817-9827 (CRediT taxonomy roles: software)
Logan Schmillen is an undergraduate student in computer science, Southern Illinois University,
Carbondale, Illinois; ORCID: 0009-0007-7287-1867 (CRediT taxonomy roles: software)
Shelley Tischkau is professor and Chair, Department of Pharmacology, Southern Illinois
University School of Medicine, Springfield, Illinois; ORCID: 0000-0002-8016-6398. (CRediT
taxonomy roles: conceptualization, investigation)
Anna T. Cianciolo is professor, Department of Medical Education, Southern Illinois University
School of Medicine, Springfield, Illinois; ORCID: 0000-0001-5948-9304. (CRediT taxonomy
roles: conceptualization, formal analysis, writing original draft)
Pinckney Benedict is professor, Department of English, and Director, Center for Virtual
Expression (CVEX), Southern Illinois University, Carbondale, Illinois; ORCID: 0009-0001-
5942-6968. (CRediT taxonomy roles: conceptualization, methodology, resources, visualization)
Richard Selinfreund is associate professor and Head of Pathology Group, Department of
Medical Microbiology, Immunology and Cell Biology, Southern Illinois University School of
Medicine, Springfield, Illinois; ORCID: 0000-0002-3778-5134. (CRediT taxonomy roles:
funding acquisition, methodology, project administration, resources, supervision)
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

3
Correspondence should be addressed to Richard Selinfreund, Department of Medical
Microbiology, Immunology and Cell Biology, Southern Illinois University School of Medicine,
PO Box 19626, Springfield, IL 62794-9626; telephone: (217) 545-4580; email:
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
4
Abstract
Background: Medical educators who implement problem-based learning (PBL) strive to balance
realism and feasibility when simulating patient cases, aiming to stimulate collaborative group
discussion, engage students’ clinical reasoning, motivate self-directed learning, and promote the
development of actionable scientific understanding. Recent advances in generative artificial
intelligence (AI) offer exciting new potential for patient simulation in PBL. Method: This study
used a between-groups, mixed-methods approach to (1) form a comprehensive picture of Year 2
medical student interactions with a generative AI-simulated patient in a PBL tutorial, as
compared to interactions with multimedia patient case materials; and (2) triangulate on the
impact these interactions had on learning. Two groups of students (N = 13) gathered patient
history information from a generative AI-enabled, 3D-animated avatar (AI condition). Two other
student groups (N = 13) gathered patient history information from a multimedia database using
keyword searching (Electronic PBL Module [ePBLM] condition). We used descriptive
observation to explore student interactions with both forms of the simulated patient, and we
quantitatively compared students’ perceptions of their learning experience and recall of patient
history information across conditions. Results: Students in the AI condition rated their present,
AI-augmented PBL learning experience—particularly its clinical accuracy and teamwork
aspects—significantly higher than they rated their previous PBL learning experiences using
ePBLMs. Recall of patient history information did not differ between conditions. Descriptive
observation indicated that the AI avatar presented case content accurately, with an appropriate
amount of information provided in response to students’ questions. Students were highly
engaged as a group in taking a history from the avatar. However, although students used
language suggestive of anthropomorphizing of the AI (e.g., gender pronouns), they appeared to
orient to it as an augmented “question bank” for gathering patient history information, using a
questioning strategy akin to querying an ePBLM. Discussion: Optimizing AI implementation to
stimulate clinical reasoning and patient communication skills in PBL could include (1) starting
early, perhaps in Year 1, before an alternative interactional framework can take hold; (2)
orienting students to the AI to help them understand its capabilities; and (3) encouraging “play”
with or “discovery learning” of the AI’s capabilities.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
5
Introduction
In medical problem-based learning (PBL), patient cases provide the organizing structure of the
curriculum, serving as triggers for learning and providing a platform to exercise thinking
representative of physicians’ workplace cognition (Wee, Kek, & Sim, 2001).
Patient case design therefore is a key concern for PBL educators. Quality patient cases stimulate
collaborative group discussion, engage clinical reasoning, motivate self-directed learning, and
promote the development of actionable scientific understanding.
• Characteristics of a quality patient case – realistic, ideally based on a real patient, set in
a medical context, sufficiently challenging for students to stimulate high-level cognitive
engagement, designed based on clear learning objectives (Wee, Kek, & Sim, 2001;
Azer, Peterson, Guerrero, & Edgren, 2012)
• Characteristics of quality interactions with patient case materials (questioning oneself
and others, self-explanation and elaboration of ideas, testing one’s understanding, and
self-identification of knowledge and comprehension gaps – Cianciolo & Regehr, 2019)
The diversity of approaches to simulating patients in PBL ranges from paper cases to interactive
courseware to live patient actors, each with their own tradeoffs.
• Advantages of high-fidelity simulation (engaging and provides opportunity to practice
clinical skills – Barrows & Tamblyn, 1980; facilitates patient-centered learning –
MacLeod, 2011)
• Disadvantages of high-fidelity simulation (lack of control and potential to become too
complex – Barrows & Tamblyn, 1980; cost in time, personnel, and funding)
Recent advances in generative artificial intelligence (AI) offer exciting new potential for patient
simulation in PBL.
• Capabilities of generative AI for simulating people realistically – use of these
capabilities in gaming and for other non-medical purposes
• Ways that generative AI provides the advantages of high-fidelity simulation without the
disadvantages (guardrails)
• More realistic patients may stimulate renewed interest in PBL tutorials at a time when
engagement in our own curriculum and elsewhere is lacking (Dawood, Rea, Decker,
Kelley, & Cianciolo, 2021; Walling, Istas, Bonaminio, Paolo, Fontes, Davis, & Berardo,
2017; Kilgour, Grundy, & Monrouxe, 2016).
Generative AI-simulated patients offer higher fidelity patient simulation, with potentially greater
control, than what is currently feasible in most medical PBL curricula. However, AI
development can be time-consuming and expensive, and the technology is still evolving.
Research is needed to explore the impact of using generative AI to simulate patients in PBL
tutorials to understand how (and when) to best implement this new technology.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
6
Methods
Overview
This study used a between-groups, mixed-methods approach (Schifferdecker & Reed, 2009) to
(1) form a comprehensive picture of medical student interactions with a generative AI-simulated
patient in a PBL tutorial, as compared to interactions with multimedia patient case materials; and
(2) triangulate on the impact these interactions had on learning. Two groups of students gathered
patient history information from a generative AI-enabled, 3D-animated avatar (AI condition).
Two other student groups gathered patient history information from a multimedia database using
keyword searching (Electronic PBL Module [ePBLM] condition). We used descriptive
observation to explore student interactions with both forms of the simulated patient, and we
quantitatively compared students’ perceptions of their learning experience and recall of patient
history information across conditions.
Context/Setting
This study took place in March 2024 at a small, public, community-based medical school in the
Midwestern U.S. (class size = 72), which was the first institution to implement its PBL
curriculum using ePBLMs (Ryan & Koschmann, 1994). The 4-year curriculum follows a 2+2
design in which the first 2 years focus on preclinical, basic science instruction in a classroom
setting with periodic clinical exposure, and the second 2 years focus on clinical clerkships and
electives. The preclinical curriculum comprises spirally organized organ-system-based units;
Year 1 instruction emphasizes anatomy, physiology, and histology, and Year 2 emphasizes
pathophysiology and pharmacology. The curriculum is delivered using a hybrid PBL format
(Lim, 2012) in which participation in PBL tutorials is required, and attendance at correlated
lectures is recommended, but not mandatory.
PBL tutorials in our preclinical curriculum comprise small groups of 6-8 students and a
facilitator who meet multiple times per week (3 times/week in Year 1, 2 times/week in Year 2) to
exercise clinical reasoning with real-world patient cases, discuss understanding of the case
content, identify basic science knowledge gaps (i.e., learning issues), and develop shared
knowledge of the patient’s condition and its treatment (Koschmann, Glen, & Conlee, 1997;
Cianciolo, Kidd, & Murray, 2016). Procedurally, students work collaboratively to “open” the
case, which involves gathering patient information from history-taking, physical examination,
laboratory studies, and imaging to understand the patient’s medical concerns, form a differential
diagnosis, and identify learning issues to address with self-directed learning. Following self-
directed learning, students “close” the case by discussing their self-directed learning findings, the
implications of their new knowledge for understanding the patient case, and the patient’s care
outcomes. The students comprising PBL tutorial groups change each unit, for a total of 94
unique groups assigned across both years of the preclinical curriculum.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
7
Participants
Participants comprised 4 groups of second-year medical students (N = 26, 37% of the Class of
2026. Among the 14 participants who provided demographics, 79% self-identified as women and
20% self-identified as belonging to a marginalized racial/ethnic group. Students’ participation
occurred during the first 2 days of the final unit in the preclinical curriculum (Endocrinology,
Reproduction, and Gastroenterology [ERG]), approximately 3 months prior to taking Step 1 of
the USMLE Board Examination, and after nearly 2 years’ experience in our PBL (ePBLM)
curriculum. Participants were a convenience sample recruited via word of mouth by fellow
second-year medical students serving as co-investigators in this study. There were no
inclusion/exclusion criteria. Participants were allowed to choose their PBL tutorial group with
knowledge of who else was in their group. Groups were then assigned to the AI or ePBLM
condition depending on investigator availability and preference.
This study was deemed non-human subjects research by the Springfield Committee on Research
Involving Human Subjects (6 February 2024). The facilitator for all 4 groups, a faculty member
from the investigator team—who is locally considered a master PBL tutor with 16 years of
tutoring experience—described the study to participants and received their verbal consent to
participate with audio-recording. Participants were offered pizza and drinks during their tutorial,
but no other incentives were provided.
Materials
Patient Case – Randy Rhodes. The patient case used in this study is a 54-year-old man—Randy
Rhodes—who presents to the family medicine clinic with a rash on his arm. His diagnosis is
Diabetes Mellitus Type 2. The case is designed to teach pathology, pharmacology, and other
topics associated with this diagnosis (e.g., obesity and related metabolic syndromes) as one of 20
cases comprising the ERG PBL curriculum. Participants interacted with Randy Rhodes to gather
patient history information in one of 2 ways, ePBLM or generative AI:
ePBLM. ePBLMs have been used to simulate patients in our PBL curriculum for over 30
years. Developed locally to replace the spiral-bound notebooks of comprehensive case
information provided to students to role-play the patient, ePBLMs allow students to gather case
information serially by using keyword searches to simulate history-taking, physical examination,
testing/imaging, and procedures (Ryan & Koschmann, 1994). The ePBLM system returns
answers to students’ search queries as realistically as possible using multimedia. For instance, it
provides actual laboratory test or imaging results where possible, and it returns canned dialogue
snippets in response to patient history queries (e.g., “I’ve had this rash for 3 months.”) as well as
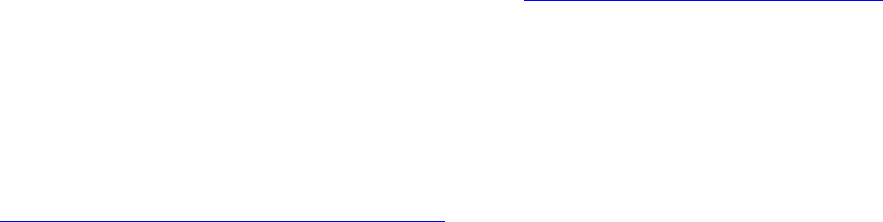
offering information about patient progression throughout their treatment. Figure 1 presents a
screen capture of the ePBLM interface for the Randy Rhodes case.
Generative AI. Students gather patient history information from the AI-enabled patient
via voice-to-voice interaction with a 3D-animated avatar situated in a clinical exam room
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

8
environment created using Unreal Game Engine 5.0 and Metahuman (Figure 2). The content of
the avatar’s responses to students’ history-taking questions—generated using the convai
platform—is produced via prompts to a general large language model that have been engineered
using the existing Randy Rhodes ePBLM database. The scope of the avatar’s responses is shaped
by “guardrails” placed by the development team to optimize the case’s educational value. For
instance, one guardrail prevents Randy Rhodes from revealing his diagnosis directly to students.
Situated within a game engine, the AI also is capable of responding with different degrees of
friendliness depending on how students interact with it. For example, the AI is trained to respond
irritably to history questions laden with medical jargon and, if guardrails had not been
implemented to prevent it, could storm out of the exam room.
1
Interactions with the AI in this
context may take forms other than questions; the avatar can respond to empathic statements and
even tell jokes.
Learner Perceptions Survey. This paper-based 8-item survey assessed participants’ perceptions
of PBL tutorials using either ePBLM or AI. Participants used a scale of 1 to 5 to rate how
positively they view several aspects of tutorial quality and impact (impact on improving clinical
knowledge, clinical simulation accuracy, impact on clinical knowledge retention, enjoyability,
stressfulness, allowance for teamwork, interestingness, impact on confidence) when either
format is used. Both forms of the survey (ePBLM and AI) are presented in the supplemental
appendix. A composite score for each form was created by summing the ratings across all 8
items (Item 5 was reverse coded). The possible range of scores was 8 to 40, representing how
positively participants view their overall PBL tutorial experience using each format.
Patient History Information Quiz. This paper-based quiz (supplemental appendix) consisted of
11 short-answer questions to assess participants’ knowledge of Randy Rhodes’s demographic
information, medical history, and symptoms immediately following the PBL tutorial and 2 weeks
later. Quizzes were graded by 2 student co-investigators masked to the condition (ePBLM or AI)
and timing (immediate or delayed) when the quiz was completed. According to a faculty-verified
key, each short answer could receive 0 points, ½ point, or 1 point, and the possible range of total
scores was 0 to 11, representing overall recall of patient history information available in the
Randy Rhodes case. Both co-investigators independently graded the first 5 quizzes to establish
consistency with the rating criteria, after which 1 co-investigator graded the remaining 52
quizzes.
Descriptive Observation Notes. Five co-investigators conducted descriptive observation
(Spradley, 1980) of the audio-recorded tutorials, documenting their notes using a template
created locally by a well-established medical education researcher (supplemental appendix). The
template prompted observers to (1) document a reflexivity reflection; (2) specify (with time
stamp) and describe noteworthy occurrences observed in the audio-recording; and (3) report in
bracketed fashion their reactions to these noteworthy occurrences. The lead observer was a
1
Randy’s developers removed the door from the examination room such that storming out is no longer possible.
Instead, the avatar will disengage from a problematic interaction and steer the conversation back toward the rash on
his arm, which is his pressing concern and motivation for seeing a doctor.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
9
behavioral scientist with experience conducting observational research of PBL tutorials
(Cianciolo, Kidd, & Murray, 2016). The other observers were first and second-year medical
student co-investigators enrolled in our preclinical curriculum.
Procedure
All 4 PBL tutorials took place in a small laboratory room arranged to mimic a typical PBL
tutorial classroom (Figure 3). The room was equipped with tables, chairs, a whiteboard, and the
tools needed to interact with the patient in each group: a keyboard and mouse to search the
ePBLM database and a push-to-talk microphone to communicate verbally with the AI-enabled
patient. The room also contained a computer monitor for presenting the simulated patient
visually.
After consent and before beginning their PBL tutorial, participants filled out the Learner
Perceptions Survey – ePLBM. That is, participants rated their perceptions of ePBLM tutorials
generally, based on their nearly 2 years’ experience in our PBL curriculum. Survey
administration was proctored by 1 of 4 student co-investigators who attended the tutorials for this
purpose as well as to answer participant questions, operate the push-to-talk microphone (AI
groups), and manage the tutorial’s other technology, such as audio-recording. Audio-recording
was accomplished via videoconferencing software (WebEx).
With minimal direction from the faculty facilitator, all 4 groups conducted a case opening, which
ranged in duration from 36 to 75 minutes and consisted of history taking. After completing the
case opening and before leaving the laboratory room, participants retook the Learner Perceptions
Survey, this time rating their perceptions of PBL tutorials using the type of simulated patient
they had just interacted with (ePBLM or AI). Participants also completed the Patient History
Information Quiz.
Two weeks after the tutorials, participants individually retook the Patient History Information
Quiz, proctored by a student co-investigator, in various campus locations of convenience for
each participant. Student co-investigators graded the quizzes after all quizzes had been
completed. Descriptive observation of the audio-recordings began after all 4 tutorials had
occurred.
Data Analysis
Quantitative analysis. Quantitative analyses were conducted using linear mixed models to
control for within-group variance while examining the effect of condition (ePBLM vs. AI) on
participants’ perceptions and recall of patient history information. P-values of .05 or smaller
were deemed statistically significant. All analyses were performed using R version 4.3.2 (R Core
Team 2023).
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
10
Qualitative analysis. Observation notes were analyzed inductively to characterize the
interactions among students and the simulated patient in each group. For each of the 4 groups,
the lead analyst compiled the independent observers’ notes into one set. These compiled notes
were arranged chronologically to create a detailed, multi-perspective characterization of
noteworthy events and associated bracketed reflections that occurred during each tutorial. To
highlight the different perspectives at a glance, the lead analyst represented each observers’ notes
using a different text color. Next, all qualitative analysts independently reviewed each set of
compiled field notes to identify regularities in the interactions among people and case materials.
Flagged as regularities were recurring interactional behaviors such as consistencies in patient
questioning strategies or commonalities among occurrences of pauses or silence in group
interactions. Analysis also flagged interactional behaviors potentially reflective of how students
oriented to the patient case or each other (e.g., referring to the patient with personal pronouns or
seeking input from peers in asking history-taking questions). Finally, all qualitative analysts
collaboratively reviewed regularities and noteworthy interactional behaviors within and across
participant groups to develop patterns in PBL behavior associated with type of simulated patient.
Results
Learner Perceptions Survey Data
Linear mixed modeling of the Learner Perceptions Survey data revealed a significant effect of
time (pre- vs. post-tutorial) for the AI condition only (Table 1). Specifically, participants’ post-
tutorial ratings of their overall PBL learning experience were, on average, 6 points higher than
their pre-tutorial ratings if their tutorial involved an AI-enabled patient. In other words, students
in the AI condition rated their present, AI-augmented PBL learning experience significantly
higher overall than they rated their previous PBL learning experiences using ePBLMs. Students
in the ePBLM condition perceived their present PBL learning experience to be approximately the
same as their previous PBL learning experiences using the same technology.
[INSERT TABLE 1 HERE.]
The item-level data in Table 2 indicate that students’ post-tutorial perceptions of their learning
experience in the AI condition were higher than their pre-tutorial perceptions almost across the
board. Particularly noteworthy is the difference in perceptions of clinical simulation accuracy; on
average, students who gathered patient history information from an AI-enabled patient rated the
clinical accuracy of their present PBL tutorial 1.6 points higher (on a 5-point scale) than the
clinical accuracy of their previous PBL tutorials using ePBLMs.
[INSERT TABLE 2 HERE.]
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
11
Patient History Quiz Data
Linear mixed modeling of the Patient History Quiz data revealed a significant effect of time only
(Table 3). Specifically, students’ recall of Randy Rhodes’s patient history information decreased
significantly from immediate to delayed assessment, across both conditions (ePBLM and AI).
Immediate and delayed recall of patient history information slightly favored the AI condition
(10.1 vs. 9.4 immediate recall for the AI and ePBLM conditions, respectively; 8.6 vs. 7.9 delayed
recall for the AI and ePBLM conditions, respectively), however this difference was
nonsignificant, and the rate of forgetting did not differ between the 2 conditions. Of note,
immediate recall performance was near ceiling (maximum quiz score = 11 points) in both
conditions, and delayed recall was also very high.
[INSERT TABLE 3 HERE.]
Observation Data
Initial impressions from the observation of one group in the AI condition:
• The AI presented case content accurately, with an appropriate amount of information
provided in response to students’ questions. The students appeared to find the avatar’s
appearance, voice quality, and behavior plausible – with no language to suggest an
aversive reaction to the patient representation (i.e., being in the uncanny valley).
• Although students used language suggestive of anthropomorphizing of the AI (e.g.,
gender pronouns, inferences about the AI’s emotional state), they appeared to orient to it
as an augmented “question bank” for gathering patient history information. The format
and style of their questions was consistent with how patient history information is
gathered from the ePBLM (i.e., singularly focused on diagnosis) versus a more
naturalistic conversation with the AI (i.e., diagnostically oriented, yet inclusive of
rapport-building). Potential explanations for this include:
o As rising third-years, the students were very experienced with using ePBLMs, and
likely brought this framework for conducting PBL to the study.
▪ This frame may have been reinforced by using a patient case that is a
required part of the curriculum versus an optional, experimental case.
▪ Further, the faculty facilitator did not offer participants a divergent
perspective for how the AI might be used.
o Voice communication with the AI was mediated by a student co-investigator, who
operated the push-to-talk microphone at students’ request. The additional layer
between the students and the AI may have created a communication bottleneck
that reduced the likelihood of naturalistic interactions.
• Students were very engaged, as a group, in history taking with the AI-enabled Randy
Rhodes.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
12
o Students seemed to enjoy the novelty of the AI avatar, commenting on its
appearance and reactions to what they said. The whole group seemed engaged in
troubleshooting the AI’s unexpected behaviors (i.e., irritability).
o To communicate effectively with the AI, students had to frame their questions
naturalistically instead of in terms of the keywords they were used to using. The
whole group seemed engaged in troubleshooting what questions to ask.
Discussion
Although using a generative AI-enabled patient simulation in a PBL tutorial had limited impact
on recall of patient history information—which was near ceiling in both the ePBLM and AI
conditions—students in the AI condition reported that the tutorial was more enjoyable and
facilitative of teamwork than did students in the ePBLM condition. Descriptive observation of
participants’ audio-recorded interactions in the PBL tutorials reinforced students’ self-reports
and help to characterize what was enjoyable and engaging about taking a history from an
artificially intelligent patient. Observation also provides insight into how to maximize the impact
of generative AI-enabled patient simulations for clinical learning in the PBL context.
Results in the context of the PBL literature WRT patient simulation.
Implications of results for optimizing AI implementation in PBL.
• Start implementation of AI early, perhaps in the first year, before an alternative
framework can take hold.
• Provide students with an orientation to the AI agent to help them understand its
capabilities (perhaps during the Year 1 orientation to PBL).
• Encourage “play” with or “discovery learning” of the AI’s capabilities.
Study limitations
• One case at one medical school (but more than one-third of the class)
• Study involved students very experienced with PBL and in the final unit of preclinical
instruction preceding the Step 1 board examination
• Students were not randomly allocated to groups (although groups were randomly
allocated to condition, and there did not appear to be systematic differences across
condition in pre-existing social connections)
• Lack of video data to conduct more comprehensive observations
• Lack of a human-simulated patient to offer a comparison case (e.g., it is impossible to
know whether students would orient to a human role-player as an augmented question
bank)
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
13
Future applications of AI in PBL and elsewhere in the medical curriculum
• More diverse and varied patient interactions than traditional standardized patients while
saving on time, scheduling, and training of standardized patients
• Potential for simulating telehealth visits and conducting standardized patient
examinations
• Communication skills assessment (e.g., use of accessible language) through the
adaptability of the AI to provide slightly different responses based on the phrasing of
users' questions
• Scalability of AI across different stages of medical education, from preclinical students
learning to communicate and diagnose to clinical students learning treatment and
management to residents and fellows learning to navigate complex or uncommon patient
interactions
Acknowledgements: We would like to thank Don Torry, PhD, for his guidance and continued
focus related to research strategy; Debra L. Klamen, MD, MHPE, for her continued support for
this project; and Sean McGinity BS, BA for his support to the quantitative data analysis. Finally,
we would like to acknowledge the medical students from the Class of 2026 who participated in
this study.
Funding/Support: This project received funding from 3 internal sources at Southern Illinois
University School of Medicine (SIU-SOM): Dean’s Start-up Funds; SIU-SOM Concept
Development Award; and an SIU-SOM Foundation Grant for Diabetes Research.
Previous presentations: Earlier versions of this work were presented at the 2024 Central Group
on Educational Affairs Spring Meeting, Milwaukee, Wisconsin, April 3-5, 2024 and at the SIU-
SOM 14th Annual Teaching and Learning Symposium, Springfield, IL, April 11, 2024.
Ethical approval: This project was deemed non-human subjects research by the Springfield
Committee on Research Involving Human Subjects (6 February 2024).
References
Wee LK, Kek MY, Sim MH. Crafting effective problems for problem-based learning. In
Proceedings of the 3rd Asia-Pacific Conference on Problem-Based Learning. 2001 Jan 1.
Azer SA, Peterson R, Guerrero APS, Edgren G. Twelve tips for constructing problem-based
learning cases. Med Teach. 2012;34:361-367.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
14
Barrows HS, Tamblyn RM. Problem-based learning: an approach to medical education. Springer
Publishing Company; 1980.
MacLeod A. Six ways problem-based learning cases can sabotage patient-centered medical
education. Acad Med. 2011;86:818-825.
Cianciolo AT, Regehr G. Learning theory and educational intervention: producing meaningful
evidence of impact through layered analysis. Acad Med. 2019;94(6):789-794.
Dawood O, Rea J, Decker N, Kelley T, Cianciolo AT. Problem-based learning about problem-
based learning: lessons learned from a student-led initiative to improve tutor group interaction.
Med Sci Educ. 2021;31:395-399.
Walling A, Istas K, Bonaminio GA, Paolo AM, Fontes JD, Davis N, Berardo BA. Medical
student perspectives of active learning: a focus group study. Teach Learn Med. 2017;29(2):173-
180.
Kilgour JM, Grundy L, Monrouxe LV. A rapid review of the factors affecting healthcare
students' satisfaction with small-group, active learning methods. Teach Learn Med.
2016;28(1):15-25.
Schifferdecker KE, Reed VA. Using mixed methods research in medical education: basic
guidelines for researchers Med Educ. 2009;43(7):637-644.
Lim WK. Dysfunctional problem-based learning curricula: Resolving the problem. BMC Med
Educ 2012;12:89.
Koschmann T, Glenn P, Conlee M. Analyzing the emergence of a learning issue in a problem-
based learning meeting. Med Educ Online. 1997;2(1). https://doi.org/10.3402/meo.v2i.4290
Cianciolo AT, Kidd B, Murray S. Observational analysis of near‐peer and faculty tutoring in
problem‐based learning groups. Med Educ. 2016;50(7):757-767.
Ryan C, Koschmann T. The Collaborative Learning Laboratory: a technology-enriched
environment to support problem-based learning. Paper presented at the National Educational
Computing Conference, 1994, Boston, MA. Available at:
https://files.eric.ed.gov/fulltext/ED396678.pdf.
Spradley JP. Participant observation. Wadsworth: Thomson Learning. 1980.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
15
Figure 1. Screen Capture of the Randy Rhodes ePBLM
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

16
Figure 2. Screen Capture of Randy Rhodes, the Generative AI-enabled Patient
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

17
Figure 3. Photo of the Laboratory Room in Which the PBL Tutorials Took Place
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

18
Table 1. Linear Mixed Model of Learner Perceptions Survey Data
Survey total
Predictors
Estimates
std. Error
CI
Statistic
p
(Intercept)
23.77
1.13
16.94 – 30.59
21.02
0.008
Time: post
0.23
0.98
-1.80 – 2.26
0.23
0.817
Condition: AI
-1.38
1.60
-6.49 – 3.72
-0.87
0.451
timepost:conditionAI
5.77
1.39
2.90 – 8.64
4.14
<0.001
Random Effects
σ
2
6.30
τ
00
id
10.00
τ
00
group
0.00
τ
11
group.conditionAI
0.00
ρ
01
group
-0.98
ICC
0.61
N
group
4
N
id
26
Observations
52
Marginal R
2
/ Conditional R
2
0.241 / 0.707
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

19
Table 2. Learner Perceptions Survey Item-Level Data – Mean (SD)
Survey Item
Pre-Tutorial (N = 26)
Post-Tutorial (N = 26)
AI (N = 13)
ePBLM (N = 13)
AI (N = 13)
ePBLM (N = 13)
Improves
clinical
knowledge
3.8 (0.6)
3.8 (0.9)
4.2 (0.6)
3.6 (0.7)
Simulates
clinical
experiences
accurately
2.6 (1.0)
3.1 (1.0)
4.2 (0.6)
3.5 (0.9)
Helps clinical
knowledge
retention
3.6 (1.0)
3.6 (1.0)
4.3 (0.6)
3.5 (0.9)
Is enjoyable
3.5 (0.8)
3.7 (0.6)
4.7 (0.5)
3.8 (0.8)
Is stressful*
4.1 (0.5)
3.9 (0.5)
3.8 (0.8)
4.2 (0.6)
Allows for
teamwork
3.8 (0.4)
4.0 (0.4)
4.5 (0.7)
4.0 (0.6)
Stimulates
interest in
learning the
disease at hand
3.4 (0.9)
3.8 (0.7)
4.4 (0.5)
3.8 (0.8)
Improves
confidence
interacting with
this chief
complaint
3.5 (1.0)
3.8 (0.7)
4.2 (0.8)
3.5 (0.7)
TOTAL
28.4 (0.4)
29.8 (0.3)
34.4 (0.3)
30.0 (0.3)
*This item is reverse-coded such that a higher score represents lower perceived stress.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
20
Table 3. Linear Mixed Model of Patient History Quiz Data
Quiz
Predictors
Estimates
std. Error
CI
Statistic
p
(Intercept)
9.40
0.32
7.55 – 11.26
29.32
0.004
Time: post
-1.46
0.29
-2.05 – -0.87
-5.07
<0.001
Condition: AI
0.69
0.41
-1.09 – 2.48
1.71
0.233
Random Effects
σ
2
1.08
τ
00
id
0.50
τ
00
group
0.00
τ
11
group.conditionAI
0.00
ρ
01
group
-1.00
N
group
4
N
id
26
Observations
52
Marginal R
2
/ Conditional R
2
0.382 / NA
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
21
Supplemental Appendix
Learner Perceptions Survey (ePBLM Condition)
Pre-Tutorial
Based on your past experience with ePBLM problem-based learning sessions, please give your
opinions on each of these statements:
1. I think that ePBLM problem-based learning sessions improve my clinical knowledge.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
2. I think that ePBLM problem-based learning sessions simulate clinical experiences
accurately.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
3. I think that seeing patients in ePBLM problem-based learning sessions helps me retain
knowledge about the clinical situations.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
4. I think that ePBLM problem-based learning sessions are enjoyable.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
5. I think that ePBLM problem-based learning sessions are stressful.
1) Strongly disagree
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
22
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
6. I think that ePBLM problem-based learning sessions allow for teamwork.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
7. I think that ePBLM problem-based learning sessions stimulate my interest in learning
about the disease at hand.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
8. I usually feel more confident interacting with chief complaints after ePBLM tutor group
sessions.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

23
Post-Tutorial
1. I think that this ePBLM problem-based learning session improved my clinical
knowledge.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
2. I think that this ePBLM problem-based learning session simulated clinical experiences
accurately.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
3. I think that seeing the patient in this ePBLM problem-based learning session will help me
retain knowledge about the clinical situation.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
4. I think that this ePBLM problem-based learning session was enjoyable.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
5. I think that this ePBLM problem-based learning session was stressful.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
6. I think that this ePBLM problem-based learning session allowed for teamwork.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

24
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
7. I think that this ePBLM problem-based learning session stimulated my interest in
learning about the disease at hand.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
8. I feel more confident interacting with this complaint after this ePBLM tutor group
session.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

25
Learner Perceptions Survey (AI Condition)
Pre-Tutorial
Based on your past experience with ePBLM problem-based learning sessions, please give your
opinions on each of these statements:
1. I think that ePBLM problem-based learning sessions improve my clinical knowledge.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
2. I think that ePBLM problem-based learning sessions simulate clinical experiences
accurately.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
3. I think that seeing patients in ePBLM problem-based learning sessions helps me retain
knowledge about the clinical situations.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
4. I think that ePBLM problem-based learning sessions are enjoyable.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
5. I think that ePBLM problem-based learning sessions are stressful.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

26
4) Agree
5) Strongly agree
6. I think that ePBLM problem-based learning sessions allow for teamwork.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
7. I think that ePBLM problem-based learning sessions stimulate my interest in learning
about the disease at hand.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
8. I usually feel more confident interacting with chief complaints after ePBLM tutor group
sessions.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

27
Post-Tutorial
1. I think that this autonomous AI problem-based learning session improved my clinical
knowledge.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
2. I think that this autonomous AI problem-based learning session simulated clinical
experiencing accurately.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
3. I think that seeing the patient in this autonomous AI problem-based learning session will
help me retain knowledge about the clinical situation.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
4. I think that this autonomous AI problem-based learning session was enjoyable.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
5. I think that this autonomous AI problem-based learning session was stressful.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

28
6. I think that this autonomous AI problem-based learning session allowed for teamwork.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
7. I think that this autonomous AI problem-based learning session stimulated my interest in
learning about the disease at hand.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
8. I feel more confident interacting with this complaint after this autonomous AI tutor group
session.
1) Strongly disagree
2) Disagree
3) Neither agree nor disagree
4) Agree
5) Strongly agree
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
29
Patient History Information Quiz
1. What was Randy’s chief complaint?
2. Did anything seem to help relieve Randy’s chief complaint?
3. What was Randy’s diet like?
4. What was Randy’s occupation?
5. Did Randy have any notable past medical history?
6. Was there any remarkable family medical history?
7. What were some of Randy’s lifestyle habits?
8. Did Randy have any weight changes? If so, what were they?
9. What were Randy’s sleep habits like?
10. What were Randy’s demographics?
11. Did Randy have any genitourinary symptoms?
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint

SIU School of Medicine Naturalistic Field Observation Tool
30
Descriptive Observation Notes Template
Date of recording:
Case Type (AI or ePBLM):
Group Size (number of students):
Observer (your name):
Observer reflexivity:
Description of Location/Space:
Name and role of the research assistant in this session:
Take detailed notes on everything you observe that you deem to be noteworthy. These notes should provide (but may not be limited to) detailed descriptions
of anything related to student interactions with the PBL case medium (AI or ePBLM), case content, each other, and the tutor. Can include direct quotes.
Timestamp
(Taken from
recording)
Observation of Activity
(Who, What, When, Where, How)
Reflections
(Your Thoughts On What You Observe)
Example:
0:07:21
Student asks the AI a question, referring to the AI by name, reacts
with apparent frustration to the AI’s indirect response to their
question.
Interesting that the student treats the AI like a person, and has
emotional reactions to what it says.
All rights reserved. No reuse allowed without permission.
(which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.
The copyright holder for this preprintthis version posted May 3, 2024. ; https://doi.org/10.1101/2024.05.02.24306753doi: medRxiv preprint
