
Oregon’s Public Children’s Behavioral Health
System: A Review of Financing to Support a
More Efficient and Effective System of Care
for Oregon’s Children, Youth & Young Adults
April 2024
DEBORAH S. HARBURGER & LENA BILIK
INNOVATIONS INSTITUTE, UNIVERSITY OF CONNECTICUT SCHOOL OF SOCIAL WORK
SUZANNE FIELDS
SUZANNE FIELDS CONSULTING, LLC
2
Contents
Introduction & Methods .......................................................................................................................... 3
Oregon’s Medicaid Structure ................................................................................................................ 4
Findings & Recommendations ............................................................................................................. 7
Early and Periodic Screening, Diagnostic and Treatment (EPSDT) Benefit .................. 8
Covered Services .............................................................................................................................. 9
Implementation Support ............................................................................................................. 10
Expanding Access and Support through the 1115 Waiver ................................................... 12
Child Welfare & Juvenile Justice-Involved Children ............................................................. 13
Additional Managed Care Oversight & Regional Design Findings .................................. 16
State Plan Options to Support Youth with Behavioral Health & Co-Occurring
Intellectual & Developmental Disability (I/DD) Service Needs ......................................... 18
Substance Use Disorder 1115 Demonstration Waiver ............................................................ 21
Open-Card (Fee-for-Service) System......................................................................................... 21
Intensive In-Home Behavioral Treatment (IIBHT) Services ............................................... 22
Diagnosis to Support Effective Treatment of Young Children ........................................ 23
Metrics and Quality Measurement ............................................................................................... 24
Workforce Challenges & Opportunities .................................................................................... 25
Conclusion ................................................................................................................................................. 28
Appendix ................................................................................................................................................... 30
Appendix A: Review Process ......................................................................................................... 31
Document Review .......................................................................................................................... 31
Key Informant Interviews ........................................................................................................... 33
Appendix B: Table of Recommendations ................................................................................. 34
This report was prepared under contract with the Oregon Health Authority, Health Systems Division, Child and
Family Behavioral Health (Agreement Number 179117-0). It may be cited as Harburger, D.S., Bilik, L., & Fields, S.
(2024).
Oregon’s Public Children’s Behavioral Health System: A Review of Financing to Support a More Efficient
and Effective System of Care for Oregon’s Children, Youth & Young Adults.
Innovations Institute, University of
Connecticut School of Social Work.
The findings and recommendations contained in this report are those of the authors alone and do not necessarily
reflect the opinions or policies of the State of Oregon.
April 2024 Update: This version of the report is an update to the report issued in February 2024. The section
State Plan Options to Support Youth with Behavioral Health & Co-Occurring Intellectual & Developmental
Disability (I/DD) Service Needs
was updated based on valuable feedback received from family members and
caregivers at the Oregon Children’s System Advisory Council in April 2024. The text now reflects improved
nuance in the findings and recommendations related to decision-making about genetic testing to support the
diagnosis and treatment of youth with intellectual and developmental disabilities. The remainder of the report
is unchanged from the prior version.

3
Introduction & Methods
In 2023, the Oregon Health Authority (OHA), Health Systems Division, Child and Family
Behavioral Health contracted with Innovations Institute at the University of Connecticut
School of Social Work to conduct a holistic system assessment of their current Medicaid
State Plan and waiver structure in Oregon for children, youth, and young adults through
age 25. The request was to review the existing financing structures and approaches and
make immediate, medium- and long-term recommendations to inform the development of
a more efficient and effective System of Care (SOC) for Oregon’s children, youth, and
young adults.
The goal of this review was to identify
• The missing components from the Centers for Medicare & Medicaid Services (CMS)-
approved authorities that would benefit the children’s system of care;
• The efficiency of transitions between and within authorities, settings, and services;
• Barriers to OHA’s goal of health equity by 2030
• The applicability and coherency of current waiver language.
• Areas where the implementation of waivers by Coordinated Care Organizations
(CCO)s do not align between CCOs; or whether CCO implementation of contractual
requirements are causing barriers for member transition between CCOs.
This review was conducted with support from OHA and their partner agencies. Most of the
findings and recommendations are based on a desk review of documents, augmented by
conversations and interviews with key partners. The appendix includes a list of documents
reviewed for this analysis and a list of people interviewed. Readers are advised to
remember that this document is a review of existing documents and materials and is not a
strategic plan. While many partners across Oregon may benefit from reviewing the report
and its findings, the primary audience of this report is OHA and its sister agencies. Further,
the findings and recommendations in this report reflect the opinions of the authors and do
not necessarily reflect those of OHA or its sister agencies.
The recommendations in this document originate from extensive experience in analyzing,
evaluating, and advising child- and family-serving agencies across the country on Medicaid
and behavioral health services for children, youth, young adults, and their families. We have
included examples that illustrate our recommendations. We are mindful that the
recommendations we make require considerable intra- and interagency cooperation, and
we have provided initial guidance on how to implement the recommendations.
Apart from our prior experience and lessons learned from across the country, our
recommendations are grounded in System of Care (SOC) values.
1
Systems that serve and
support children, youth, young adults, and their families should be family- and youth-
driven; home- and community-based; equitable; culturally humble, linguistically
competent, and fully accessible; strengths-based and individualized; data driven and
outcome oriented; and trauma-responsive.
The state and its local and regional partners collectively have spent years working to
reform and improve its behavioral health system for children, youth and families. The
structures and financing in place reflect that. The findings and recommendations are
1
Adapted from Stroul, B. A., Blau, G. M., Larson, J. M. (2021).
The Evolution of the System of Care
Approach for Children, Youth, and Young Adults with Mental Health Conditions and Their Families
. The
Institute for Innovation and Implementation, University of Maryland, Baltimore.

4
designed to highlight areas where Oregon can refine, design, or implement strategies and
approaches to enhance solutions to build upon the state’s strengths while addressing its
challenges. Additionally, we recognize that Oregon has continued to make improvements
and is already hiring more staff and implementing strategies that are consistent with the
findings and recommendations in this report. The review reflects a point-in-time while
Oregon has continued to make progress.
This review does not address the specific strengths and challenges in financing the services
and systems accessed by Tribal communities in Oregon. The authors acknowledge the
complex government-to-government relationship between the State of Oregon and the
nine Federally Recognized Tribes in Oregon and the shared responsibility to ensure that
high quality, comprehensive, effective, and culturally relevant services and supports are
available to all children and youth in Oregon, including those who are American Indian or
Alaska Native. Furthermore, the authors recognize that health disparities exist across these
and other populations in Oregon,
2
as they do across the United States, underscoring the
importance of addressing these financing structures. However, while the recommendations
made in this report are expected to benefit American Indian and Alaska Native children,
youth, and families who are served through Medicaid in Oregon, specific recommendations
are not made to address the unique challenges facing these children and youth, as those
deserve their own focused analysis that leverages significant input from the Tribes and
communities.
Oregon’s Medicaid Structure
Access to health insurance is a clear priority for Medicaid, and OHA has worked to expand
access to the Oregon Health Plan (OHP, a.k.a. Medicaid). Oregon’s 1115 Waiver (discussed
below) provides two-year continuous enrollment for people ages six and up even if their
eligibility status changes
3
and made Oregon the first state in the U.S. to allow children who
enroll in Medicaid at birth to remain enrolled until age six.
4
Oregon was the third state in
the U.S. to request federal approval to provide free health care for adults at 138-200% of
the poverty level.
4
As of December 2023, approximately 36% of Oregon residents
(1,508,111)
5
were enrolled in Medicaid, while 60% of all children (ages 0-18; n=496,271) in
Oregon were enrolled in Medicaid.
6
When individuals are enrolled in OHP, they receive fee-for-service (FFS) or “Open-Card”
eligibility. Most people are then required to be enrolled in a CCO to access services covered
2
CCO Metrics Program (2023).
CCO Metrics Performance Dashboard
. Interactive display accessed
[12/10/2023]. Portland, OR: Oregon Health Authority.
https://visualdata.dhsoha.state.or.us/t/OHA/views/CCOPerformanceMetrics/welcome
3
Oregon Health Authority. (n.d.).
What’s Changing in the 2022-2027 1115 Demonstration Waiver.
Available from the OHA website: https://www.oregon.gov/oha/hsd/medicaid-
policy/pages/changes.aspx.
4
Templeton, A. (2023).
Oregon becomes 3
rd
in nation to seek federal approval for a basic health
program.
Available from Oregon Public Broadcasting:
https://www.opb.org/article/2023/09/12/oregon-basic-health-plan-insurance-doctor-authority-
affordable-care-act/.
5
Oregon Health Authority. (2023). Medicaid Monthly Population Report for Oregon. [January 17, 2024].
Available from the OHA website:
https://app.powerbigov.us/view?r=eyJrIjoiMTRhMmNhZDktYzY4OS00MzIxLTg4NTAtNjc4NmVlNjA1NzI
4IiwidCI6IjY1OGU2M2U4LThkMzktNDk5Yy04ZjQ4LTEzYWRjOTQ1MmY0YyJ9.
6
Calculated using the U.S. Census Bureau’s QuickFacts on Oregon, with population estimates for July 1,
2023 (n=4,233,358 for total population, n=833,972 children 0-18). Available from
https://www.census.gov/quickfacts/OR.

5
by OHP. There are sixteen CCOs in Oregon, with some CCOs overlapping coverage across
counties (see map below). There are some individuals who are not automatically enrolled
in a CCO:
• Individuals with major medical insurance (Medicaid is a secondary health insurance);
• Individuals who are American Indian or Alaska Native and choose not to enroll;
• Individuals in their last three months of pregnancy who choose to stay with their
current provider until giving birth; and
• Individuals approved for temporary FFS coverage.
7
Figure 1: Map of CCOs (2020) from the Oregon Health Authority
8
In November 2023, 8.3% (120,905) of individuals in Oregon enrolled in the OHP were
receiving FFS or Open-Card mental health services, meaning that they were not receiving
behavioral health services through their CCO.
9
This percentage is similar for children: 8.7%
7
Oregon Health Authority. (n.d.)
Who Covers Your Care?
Available from the OHA website:
https://www.oregon.gov/oha/HSD/OHP/Pages/Care.aspx.
8
Oregon Health Authority. (2020).
Coordinated Care Organization 2.0 Service Areas.
Available from the
Oregon Department of Human Services website:
https://sharedsystems.dhsoha.state.or.us/DHSForms/Served/le8116.pdf
9
Oregon Health Authority. (2023).
CCO Totals by County for Mental Health, OHP & CAK/HOP, Nov
2023.
Retrieved from:
https://app.powerbigov.us/view?r=eyJrIjoiMTRhMmNhZDktYzY4OS00MzIxLTg4NTAtNjc4NmVlNjA1NzI
4IiwidCI6IjY1OGU2M2U4LThkMzktNDk5Yy04ZjQ4LTEzYWRjOTQ1MmY0YyJ9&pageName=ReportSectio
n726184bb48f86b1a99c4

6
(43,373) of children ages 0 through 18 were enrolled to receive Open-Card mental health
services in November 2023.
10
When individuals in Oregon receive medical services through
the Open-Card (FFS) system, they may still receive dental and behavioral health services
through the CCO. The same situation applies for individuals receiving dental services
through the Open-Card system. However, individuals receiving behavioral health services
through the Open-Card system must receive all of their services through the Open-Card
system. Temporary Open-Card coverage is approved for 6-12 months, with the ability to
receive authorization to extend temporary coverage. After the temporary coverage lapses,
the individual is (re)enrolled in the local CCO.
11
OHA contracts with Comagine to support its Open-Card mental health system, including
providing utilization management (UM) for Open-Card practices. Comagine provides the
UM functions for youth ages 5-17 who access services in a psychiatric residential treatment
facility (PRTF) or Behavioral Rehabilitation Services (BRS); conducts the certificate of need
(CON) process for youth through ages 17 seeking access to PRTF; and provides UM tasks
for youth ages 18-22 (and over 64) seeking services at the Oregon State Hospital.
Comagine is also the contracted independent and qualified agent for services and settings
in the approved 1915(i) Home and Community-Based Services (HCBS) State Plan Option
and other mental health residential settings for adults.
Health equity is a core value of OHA and Oregon has established a strategic goal of
eliminating health inequities by 2030. Almost half of all OHP enrollees (children and adults)
are White (47%), with the next largest racial or ethnic demographic listed as
“other/unknown.” Fourteen percent (14%) of enrollees are Hispanic or Latino and all other
racial or ethnic populations comprise less than 5% each of the total OHP enrollee
population.
5
People who are White are a smaller percentage of OHP enrollees than would
be expected based on the total population of Oregon (86% White alone; 73.5% White
alone, not Hispanic or Latino)
.6
In 2022, a greater proportion of children and youth (0-25)
enrolled in OHP received behavioral health services than would be expected based on
population, while Hispanic or Latino/a, Black or African American, and American Indian
and Alaska Native youth all received disproportionately fewer behavioral health services
compared to the overall population.
12
According to the Annie E. Casey Foundation’s
Kids Count
13
, Oregon ranks 26
th
in the U.S.
for overall child well-being but 7
th
in the U.S. for children’s health (a ranking based on rates
of low birth-weight babies, children without health insurance, child and teen deaths, and
childhood obesity). However, the data, which are not specific to behavioral health, show
racial and ethnic disparities for low birthweight babies, with Black or African American,
American Indian, Asian and Pacific Islander, Latino, and children of two or more races all
10
Oregon Health Authority. (2023).
Eligibility by Age Groups for Mental Health, OHP & CAK/HOP, Nov
2023, All Counties
. Retrieved from
https://app.powerbigov.us/view?r=eyJrIjoiMTRhMmNhZDktYzY4OS00MzIxLTg4NTAtNjc4NmVlNjA1NzI
4IiwidCI6IjY1OGU2M2U4LThkMzktNDk5Yy04ZjQ4LTEzYWRjOTQ1MmY0YyJ9&pageName=ReportSectio
n4f305eee24d2c830b04a
11
Oregon Health Authority. (n.d.)
Asking for Fee-for-Service Oregon Health Plan (OHP) Coverage.
Available from the OHA website: https://www.oregon.gov/oha/HSD/OHP/Pages/FFS.aspx
12
OHA. (2023).
Child and Family Behavioral Health Performance Indicators.
Available from
https://www.oregon.gov/oha/HSD/BH-Child-
Family/Documents/Performance%20Indicators%20Report_Apr2023.pdf.
13
Annie E. Casey Foundation. (2024).
2023 Kids Count Data Book Interactive.
Available from
https://www.aecf.org/resources/2023-kids-count-data-book
.

7
having higher percentages of low birthweights than non-Hispanic white children. These
disparities are less present for the measure of children without health insurance, with Black
or African American children having the lowest percentage of uninsured children (1%) in
Oregon. However, American Indian and Latino children had higher percentages than other
races and ethnicities, at 4% and 5% respectively, a statistic that aligns with national data.
14
The 2023 Six Month Report from the OHA Ombuds Program
15
observed that finding local
mental health providers that offer culturally and linguistically aligned services is very
challenging and that there are potentially disparate outcomes for individuals who prefer a
language other than or do not speak English and have been traditionally excluded from
Medicaid and other population analyses. Additionally, children participating in Healthier
Oregon
16
(with most enrollees speaking English less than very well) are less likely to access
mental health assessments and mental health therapies.
17
They also found that children
who are Black or African American are overrepresented among the youth who experienced
Emergency Department Boarding compared to their proportion of the population.
It is particularly important for OHA and its sister agencies to collect data on race and
ethnicity, as discussed throughout this report, and use those data along with input and
feedback from youth, families, and partners, to ensure equitable access to effective
services and supports across Oregon. A focus on children, including those involved with
child welfare and juvenile justice systems (populations more likely to disproportionately
involved families of Color), will position Oregon to be successful in meeting its goals of
health equity across populations.
18
Findings & Recommendations
The document reviews and meetings with partners identified themes spanning service
array, eligibility, and access (inclusive of workforce capacity) and contracting language,
structures, and accountability (inclusive of oversight and performance measurement). The
themes overlap across populations, structures, and services but have interwoven
challenges and opportunities. There was a recurring theme of the balance of
14
Nationally, in 2021, 8.5% of children were born at a low birthweight. There are national disparities existing
across races and ethnicities that are consistent with Oregon’s data: 14.1% of Black or African American
babies were born low birthweight nationally. Oregon’s rates of uninsured children are lower than the
national average of 5%, although the disparities mirror national disparities that show higher percentages
of uninsured children who are American Indian or Latino.
15
OHA. (2023).
Ombuds Program 2023 Six Month Report.
Available from
https://www.oregon.gov/oha/ERD/OmbudsProgram/OHA%20Ombuds%20Six%20Month%20Report_Fi
nal.pdf
16
In 2021, House Bill 3352 established a program called “Cover All People,” which is now known as
“Healthier Oregon.” This program enables individuals to enroll in OHP and receive full OHP benefits if
they live in Oregon and meet income and other criteria, without consideration of their
immigration/citizenship status. (See
https://www.oregon.gov/oha/hsd/ohp/pages/healthier-
oregon.aspx.)
17
This analysis did not explore whether this is an issue of access, awareness, stigma, or another reason.
The authors recognize that the Healthier Oregon Program was expanded to include the broader
population in 2023, without consideration for immigration or citizenship status, and these data warrant
further analysis to identify opportunities to support access to care.
18
Like many states, children in Oregon who are Black, American Indian, or more than one race are more
likely to enter the child welfare system than would be expected based on their proportion in the general
population, with disproportionality index values of 1.65, 3.04, and 1.71, respectively. Source: Puzzanchera,
C., Zeigler, M., Taylor, M., Kang, W. and Smith, J. (2023). Disproportionality Rates for Children of Color in
Foster Care Dashboard. National Council of Juvenile and Family Court Judges. Available from
https://ncjj.org/AFCARS/Disproportionality_Dashboard.asp?selState=Oregon&selDisplay=1.

8
standardization versus regionalization and customization by CCO. It is clear that Medicaid’s
goal is for the OHP enrollees to experience the Medicaid system as seamless, even while
OHA weaves together numerous authorities and mechanisms. However, as discussed
below, the contracting language and associated structures and accountability mechanisms
(or lack of such) impact the service array. Similarly, lack of clarity regarding the existing
service array and its accessibility lead to challenges and confusion in contracting, limits in
access, and reduced accountability and oversight.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT) Benefit
Federal Medicaid law recognizes the unique needs of children by requiring the delivery of
comprehensive services to all Medicaid beneficiaries under the age of 21 through provisions
in the law known as Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
benefit.
19
Coverage requirements for children under Medicaid are more robust than those
that apply to Medicaid-enrolled adults. While EPSDT emphasizes screening and early
detection, it also includes a broad mandate related to treatment. The objective—and legal
requirement—is for children to get access to all needed services when they need it. The
scope of services offered to children under Medicaid is important for all children’s health,
but particularly for children with behavioral health needs.
20
EPSDT is a critical strategy to
address health equity by providing the screening, treatment, and services that an individual
needs.
Prior to January 1, 2023, Oregon maintained a federal waiver of EPSDT and utilized its
Prioritized List of Health Services. However, effective January 1, 2023, EPSDT benefits are
provided to all OHP members under age 21. OHA and CCOs must “cover all medically
necessary and medically appropriate services for OHP members under age 21, regardless
of placement on the Prioritized List of Health Services.”
21
This is a significant shift in
coverage and, given the importance of EPSDT in supporting access to comprehensive
services, our recommendations are grounded in supporting Oregon to fulfill
implementation of the EPSDT requirements.
22
Under EPSDT, every state must provide all “medically necessary services” that could be
covered within the categories of mandatory and optional Medicaid services listed in
Section 1905(a) of the Social Security Act, regardless of whether the services are identified
in a state’s Medicaid State Plan or available to adults enrolled in the program.
19,20
This
19
Centers for Medicare & Medicaid Services (CMS). (n.d.).
Early and Periodic Screening, Diagnostic, and
Treatment.
Available from CMS: https://www.medicaid.gov/medicaid/benefits/early-and-periodic-
screening-diagnostic-and-treatment/index.html.
20
Tsai, D. (2022).
CMCS Informational Bulletin: Leveraging Medicaid, CHIP, and Other Federal Programs
in the Delivery of Behavioral Health Services for Children and Youth.
Available from CMS:
https://www.medicaid.gov/sites/default/files/2022-08/bhccib08182022.pdf
21
Oregon Health Authority. (n.d.).
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
Program.
Available from OHA: https://www.oregon.gov/oha/hsd/ohp/pages/epsdt.aspx
22
Note:
While Oregon’s EPSDT benefit was effective 1/1/23, additional guidance, updates, and guides
have been issued since that time. The permanent EPSDT program rules went into effect on 1/1/24,
although CCOs and OHA were under guidance and program requirements that align with these
permanent rules since 1/1/23. OHA also is hiring additional staff to support implementation, policy, and
data analytics associated with EPSDT. The authors have done our best to ensure that the findings in this
document align with the most recent guidance, rules, and materials issued by OHA. However, readers
are encouraged to review the most recent publications and materials related to EPSDT in Oregon and
recognize that these findings reflect a point-in-time review of a dynamic and ongoing process. Oregon
maintains a document with a list of updated documents, which is available online:
https://www.oregon.gov/oha/HSD/OHP/Tools/EPSDT-Guidance-Change-Log.pdf
9
includes physical and behavioral health services as well as long-term services and supports.
States and Medicaid managed care organizations (MCOs) can require prior authorization
for particular services to safeguard against unnecessary use of services, but prior
authorization cannot result in a delay or denial of medically necessary services. Notably,
for children, states and MCOs may not impose hard or fixed limits on specific services (e.g.,
no more than 30 units of a service). If the service or device is medically necessary, it must
be provided.
20,23
While all services—for adults as well as children—must be “medically
necessary” for the individual for that service to be covered, Medicaid has a medical
necessity standard that is unique to children. The EPSDT pediatric medical necessity
definition includes a focus on correcting or ameliorating defects and physical and mental
illnesses and conditions.
23
EPSDT establishes a national pediatric standard of medical
necessity that all states must follow to address children’s unique physical and behavioral
health needs.
As noted above, as part of Oregon’s federal April 2023 approval for its 1115 Waiver,
beginning January 1, 2023, all section 1905(a) services that are determined necessary to
correct or ameliorate physical and mental illnesses and conditions, regardless of whether
they are included in the state plan, are covered for children under 21, in accordance with
the EPSDT definition at section 1905(r) of the Act. Oregon’s definition of EPSDT Medical
Necessity includes a requirement that the service is also “EPSDT Medically Appropriate.”
24
Covered Services
While services for children under 21 determined to be necessary to correct or ameliorate a
behavioral health condition now are covered under EPSDT, regardless of inclusion in the
State Plan, Oregon does not have a list of such services for families, providers, CCOs, and
government partners to use as a guide. The Oregon EPSDT FAQ’s question about which
services are included in the EPSDT benefit is answered: “EPSDT is a comprehensive child
and youth health care benefit for OHP members ages birth to 21. Medically necessary and
medically appropriate physical, dental, behavioral health, and pharmacy benefits are
covered through EPSDT. This includes screenings, checkups, tests and follow-up care,
including for vision, hearing and oral/dental health.”
It is important for families and providers to understand that all medically necessary and
medically appropriate services are covered. However, a comprehensive list is important to
establish baselines of service array, identify gaps in services, and determine network
adequacy. One of the tasks of this analysis was to determine the missing components from
the CMS-approved authorities and make recommendations associated with improving
access to timely, quality, trauma-responsive, and individualized services and interventions.
Comprehensive and actionable recommendations cannot be made without a list of all
covered services.
The website guiding individuals and families in the selection of a CCO states, “Except for
extra services and pharmacies, all CCOs offer the same OHP benefits…Some CCOs provide
extra services. These are items or services to support your health or manage a condition.
23
CMS. (2014).
EPSDT-A Guide for States: Coverage in the Medicaid Benefit for Children and
Adolescents.
Available form CMS: https://www.medicaid.gov/sites/default/files/2019-
12/epsdt_coverage_guide.pdf
24
Oregon Administrative Rule, Chapter 410, Division 151.
Early and Periodic Screening, Diagnostic and
Treatment. Available from
https://secure.sos.state.or.us/oard/displayDivisionRules.action?selectedDivision=8155.

10
Some extra services are available to all members. Others are available on a case-by-case
basis or by special request. You can contact each CCO for a full list of services and how to
access them.”
25
It is unclear how much variability exists across CCOs and what each
member can expect to receive from all CCOs versus extra services provided.
We recognize that Oregon has sought to move away from its historic use of lists in its
efforts to message that the State is responsible for EPSDT. However, developing and
maintaining a list of minimum covered services is not a concern when it establishes a
strong, evidence-informed foundation for the execution of EPSDT. A problem arises when
states rely on a list of services as a cap or ceiling, not when the list serves as a baseline and
minimum standard of expected services. Such a list could start with services previously
included in the Prioritized List of Services, the Behavioral Health Fee Schedule under the
Oregon Health Plan Fee-for-Service, and the services the CCOs are required to provide
under contract. Oregon must continue to reinforce that this list is not offered as a coverage
guide to what is available, which contradicts EPSDT, but as a tool to convey the range of
services that are important to consider.
All children and youth with behavioral health service needs, regardless of CCO or region,
should have access to providers who offer individual, group and family therapies and
psychiatric services; peer support; intensive in-home services; and mobile response and
stabilization services. They also should have access to intensive care coordination using
Wrapround, respite care, and culturally and linguistically responsive services and evidence-
based and promising practices. These services have been demonstrated to be effective in
decreasing the need for more restrictive and costly services such as inpatient
hospitalization and psychiatric residential treatment facilities.
26
Implementation Support
Oregon has developed numerous documents regarding changes to its EPSDT program,
including a CCO guidance document, EPSDT Provider Guide, provider communications,
and related regulatory guidance. These communications are clear, concise, easy to follow,
and anticipate the common questions and challenges to transitioning to EPSDT. We
commend Oregon for its clarity in these documents. However, Oregon needs to take
additional steps to ensure comprehensive
implementation
of EPSDT.
25
Oregon Health Authority. (2022).
CCO Plans.
Available from the OHA website:
https://www.oregon.gov/OHA/HSD/OHP/Pages/CCO-Plans.aspx
26
See Mann, C. & Hyde, P. (2013).
Coverage of Behavioral Health Services for Children, Youth, and Young
Adults with Significant Mental Health Conditions.
Available from the Medicaid website:
https://www.medicaid.gov/sites/default/files/federal-policy-guidance/downloads/CIB-05-07-2013.pdf;
ICF International. (2013).
Avoided costs of system of care-related outcomes: 2005- 2010 communities
funded by the federal Children’s Mental Health Initiative
. Atlanta, GA; Stroul, B. A., Goldman, S. K., Pires,
S. A., & Manteuffel, B. (2012).
Expanding the system of care approach: Improving the lives of children,
youth, and families
. Washington, DC: Georgetown University Center for Child and Human Development,
National Technical Assistance Center for Children’s Mental Health.
https://gucchd.georgetown.edu/products/SOC%20Results%205-7-12.pdf; Urdapilleta, O., Kim, G., Wang,
Y., Howard, J., Varghese, R., Waterman, G., et al. (2012).
National evaluation of the Medicaid
demonstration home and community-based alternatives to psychiatric residential treatment facilities,
final evaluation report
. Centers for Medicare & Medicaid Services.
https://www.medicaid.gov/sites/default/files/2019-12/cba-evaluation-final.pdf ; Stroul, B. A., Pires, S. A.,
Boyce, S., Krivelyova, A., Walrath, C. (2015).
Return on Investment in Systems of Care for Children With
Behavioral Health Challenges
. Washington, DC: Georgetown University Center for Child and Human
Development, National Technical Assistance Center for Children’s Mental Health.
https://gucchd.georgetown.edu/products/SOCReturnOnInvestmentIssueBrief.pdf

11
States often struggle to fulfill their obligations in EPSDT in several areas. This includes a
lack of training on EPSDT for pediatric providers and MCOs and limited or inaccessible
consumer information and education on the services available to Medicaid-enrolled
children. It can also include improper application of service limits and exclusions as well as
a nontransparent medical necessity determination process by MCOs (including CCOs),
which lead to improper denials of care. States struggle with a shortage of pediatric
specialists generally, and many lack specific network adequacy requirements for pediatric
specialists in some Medicaid managed care contracts. Often there is limited state
engagement with families and pediatric providers on systemic issues and limited state
monitoring and oversight aimed at preventing, tracking and remediating access challenges
for Medicaid-enrolled children with special healthcare needs.
27
As Oregon transitions from its use of a prioritized list of services to meeting the full national
standard for medical necessity under EPSDT, Oregon will need to monitor its efforts across
these various areas and be prepared to provide operational and policy support and
oversight. As noted above, Oregon will want to outline a pathway for providers and families
to request services that are not listed in the State Plan and will want to identify specific
performance metrics to collect and monitor (initial recommended metrics are listed
below). These metrics should be stratified by demographics, geographical area, and CCO
coverage and incorporated into continuous quality improvement (CQI) processes that
include meaningful family, youth, provider, and public agency participation. This includes
monitoring EPSDT training penetration rates across primary care and pediatric medical
providers and across sub-specialties of behavioral health providers in order to ensure
targeted engagement outreach and engagement for training.
Finally, the Bipartisan Safer Communities Act of 2022 (P.L. 117-159) included EPSDT
provisions requiring CMS to review state implementation of EPSDT, identify any gaps in
state implementation, and provide technical assistance to address these gaps. CMS will be
issuing guidance to states and a report to Congress in 2024, with reports due every five
years thereafter. As such, Oregon has initiated, or will shortly be initiating, discussion and
a review with CMS regarding the state’s EPSDT implementation. This will provide Oregon
with an opportunity to highlight its EPSDT documentation and policies and identify
opportunities to strengthen implementation to address challenges and gaps in coverage.
Recommendations:
1) Create a list of all covered specialty behavioral health services for children under 21
that are available under the State Plan to serve as a guide to families, providers, and
CCOs, emphasizing that this list is a minimum floor and not a ceiling on services.
The list of services should explicitly state the required services provided by all CCOs.
2) Develop documentation outlining a pathway to requesting services not listed in the
State Plan.
3) Engage families and youth in reviewing and adjusting the minimum list of covered
services and pathway, including methods for reaching families and youth and
additional materials or messages that could be further developed. Families and
youth should have opportunities to provide meaningful feedback on the design,
27
Mann, C., Serafi,K., Eder, J., & O’Connor, K.. (2019).
Keeping Medicaid’s Promise: Strengthening Access
to Services for Children with Special Healthcare Needs.
Available from Manatt:
https://www.manatt.com/Manatt/media/Documents/FINAL-Keeping-Medicaid_s-Promise-Issue-Brief-
10-01-19.pdf
12
implementation, and effectiveness of EPSDT and how to ensure that the minimum
list reflects provider capacity, not service coverage allowability.
4) Work with provider associations and groups to support implementation of EPSDT
and ensure understanding of the documents and tools provided.
5) Enhance CQI processes to include specific quality performance metrics related to
EPSDT; collection, analysis, and use of these data to adjust statutory, regulatory, and
contractual standards and requirements; and meaningful opportunities for
engagement and feedback. Monitor implementation across metrics below to ensure
that EPSDT is being implemented as intended.
a. Metrics should be stratified by demographics, geographical area, and CCO
coverage and incorporated into the CQI process.
b. Implement oversight mechanisms of the CCOs to include:
i. Ongoing and/or annual re-training on EPSDT;
ii. Review of who is and is not making EPSDT requests to support
focused training and technical assistance;
iii. Ensuring that no service limits or exclusions are being implemented
inconsistent with EPSDT.
c. Recommended metrics include:
i. Total number of primary care and pediatric providers and the
penetration rate of those trained with a minimum baseline established;
ii. Total number of behavioral health providers serving pediatric
populations and the penetration rate of those trained training
participation, with a minimum baseline established;
iii. The number and type of requests for behavioral health services under
EPSDT and changes to those requests over time;
iv. Questions and issues identified by families, youth, and providers for
clarity or resolution; and,
v. Achievement of network adequacy standards for specialty behavioral
health services for children and youth, by service type (discussed
further below).
Expanding Access and Support through the 1115 Waiver
Oregon received approval for a specific benefit to include transition-aged individuals who
are between ages 19 and 26, have income up to 300 percent FPL, and meet certain
eligibility criteria, including “have a serious emotional disturbance or serious mental health
issue” among the population of Youth with Special Health Care Needs (YSHCN). We
commend Oregon for this important addition addressing the needs of young adults. While
technically adults, persons aged 19-26 are still developing and differ from older adults
emotionally, socially, and cognitively. These youth will benefit from Oregon’s provision
that, “Beginning January 1, 2023, for all children younger than 21 years old, and YSHCN, all
section 1905(a) services that are determined necessary to correct or ameliorate physical
and mental illnesses and conditions, regardless of whether they are included in the state
plan, in accordance with the EPSDT definition at section 1905(r) of the Act.”
Additionally, Oregon received approval for significant investment in with its coverage of
Health-Related Social Needs (HRSN), including for the YSHCN population, youth
transitioning from institutions for mental diseases; youth released from incarceration,
including prisons, local correctional facilities, and tribal correctional facilities; and youth
involved in the child welfare system, including youth transitioning out of foster care. These
services may include housing supports; nutrition supports; and case management,
outreach and education, including linkage to other state and federal benefit programs.
13
Services to address HRSN have been shown to be effective in improving health outcomes,
particularly for vulnerable populations.
28
Oregon is only one of six states with federally
approved 1115 waivers addressing HRSN.
Recommendations:
1) Provide training, coaching, and implementation support to providers delivering
services to young adults ages 18-26 to ensure that they have the necessary expertise
and knowledge of this unique developmental stage of young adulthood.
2) Develop, collect, and analyze metrics, stratified by the above-recommended
demographics, reported by each of the prioritized populations and total overall.
a. Data should include the HRSN penetration rate for each of the prioritized
youth populations, with expectations that the CCOs will engage in outreach
and training to providers serving these populations to improve HRSN
penetration rates.
b. Collect and report on provider network information that delineates providers
with expertise in emerging adulthood, much like is tracked for those with
expertise in early childhood and make this information available to young
adults and CCOs.
3) As part of the Section 5121 requirements discussed below, Oregon will need to
develop a plan for certain screening and diagnostic services for youth in juvenile or
correctional facilities. Given Oregon’s plan to facilitate HRSNs, it will be important
that the protocol to access HRSNs through the CCOs align with Oregon’s Section
5121 plan.
4) As one of the first states providing services to address HRSN through an 1115 waiver,
Oregon may want to engage, formally or informally, with peers in Arizona, Arkansas,
Massachusetts, New Jersey, and Washington to share best practices and lessons
learned. Oregon is applying for the Center for Health Care Strategies’ Medicaid
Health-Related Social Needs Implementation Learning Series; regardless of
acceptance, Oregon should track the work and findings of this Series.
5) Oregon should facilitate a learning collaborative with families, youth, and relevant
state and local partners to review the data, identify areas for improvement, and
support implementation activities.
Child Welfare & Juvenile Justice-Involved Children
Children involved with child welfare and juvenile justice systems require additional
coordination and intentional system design activities to meet their needs across life
domains.
29
Documents reviewed and partners interviewed identified particular challenges
experienced by youth and families involved in these public systems. In particular, they
noted that, like all youth and families, they risk losing access to their providers when they
28
Whitman, A., De Lew, N., Chappel, A., Aysola, V., Zuckerman, R., & Sommers, B.D. (2022).
Addressing
social determinants of health: Examples of successful evidence-based strategies and current federal
efforts.
Available from the Assistant Secretary for Planning and Evaluation:
https://aspe.hhs.gov/sites/default/files/documents/e2b650cd64cf84aae8ff0fae7474af82/SDOH-
Evidence-Review.pdf
29
See Harburger, D.S., Pires, S.A., & Schober, M.A. (2022). Sustainable financing to support children &
families: Medicaid and other fiscal, funding, and financing challenges and opportunities. In R. Denby-
Brinson & C. Ingram (Eds.),
Child and family-serving systems: A compendium of policy and practice
(Volume I: Evolution of protecting, strengthening, and sustaining children and families).
CWLA Press.

14
move. Continuity of care is particularly important for these children and care improves
when there is coordination at the system and individual levels.
30
Oregon, like many states, is experiencing a challenge in finding out-of-home placements
for children in foster care with complex needs. The existing foster homes and congregate
care placements are insufficient, leading to children being placed in temporary lodging.
Most children and youth can be served in a family-based setting if there are sufficient and
intensive enough services provided. However, this requires intensive home- and
community-based services to be available across the state, services to be able to be
provided in the home, and caregivers to be supported through services such as mobile
response and stabilization services, care coordination, respite care, and peer support.
Oregon’s Family First Prevention Services Act (FFPSA) Prevention Plan identified four
evidence-based practices that will be provided to eligible children and families with a goal
of preventing out-of-home placement. The services were selected to increase Oregon’s
capacity to better serve children ages 0-5, children ages 6-12, children whose caregivers
have SUDs, children whose parents have I/DD service needs, and African American,
American Indian/Alaska Native, and Latinx children and families. The four initial services
(Parent Child Interactional Therapy, Functional Family Therapy, Motivational Interviewing,
and Parents as Teachers) are being implemented across the state, with a goal of expanding
eligible services to include a range of interventions, including Oregon’s Tribal Best
Practices.
Under section 5121 of the Consolidated Appropriations Act, 2023 (P.L. 117-328), State
Medicaid Agencies (SMA) and Children’s Health Insurance Programs are required to have
developed a plan by January 2025 that will require the state to:
• Provide certain screenings and diagnostic services (including behavioral health
screening and assessments) in accordance with EPSDT requirements to eligible
juvenile youth in “public institutions” (e.g., juvenile justice facilities) 30 days prior to
the youth’s release from the facility; and,
• Provide targeted case management (TCM) services that include referrals and
linkage to aftercare services and supports.
The Consolidated Appropriations Act makes Medicaid federal financial participation (FFP)
available to SMAs for providing these services (using regular state match). In addition,
Section 5121 aligns CHIP rules with existing Medicaid rules regarding suspension rather than
termination of coverage while a child is an inmate of a public institution and related
requirements regarding redeterminations of coverage.
Under section 5122 of the Consolidated Appropriations Act, 2023 states will have the
option to provide Medicaid and CHIP coverage to juvenile youth in public institutions
during the initial period pending disposition of charges. This optional opportunity will be
available beginning in January 2025 and would likely require a state to submit an 1115
waiver to waive the provision that prohibits FFP for medical or behavioral health care to
30
Substance Abuse and Mental Health Services Administration (2019).
Intensive Care Coordination for
Children and Youth with Complex Mental and Substance Use Disorders: State and Community Profiles.
(SAMHSA Publication No. PEP19-04-01-001). Available from the SAMHSA website:
https://store.samhsa.gov/sites/default/files/intensive-care-coordination-children-youth-complex-
mental-substance-use-disorders-pep19-04-01-001.pdf and Agency for Healthcare Research and Quality.
(2018).
Care coordination.
Available from the AHRQ website:
https://www.ahrq.gov/ncepcr/care/coordination.html

15
inmates of a public institution. This is consistent with the recent guidance CMS released
regarding reentry for individuals in correctional facilities.
31
Recommendations:
1) As part of CCO contracts, require CCOs to establish Memoranda of Understanding
(MOU) with local child welfare, juvenile justice, and developmental disabilities
offices to improve coordination and communication, support children and families
to maintain continuity of care with providers, and ensure that both the CCOs and
the local agencies have a shared understanding of roles, responsibilities, and
expectations.
2) OHA should leverage Federal Financial Participation (FFP) under Medicaid to
support a children’s behavioral health liaison between the child welfare agency and
the CCOs to support improved coordination and problem-solving.
3) Child welfare should track the implementation of FFPSA services and identify
whether these services are being provided in addition to or instead of children’s
mental health services through the CCOs. They should determine if the FFPSA
services are supporting children and families to remain together in their own homes
and, if services are effective, explore coverage of them under the Medicaid State
Plan for Medicaid-eligible families.
4) OHA and DHS should jointly provide training and individualized coaching to child
welfare and Medicaid leaders and managers, as well as to local child welfare workers
and supervisors and CCO staff to support moving children out of temporary lodging
and into the most effective, least restrictive setting. DHS, in collaboration with OHA,
families, youth, and other partners, should:
a. Establish best practice standards, expectations, and guidelines for child
welfare workers in making individualized recommendations for out-of-home
placements for children who are unable to remain in their own homes,
prioritizing kin and fictive kin and other family-based settings with additional
supports as needed.
b. Integrate the CANS into care planning and use a standardized tool to support
teams—including youth and families—to identify goals and action steps,
including timelines for discharging from hospitals and congregate care
settings and services needed to support a successful transition.
c. Develop a pathway to review and approve requests for individualized
services and supports that will enable children to be served in a family-based
setting (e.g., one-on-one supports in the home from 3-6pm on school days
for a child that struggles during this time or access to an expressive therapy
or healing practice that is culturally responsive to the family’s needs).
d. Establish performance measures and a CQI process for congregate care
placements for children involved with child welfare and juvenile justice,
looking at the clinical and behavioral health services provided, the outcomes
of the children in the programs, the ratios of direct care staff, the length of
stay in the program, and the discharge location (home, family-based setting,
or other congregate care setting). Data should be examined by demographic
characteristics, geographic location, and CCO enrollment.
5) In the plan in response to Section 5121, Oregon should ensure it aligns its screening
and assessment pathway to ensure a consistent approach for all individuals. It will
be important to develop a pathway not only with juvenile justice facilities, but with
31
See https://ccf.georgetown.edu/2023/01/05/consolidated-appropriations-act-2023-medicaid-and-
chip-provisions-explained/ for an explanation of provisions of the Act.
16
adult correctional facilities as well, given that youth and emerging adults up to age
26 may be in adult correctional facilities.
6) Taking note of high trauma rates in this population, OHA should partner with other
child- and family-serving agencies to identify avenues for prevention, as well as
expanding early evidence-based treatment; these efforts should be incorporated
into IIBHT programs.
7) Given the high percentage of youth in foster care in IIBHT, ODHS should be invited
to regular reviews of IIBHT to ensure that the needs of this population are being
understood and addressed in IIBHT programs.
8) OHA should ensure that the juvenile justice and child welfare agencies are part of
the implementation of the YSHCN and HRSN provisions of the 1115 Waiver to support
alignment and consistency across systems/payers, coordinate policies and
procedures to leverage services and supports for the shared population of youth,
and ensure seamless access to services uniquely available to this population to
achieve shared outcomes (e.g., Foster Care Transition Funds, Independent Living
Program Provider Aftercare Support Services, Family Unification Program-You t h
vouchers, Foster Youth to Independence (FYI), Chafee Education & Training Grants).
Additional Managed Care Oversight & Regional Design Findings
CCOs serve as a vehicle for Oregon to achieve its goals of increasing access to health care,
improving the quality of care and access to preventive services, and containing the cost of
health care. The CCO framework serves as a mechanism to support customization to the
unique geographic, racial, ethnic, and cultural needs of the population living in the CCO’s
geographic coverage areas. However, with customization comes the need to be clear on
which issues, processes, and expectations require standardization.
Sometimes, it is the outcome that is standardized, thus allowing for a customized regional
approach to meet that outcome. However, in children’s behavioral health, many of the
outcome metrics are influenced by factors not solely in control of a CCO or provider,
particularly because children are part of family units and needs span life domains for the
children and their families. In some instances, a relevant behavioral health metric is
measured too far from the point of service, cannot be attributed to any one service, or
varies based on the quality of the provider. As such, most states have had to rely on
process measures in addition to standard quality measures.
A core system of care value is that there is a clear locus of accountability for services and
outcomes with coordination across providers, settings, and domains. However, across
Oregon, there is a fragmentation and bifurcation of responsibilities, with everyone and no
one being accountable for providing high quality, timely, responsive, and effective services
and supports. Each CCO has a different pathway to care, which means that youth, families,
and providers have to navigate different access points and networks anytime the youth
moves to a different geographic area and has to change CCOs. In states with multiple
managed care plans with child beneficiaries enrolled (e.g., Massachusetts), state Medicaid
agencies have required use of common screening tools, a single assessment tool, and
access to the same benefit array across all their health plan partners.
Implementation of new standards, initiatives, or practices is challenging because of the
variability across the State, including regions that have multiple CCOs. Inconsistency in
medical necessity criteria, service authorizations, and utilization management approaches
leads to practice differences across providers and unduly burdens the State’s providers
that are paneled with multiple CCOs.

17
Oregon’s lack of standardized coding for billing makes it difficult to assess the penetration,
utilization, and expenditure rates for services across the state. Although the CCOs
document the services provided to a youth or family, if the codes were not part of the
original fee schedule, the CCOs may use their own codes. This makes it challenging to roll
up the data statewide for analysis and quality improvement.
Oregon is to be commended for strengthening its network adequacy standards (OAR 410-
141-3515) and expanding its capacity for data analytics in its CCO Operations Team.
However, the proposed network adequacy standards group all children’s behavioral health
providers, including for children with SED, into one category. There are numerous home-
and community-based behavioral health services that should be available to all children in
any state, and a requirement to have “mental health providers serving pediatrics” within a
particular distance or time is insufficient. We note that further delineation of medical
providers is included in Oregon’s approach, and we recommend that the state’s need to
assure certain medical categories of expertise are available should be the approach applied
to behavioral health categories of care. Currently, behavioral health itself is seen as a
specialty category to medical care vs as having its own essential sub-categories of
approaches that are essential to ensure are available. Grouping outpatient therapy with
intensive in home therapy implies that both equally can address the same type of issues
which is not true. However, a state knowing whether it has sufficient capacity to provide
outpatient therapy to youth and intensive in home for that smaller group of beneficiaries
in need is essential to ensuring EPSDT.
Finally, Oregon’s Behavioral Health Resource Networks (BHRNs) were designed to fill a
gap in the continuum of services and cover services not otherwise covered by Medicaid or
insurance. Established by Oregon voters in 2020 through Ballot Measure 110 and codified
by Senate Bill 755 (2021), by law, each Oregon county must have a BHRN and each BHRN
must provide screening and assessments for SUD use, low-barrier SUD treatment, housing,
harm reduction services, peer services, and supported employment. Statutory language
prohibits BHRNs from supplanting funds, so CCOs and insurance are the primary payer for
all BHRN services if they are reimbursable services. The BHRN provide services that are
not Medicaid billable, which might be provided by some CCOs as additional services.
Although all BHRNs must have a policy on how they will provide youth-specific services or
refer youth to community providers of those services, the vast majority of services
provided by BHRNs in Fiscal Year 2023 were provided to the adult population.
32
Recommendations:
1) In the new CCO contracts, Oregon should require that all CCOs use the same
medical necessity criteria, service authorization and utilization review criteria, billing
codes, and pathway to care. Oregon should consider standardizing reimbursement
rates for providers, as discussed below.
2) Network adequacy standards should be further delineated for children’s mental
health providers to ensure consistent access statewide to a minimum array of
services, including individual, group, and family therapies; peer support; intensive
in-home services; and mobile response and stabilization services.
32
Oregon Health Authority. (n.d.).
Measure 110: A Health-Based Approach to Addiction and Overdose.
Data dashboard accessed on 2/2/24.
https://app.powerbigov.us/view?r=eyJrIjoiODU1NDNlNzUtMDBkNy00NTM1LWE4NzgtNGEyNzQxYWY0
NTU2IiwidCI6IjY1OGU2M2U4LThkMzktNDk5Yy04ZjQ4LTEzYWRjOTQ1MmY0YyJ9.
18
3) Clarify the roles and responsibilities of the BHRN versus the CCOs and how they are
expected to interface and support children and adults.
4) In the 1115 Waiver, the CCOs are required to implement various governance and
organizational councils to guide their work. Recognizing that consumers are
specifically listed as participants, we recommend further delineation to ensure that
adult consumers, youth, and families are represented and have an opportunity for
meaningful participation.
State Plan Options to Support Youth with Behavioral Health & Co-
Occurring Intellectual & Developmental Disability (I/DD) Service Needs
Oregon is using multiple HCBS Medicaid authorities to address the needs of persons with
I/DD. These specific authorities include:
• The Behavioral ICF/IDD Model Waiver (1915(c) authority) which serves children, from
birth through age 17, who meet the ICF/ID level of care. These children, due to their
behavioral needs, require the specialized services provided through this HCBS
waiver in order to remain in or return to the family home. The critical goal of this
waiver is to assure that children who are at risk of entering an ICF/ID can live in the
family home and preserve a family's capacity to care for their child; and assure the
health and safety of the child within the family.
• Children’s HCBS Waiver (1915(c) authority) which provides home and community-
based services to children from birth through age 17 with I/DD service needs in 24-
hour residential settings (licensed community homes, developmental disability
foster homes) or in the child's family home, including child welfare foster care.
We found the benefits under these authorities to be well-defined and included a broad
benefit array addressing the various needs of persons with I/DD at different developmental
stages. Access to both waivers are limited by Oregon’s choice not to use institutional
income and resource rules for the medically needy. This seems inconsistent with Oregon’s
efforts to expand access to Medicaid across populations and may result in children having
difficulty accessing necessary services in their homes and communities and may result in
families accessing services through Voluntary Placement Agreements.
Our review did not include the notices to families and recipients, the training materials to
providers, and existing utilization and outcome data. As such, we highlight considerations
for improving access to diagnosis and treatment for children and youth with co-occurring
behavioral health and intellectual developmental disabilities; these issues may not be
present in Oregon but are elevated to assist Oregon in assessing its system and services.
Psychiatric and behavioral symptoms can be misattributed to and overshadowed by I/DD,
thereby reducing who is assessed and determined to have a behavioral health need and

19
impacting treatment approaches.
33,34,35
Behavioral health providers often are not trained
with the skills to engage, assess, and treat people with I/DD in treatment for co-occurring
needs, nor do they have the training and expertise to adapt treatment interventions to
meet the strengths and challenges of people with I/DD.
33,35
Across populations, access to
quality and effective treatment for individuals with co-occurring I/DD and mental health
disorders often is hampered by the “lack of a skilled workforce, diagnostic overshadowing,
and a failure to integrate services”(p.96).
36
Barriers to receiving effective diagnoses and
treatment may be more pronounced for populations of children and youth who display
offending behaviors, are People of Color, and/or have complex needs.
37
Additionally, in 2021, the American College of Medical Genetics and Genomics
recommended the use of exome and genome sequencing (ES/GS) as a first- or second-
line test in individuals with congenital anomalies onset prior to age 1 or developmental
delay or intellectual disability with onset prior to age 18.
38
Genetic sequencing can be an
important tool to improve psychosocial outcomes, provide prognosis and expected clinical
course, support youth and families in decision-making, refine treatment options, avoid
unnecessary and redundant testing, and identify associated medical risks.
39
However, it
should be noted that parents, caregivers, and youth may have concerns about genetic
testing, including potential harm resulting from the testing itself, how the findings are used,
and the ability to protect the information.
4041
Oregon’s
Prioritized List Guideline Note
states that coverage is provided related to the
diagnostic evaluation of individuals with I/DD, Autism Spectrum Disorder, or multiple
congenital anomalies. However, there are limitations provided in the guideline, including
only covering testing for children with ASD if it is accompanied by dysmorphic features
33
CAMH. (2023).
IDD-Diagnosing Psychiatric Disorders in People with IDD
. Available from the CAMH
website: https://www.camh.ca/en/professionals/treating-conditions-and-disorders/intellectual-and-
developmental-disabilities/idd---diagnosis/idd---diagnosing-psychiatric-disorders-in-people-with-idd.
34
NADD. (2022).
IDD/MI Diagnosis
. Available from the NADD website: https://thenadd.org/idd-mi-
diagnosis/.
35
Hogg Foundation for Mental Health. (2014).
Policy Recommendations: Addressing the Mental Health
and Wellness of Individuals with Intellectual Disabilities (IDD).
Available from
https://utw10282.utweb.utexas.edu/wp-content/uploads/2015/09/MH_IDD-Policy-Rec_0801141.pdf.
36
Whittle, E. L., Fisher, K. R., Reppermund, S., Lenroot, R., & Trollor, J. (2018). Barriers and Enablers to
Accessing Mental Health Services for People With Intellectual Disability: A Scoping Review.
Journal of
Mental Health Research in Intellectual Disabilities,
11(1), 69–102. doi: 10.1080/19315864.2017.1408724.
37
Sin, C., Francis, R. and Cook, C. (2010). Access to and experience of child and adolescent mental
health services: barriers to children and young people with learning disabilities and their families.
Mental
Health Review Journal
,
(15)
1. https://doi.org/10.5042/mhrj.2010.0199
38
Manickam, K., McClain, M.R., Demmer, L.A., Biswas, S., Kearney, H.M., Malinowski, J., Massingham, L.J.,
Miller, D., Yu, T.W., Hisama, F.M., & ACMG Board of Directors. (2021). Exome and genome sequencing for
pediatric patients with congenital anomalies or intellectual disability: an evidence-based clinical
guideline of the American College of Medical Genetics and Genomics (ACMG).
Genetics in Medicine,
(23)
. https://doi.org/10.1038/s41436-021-01242-6.
39
Sun, F., Oristaglio, J., Levy, S.E., Hakonarson, H., Sullivan, N., Fontanarosa, J., & Schoelles, K.M. (2015).
Genetic Testing for Developmental Disabilities, Intellectual Disability, and Autism Spectrum Disorder.
(Technical Briefs, No. 23). Available from:
https://www.ncbi.nlm.nih.gov/books/NBK304462/pdf/Bookshelf_NBK304462.pdf
40
Klitzman, R., Bezborodko, E., Chung, W.K., & Appelbaum, P.S. (2024). Parents’ views of benefits and
limitations of receiving genetic diagnosis for their offspring.
Child : Care, Health & Development
,
50
(1),
e13212-n/a. https://doi.org/10.1111/cch.13212 .
41
Harburger, D.S., Fields, S. & Bilik, L. (2024, April 24).
Medicaid Analysis Report Presentation.
Presentation to the Oregon Children’s System Advisory Council. Virtual meeting.
https://www.oregon.gov/oha/hsd/bh-child-family/pages/csac.aspx

20
including macro or microcephaly, congenital anomalies, or intellectual
disability/developmental delay.
42
Oregon is one of five states with a CMS-approved 1915(k) State Plan Amendment (SPA),
also known as the “Community First Choice Option.” This mechanism provides enhanced
federal matching payments to states for expenditures associated with providing home and
community-based attendant services and supports to eligible enrollees. Oregon’s K Plan
was approved in 2013 and provides services to individuals who are in an eligibility group
that includes Nursing Facility services or are below 150% of federal poverty level. The K
Plan services are available to children and youth who require the level of care provided in
a hospital, nursing facility, intermediate care facility for individuals with intellectual
disabilities (ICF/ID), or an institution providing psychiatric services for individuals under 21
using hospital level of care criteria. The K Plan states that “individuals who are receiving
medical assistance under the special home and community-based waiver eligibility group
defined at section 1902(a)(10)(A)(ii)(VI) of the Act must continue to meet all 1915(c)
requirements and must receive at least one home and community-based waivered service
per month.”
Oregon, like many states, has separate systems and care pathways for children with
behavioral health and I/DD service needs. The language found in the 1915(c) waivers and
the K Plan makes it challenging to understand how a child with co-occurring needs could
be served through these mechanisms. The HCBS authorities (1915(k), 1915(c), 1915(i),
1915(j)) and long-term nursing facility services are statutory carve-outs from CCOs and are
provided through the Open-Card system. CCOs are required to cover PRTF but not HCBS.
They are required to provide care coordination for individuals receiving HCBS who are
enrolled in their CCO. Guidance to CCOs in 2020 stated that all admissions to PRTFs,
including subacute treatment, would require a Certificate of Need, but there is no single
set of medical necessity criteria (MNC) for this level of care as it is set by each CCO. This
further complicates the ability of children to access K Plan services.
In 2023, legislation was introduced in Oregon to improve the ability of children with mental
health needs to access K Plan services, including through alignment with PRTF
requirements. It is anticipated that it will be reintroduced in the 2024 Session.
Recommendations:
1. Ensure there is specific training and coaching for providers to address the screening,
diagnostic, and behavioral health treatment needs of persons with I/DD. Identify
opportunities to support behavioral health clinicians to receive training to use the
most updated diagnostic tools and manuals.
2. Utilize population-level utilization and outcomes reports across waiver and state
plan services to ensure individualized planning and access to all Medicaid services
across each CCO for individuals with co-occurring behavioral health and I/DD
service needs.
3. Ensure that processes and governance structures solicit meaningful input from
families and youth who experience behavioral health and I/DD service needs and
support interagency coordination and planning to align services and supports for
individuals with co-occurring service needs.
42
Oregon Health Authority. (2023).
Prioritized List, Guidelines, Interventions, & Services for Non-
Coverage.
Available from: https://www.oregon.gov/oha/HPA/DSI-HERC/Pages/Prioritized-List.aspx

21
4. Provide guidance to families, CCOs, and partners on the potential benefits of genetic
testing for children and youth with I/DD, particularly when they are demonstrating
behavioral problems and behavioral health conditions that are not being well-
managed or treated. Support families and caregivers to request testing if desired
and appropriate, using such e guidance to clarify that, under EPSDT, genetic testing
may be covered beyond what is detailed in the Prioritized List based on the
individual needs of the child and family, in keeping with guidance from the American
College of Medical Genetics and Genomics.
5. Ensure that efforts to expand access to K Plan services for children with behavioral
health needs are done in coordination and alignment with the existing service
systems, including those serving children and youth with intellectual and
developmental disabilities. Support alignment and integration of care pathways and
access points rather than creating separate, parallel approaches.
Substance Use Disorder 1115 Demonstration Waiver
Oregon has a long-term commitment to addressing SUD treatment needs. The 1115 SUD
Waiver increased identification, initiation, and engagement of Medicaid beneficiaries
diagnosed and engaged in SUD services, providing a continuum of care to increase the
chances of Medicaid beneficiaries of having a successful recovery process. Oregon’s
network adequacy standards (discussed below) recognize the urgency of providing SUD
treatment when it is requested. The SUD diagnosis, treatment, and recovery support needs
of youth and young adults with SUD may go unrecognized, overshadowed by the adult
SUD treatment and service delivery system. There are high prevalence rates of SUD
treatment needs among youth and young adults in need of mental health services,
particularly among populations of youth involved with juvenile justice systems, living in
more rural communities, and involved with child welfare or residential services.
43
Recommendations:
1) Ensure that the ASAM adolescent substance use levels of care are covered, including
clarifying that coverage through the CCOs includes ASAM Level 0.5 (EI), Level 1
(OP), and Level 2.1 (IOP).
2) Explicitly require that the CCOs provide coverage of SUD providers with
demonstrated expertise in delivering SUD services to the emerging adult
population.
Open-Card (Fee-for-Service) System
The Open-Card system provides necessary services to individuals and families when they
are unable to access them through their CCO. However, it is unclear which services are
available only through the Open-Card versus the CCOs and whether there is significant
variation by CCO or region. It also is unclear when members will be expected to access
FFS in order to receive a medically necessary service under EPSDT or whether the CCOs
will cover the service while maintaining the individual within the CCO.
In 2024, OHA issued a new Open-Card Handbook
44
that provides more extensive
information than previously available for members about what is covered under Open-
43
SAMHSA. (2021).
Treatment Considerations for Youth and Young Adults with Serious Emotional
Disturbances/Serious Mental Illnesses and Co-occurring Substance Use.
(Publication No. PEP20-06-02-
001.) Available from https://store.samhsa.gov/sites/default/files/pep20-06-02-001.pdf.
44
Oregon Health Authority. (2024).
Oregon Health Plan Open Card Member Handbook.
Available from
https://www.oregon.gov/oha/HSD/OHP/Tools/Open-Card-Handbook-EN.pdf.

22
Card, along with how to access the services and obtain more information. The handbook
provides information on the OHP Open-Card, general information on benefits, information
on care for kids and emergencies, and additional information, including care for American
Indian/Alaska Native members.
Recommendations:
1) Clarify which services are provided through Open-Card and not CCOs, using the
service list recommended above as a guide. Clarify the services that are always
provided through Open-Card versus those that
may
be provided by the CCO and
outline pathways for accessing services under those scenarios.
2) Explore opportunities to provide support to OHP members during non-traditional
working hours, including evenings and weekends, to ensure individuals and families
can access necessary support.
Intensive In-Home Behavioral Treatment (IIBHT) Services
IIBHT is designed to be a community-based alternative to residential treatment and
inpatient hospitalization for children and youth. Initially implemented through the FFS
system, CCOs were funded for and became required to cover the IIBHT benefit in 2021.
IIBHT was designed to serve children and youth who require 4-6 hours of intensive, in-
home services weekly to address their behavioral health needs. It is available to children
with I/DD service needs in their own homes as well as children in foster homes, group
homes, shelter care, and behavior rehabilitation services. In 2022, IIBHT was not available
in 10 counties. However, the list of IIBHT certified providers accepting referrals is growing
and all CCOs currently have IIBT. The workforce challenges identified below have impacted
this service itself as well, limiting the number of youth and families able to benefit.
45
While this service appears to be serving youth with intensive needs as intended, there may
be children and youth who would be eligible for the service who are unable to access it,
not only due to limited availability of providers, but due to challenges with meeting the
medical necessity criteria. The criteria outlined in both Oregon Administrative Rule 410-
172-0650 and the Frequently Asked Questions
46
states that Medicaid-eligible children
under age 21 must have “multiple behavioral health diagnoses” that “impact on multiple
life domains” and “significant safety risks or concerns.” While there are exceptions for
children who are at-risk of out-of-home placement or are transitioning home from an out-
of-home placement, these standards seem limiting and make it less likely for children to
be able to access the necessary intensity of services.
Additionally, while Oregon Administrative Rule 410-172-0650 states that, in requesting
initial authorization for IIBHT, the request must include “Sufficient information and
documentation to justify the presence of two or more primary mental health diagnoses
that meets the medically necessary reason for services,” Oregon Administrative Rule 309-
019-0167 states that the IIBHT assessments shall include “Sufficient information and
documentation to justify the presence of a qualifying DSM 5 diagnosis that is the medically
45
Data, Evaluation and Technical Assistance team, Oregon Health & Science University. (2023).
Intensive
In-Home Behavioral Health Treatment 2022 Annual Report.
Available from the OHA website:
https://www.oregon.gov/oha/HSD/BH-Child-Family/Documents/IIBHT-Annual-Report-2022.pdf
46
Oregon Health Authority, Health Systems Division, Child & Family Behavioral Health Unit. (2020).
Frequently Asked Questions Intensive In-Home Behavioral Health Treatment (IIBHT).
Available from the
OHA website: https://www.oregon.gov/oha/HSD/BH-Child-
Family/Documents/IIBHT%20FAQ%20Part%201%20102320.pdf

23
necessary reason for services.” These rules appear to contradict each other, with the
former requiring two diagnoses and the latter requiring one.
Recommendations:
1) Continue to increase the availability of IIBHT statewide, including assessing
availability using network adequacy standards.
2) Continue to collect and analyze data on the implementation of IIBHT to assess
whether the program is serving the population as intended and the associated
program outcomes. Consider collecting data on length of time from referral to
treatment start date as an additional metric to assess network adequacy.
3) Revise the Administrative Rules and FAQ to align medical necessity criteria for IIBHT
to clarify the number of diagnoses required to access the service. Consider reducing
the requirement for two diagnoses to one diagnosis while maintaining a requirement
that the conditions are impacting multiple life domains (or the youth is at-risk for or
transitioning from an out-of-home placement).
4) Convene a workgroup with mandatory participation by CCOs and county programs
to:
a. Identify and address barriers to launching IIBHT in counties where it has not
launched.
b. Identify and address barriers to adequate and timely coverage in counties
where it has launched.
c. Clarify the responsibility of CCOs in supporting the effective operation of
IIBHT.
d. Work with CCOs to estimate current need by region, to identify who is
accessing and not accessing IIBHT services, as well as alternatives utilized by
those not accessing IIBHT; and,
e. Clarify and improve pathways to care for youth eligible for IIBHT services
who are not being referred or otherwise getting access to the program.
Diagnosis to Support Effective Treatment of Young Children
Oregon created the
Oregon Early Childhood Diagnostic Crosswalk
in 2018 (updated in
2022)
47
based on the national ZERO to THREE guidance, which aligned The Diagnostic
Classification of Mental Health and Developmental Disorders of Infancy and Early
Childhood (DC:0-5), The Diagnostic and Statistical Manual of Mental Disorders, Fifth
Edition (DSM 5), and The International Statistical Classification of Diseases and Related
Health Problems, tenth revision (ICD-10). This crosswalk is designed to support effective
and accurate diagnosis of and treatment to young children, facilitating more preventative
and early access to needed services before behavioral health issues progress. This is an
example of leveraging and aligning tools to support a coordinated pathway to care.
Additionally, in 2022, the federal Centers for Medicaid and CHIP Services (CMCS) urged
States to “avoid requiring a behavioral health diagnosis for the provision of EPSDT
services. States can determine that some services are medically necessary for children and
youth without a diagnosed behavioral health condition.
48
47
Theodorou, L. (2022).
Oregon Early Childhood Diagnostic Crosswalk.
Available from the OHA website:
https://www.oregon.gov/oha/HSD/BH-Child-Family/Pages/Early-Childhood.aspx
48
Centers for Medicaid & CHIP Services (CMCS). (2022).
Leveraging Medicaid, CHIP, and Other Federal
Programs in the Delivery of Behavioral Health Services for Children and Youth
. Informational Bulletin.
https://www.medicaid.gov/federal-policy-guidance/downloads/bhccib08182022.pdf

24
Recommendations:
1) Update the language associated with the Early Childhood Diagnostic Crosswalk to
de-link it from the List of Prioritized Services and align it with EPSDT
implementation.
2) Provide regular and ongoing training to all behavioral health providers on the
application of the early childhood and CMS guidance to their assessment, diagnostic
and treatment services.
Metrics and Quality Measurement
Quality measurement and improvement processes are foundational to a healthy Medicaid
program. While CMS requires specific metrics such as the Child and Adult Core Set and
CAHPS be collected and seeks assurances that improvement processes are integral to the
Medicaid program, states must also ensure that metrics and improvement activities are
both customized and clearly communicated to all partners to monitor behavioral health
priorities for children. These metrics can also aim to help capture meaningful information
about the children, youth, and their families receiving behavioral health services.
Oregon’s metrics and quality measurement dashboard for its CCOs are exemplary. Many
of its metrics encompass functional improvement areas and identify desirable outcomes.
Throughout this report, we have recommended some additional CQI activities and data
collection that would enhance Oregon’s Medicaid program. One additional area of
improvement is increased specificity for measuring the effectiveness of behavioral health
services for children and youth. Oregon’s CCO Performance Metrics Dashboard includes a
demographic breakdown that specifies race and ethnicity, language, and disability, but
does not include a breakdown for age. For example, for Depression Screening data, the
only children included in Oregon’s current breakdown are aged 12 and older; the only
children’s data provided related to follow up care after ADHD medication prescription is
for children ages 6-12. Ensuring additional data collection to capture the experience of the
behavioral health system of the full range of childhood would help Oregon identify gaps
and areas of improvement.
Recommendations:
1) Provide data in age groupings that align with or are even more specific than what is
required in the CMS Core Set.
2) Ensure data collection efforts are implemented in alignment with recommendations
provided above (e.g., regarding network adequacy) and are reported in a manner
similar to those already provided in the dashboard.
3) To support implementation of IIBHT and to drive systems improvement, OHA and
OHSU should:
a. Continue to highlight the importance of data collection to programs and to
identify barriers to timely and accurate data reporting;
b. Develop a mechanism to track referrals to IIBHT that are not accepted or
delayed due to capacity issues and to track the barriers preventing prompt
enrollment;
c. Develop mechanisms to integrate data about youth mental health programs
and services, including IIBHT, across the behavioral health continuum of care,
to create a more comprehensive picture of needs as well as strengths in the
system; and
d. Develop and implement a follow-up family survey to obtain family
perspectives on IIBHT services, including barriers to care following IIBHT.

25
Workforce Challenges & Opportunities
Oregon is not alone in facing significant behavioral health workforce challenges. Nationally,
there is a scarcity of behavioral health professionals, including but not limited to
psychiatrists, which is exacerbated by challenges associated with Medicaid insurance
rates.
49,50
Demographics of the behavioral health workforce are not always reflective of
the people and communities served and people of color, non-English speakers, and
LGBTQ+ individuals may struggle to find providers able to provide culturally and
linguistically competent and affirming services.
49
Additionally, it is challenging to determine the full extent of the behavioral health
workforce shortage. A study of Oregon’s CCOs prior to the COVID-19 pandemic found that
over two-thirds of mental health prescribers and 59% of mental health non-prescribing
clinicians were “phantom” providers who were listed as in-network with the CCOs but did
not see Medicaid patients.
51
The authors of this study found that these phantom networks
“were larger and realized access was lower among specialty mental health providers than
among primary care providers”(p.1018). They observed that, while some geographic
constraints exist with health care shortage areas and low workforce supplies, other factors
including administrative capacity (including data collection and validation), network
monitoring, and enforcement mechanisms may contribute to the variation across the
CCOs.
51
Oregon was one of 27 states that had Medicaid reimbursement rate increases for
behavioral health providers in FY2022 and/or FY2023.
50
Oregon is to be commended for
directing its CCOs to increase the rates paid to behavioral health providers. OHA
reinvested savings from 2022 and utilized new legislative funds to support these increases.
Providers with more than 50% of service revenue from Medicaid received a 30% increase
while providers with less than 50% of service revenue from Medicaid received a 15%
increase. This creative approach to reimburse helps to incentivize providers to accept
Medicaid reimbursement as a larger share of their overall revenue. OHA also provided
differentials for providers who deliver culturally and linguistically specific services and
serve members who have co-occurring disorders.
52
In addition to increasing rates,
strategies employed across the U.S. to address the behavioral health workforce shortage
included reducing provider administrative burden, extending the workforce, and
incentivizing participation, including through prompt payment policies.
50
Key informants discussed the “great resignation” in behavioral health in Oregon prior to
the pandemic, noting it was accelerated with retirements and the pandemic. In 2022, over
49
Counts, N. (2023).
Understanding the U.S. behavioral health workforce shortage.
Available from The
Commonwealth Fund:
https://www.commonwealthfund.org/publications/explainer/2023/may/understanding-us-behavioral-
health-workforce-shortage.
50
Saunders, H., Guth, M., & Eckart, G. (2023).
A look at strategies to address behavioral health workforce
shortages: Findings from a survey of State Medicaid programs.
Available from KFF:
https://www.kff.org/mental-health/issue-brief/a-look-at-strategies-to-address-behavioral-health-
workforce-shortages-findings-from-a-survey-of-state-medicaid-programs/
51
Zhu, J.M., Charlesworth, C.J., Polsky, D., & McConnell, K.J. (2022). Phantom networks: Discrepancies
between reported and realized mental health care access in Oregon Medicaid.
Health Affairs (41).
DOI:10.1377/hlthaff.2022.00052.
52
Oregon Health Authority. (2022).
OHA Releases 2023 CCO Capitation Rates.
[OHA & ODHS Bulletin]
Available from
https://content.govdelivery.com/accounts/ORDHS/bulletins/3337ade#:~:text=OHA%20is%20increasing
%20behavioral%20health,50%25%20service%20revenue%20from%20Medicaid.

26
half of the youth who completed IIBHT identified barriers in accessing care at the time of
program completion. These included limited access to an in-network provider and
difficulty finding an outpatient provider willing or able to work with the youth’s level of
acuity.
45
Anecdotally, the complex challenges that the behavioral health workforce
encounters has made some seek other employment at the same or higher wages. School-
based mental health services have been one area where some counties have been able to
be innovative and effective and compensate for gaps in services in the larger community.
As a locally developed and managed service, the service providers may better reflect the
community being served. It was also noted that it may be more common for a provider to
have a contract with a CCO but not participate in the Open-Card system. As a result,
individuals receiving behavioral health services outside of the CCO, including individuals
who are American Indian or Alaska Native and have elected not to enroll in a CCO, may
have more limited provider selection.
Oregon is to be further commended for its actions in 2021 and 2022 to increase the
recruitment and retention of behavioral health providers who are people of color, tribal
members, or residents of rural areas of Oregon and can provide culturally responsive care
for diverse communities. This $80 million Behavioral Health Workforce Initiative is
supporting these efforts through clinical supervision grants; scholarships, tuition assistance
and stipends; student loan repayment; workforce bonus and housing stipend incentives;
recruitment and retention activities; licensing board fee waivers; and partnerships with the
nine Federally Recognized Tribes of Oregon.
In 2023, OHA was legislatively required to convene a workgroup to study major barriers
to workforce recruitment and retention in Oregon’s publicly financed behavioral health
system and produce recommendations for improvement, with an initial report due in
January 2025 and a final report in December 2025. This HB 2235 Workgroup was just
convened in December 2023. The Workgroup’s draft charter observes that “low pay,
administrative burden, high volume, and high acuity needs of clients are major factors in
providers leaving the field.”
In May 2022, the mean wage (across all payers) for substance abuse, behavioral disorder,
and mental health counselors in Oregon was $29.32/hour. The median wage for child,
family, and school social workers; health care social workers; mental health and substance
abuse social workers; and all other social workers was similarly low ($28.55, $37.09, $26.14,
and $28.66 respectively).
53
Inflation, while decreasing, means that a wage of $29.32/hour
in May 2022 had the same buying power as $30.80 in November 2023. Over a 40-hour
work week, that is a difference of $59.20, or $3,078.40 over one year.
While we were unable to examine the reimbursement rates paid by the CCOs to providers,
we did review the rates of services under the Open-Card system. CCOs are required to pay
the Open-Card rates to non-contracted providers but CCOs are not required to pay these
rates for their providers. In fact, OHA “encourages CCOs to use the flexibilities provided
by contract to determine the appropriate codes and rates to use for reimbursement to
53
Bureau of Labor Statistics. (2023).
Occupational Employment and Wage Statistics Query System.
Query run 12/30/23. Available from
https://data.bls.gov/oes/#/geoOcc/Multiple%20occupations%20for%20one%20geographical%20area
.

27
contracted providers, based on your area’s demographics and the services you provide to
your members.”
54
The rates for many services in the Open-Card fee schedule are robust, particularly when
provided with prior authorization (e.g., 45 minutes of psychotherapy with the patient
and/or family member is $178.55 with prior authorization of $142.85 without). However,
some services have rates that disincentivize providers, both through their low rate and the
administrative burden. For example, Community-Based Wraparound Services provided
through a certified fidelity Wraparound program is reimbursed at $27.32 per 15 minutes.
The 15-minute billing requirement is misaligned with the Wraparound service delivery
model, which requires ongoing work across a week or month to include individual meetings
with the child and family, team member engagement, collateral contacts, assessments,
care planning activities, and facilitation of child and family team meetings. Many states
provide a monthly per member per month capitated rate for the service.
30
Similarly, the 15-
minute billing increment and rate for Multisystemic Therapy for juveniles seems overly
burdensome (given the service delivery model) and low. For example, Louisiana (ranked
39
th
in total cost of living) pays $36.01/15 min and New Mexico (ranked 46
th
in total cost
of living) pays $48.56/15 minutes. This is compared to $24.81/15 minutes in Oregon, which
ranks 10
th
(i.e., more expensive) in total cost of living.
55
Some states have utilized a Center of Excellence
56
to support workforce development
(including training and coaching), performance measurement and continuous quality
improvement, policy and financing, interagency initiatives, and sustainability efforts. States
use Centers of Excellence to support specific interventions (e.g., evidence-based practices
like Multisystemic Therapy or Functional Family Therapy) and practice models (e.g.,
intensive care coordination using Wraparound) as well as broad-based activities related to
children’s behavioral health and well-being. Such a Center helps state agencies to improve
outcomes for shared populations that are engaged with multiple public child- and family-
serving agencies through shared accountability and oversight of initiatives; economies of
scale in training, coaching, and continuous quality improvement costs and activities; and
consistency in interagency implementation.
Recommendations:
1. In addition to general efforts to strength the child and youth behavioral health
workforce, OHA should focus on efforts related to:
a. Developing and supporting the IIBHT workforce;
b. Developing and supporting the peer workforce, with efforts specific to youth
and caregiver peer support embedded as part of a broader effort;
c. Providing training, coaching, and ongoing support to providers with
expertise in serving older youth and young adults; young children and their
families; and children and youth with co-occurring mental health, I/DD,
and/or SUD service needs.
54
Oregon Health Authority. (2022).
OHP Fee-for-Service Behavioral Health Fee Schedule.
Available
from the OHA website:
https://www.oregon.gov/oha/HSD/OHP/Tools/BH-Fee-Schedule-Fact-
Sheet.pdf.
55
Rothstein, R. (2023). Examining the cost of living by state in 2023. Available from Forbes:
https://www.forbes.com/advisor/mortgages/cost-of-living-by-state/
56
For more information, see Mettrick, J., Harburger, D.S., Kanary, P.J., Lieman, R.B., & Zabel, M. (2015).
Building Cross-System Implementation Centers: A Roadmap for State and Local Child Serving Agencies
in developing Centers of Excellence (COE). Available from the Annie E. Casey Foundation:
https://www.aecf.org/resources/building-cross-system-implementation-centers
.
28
2. Consider developing a Center of Excellence to support sustainable and effective
behavioral health workforce initiatives across behavioral health, I/DD, child welfare,
juvenile justice, and school systems.
3. Obtain data on the distribution of the 2023 rate increases to providers and require
the CCOs to provide updated data on their providers to assess whether the
differential rates expanded access or incentivized any providers to expand the share
of their revenue from Medicaid. Explore whether it is possible to implement another
rate increase, taking inflation into account.
4. Ensure that the HB2235 Workgroup includes individuals with expertise in child and
youth behavioral health services and co-occurring services (mental health, SUD, and
I/DD), including both providers and individuals with lived experiences. The current
workgroup membership includes some consumer organizations, but none
specifically focused on children and youth services and systems.
5. Ensure that the HB 2235 Workgroup explores specific needs of the public child and
youth behavioral health system, including the need for providers to be trained,
coached, and compensated for working across life domains and as part of
interdisciplinary teams. Members should understand the relationship between the
providers contracted by child welfare, juvenile justice, and other systems to
Medicaid.
6. Consider standardizing minimum rates paid to providers across the CCO and Open-
Card systems to support a robust workforce and consistency statewide.
7. Review rates paid under the Open-Card system for less traditional services to ensure
that they are sufficient. An initial review should look at services that may not be
included in the Medicare fee schedule, since many Medicaid rates are set at 70% of
Medicare rates. Services to be reviewed could include Wraparound, Multisystemic
Therapy, care coordination, expressive therapies, peer support, and mobile response
and stabilization services for children and youth.
Conclusion
As noted throughout, Oregon has much to be proud of in their child and youth public
behavioral health system. Most policies and rules are clear and specific about values and
expectations. Oregon is a leader nationally in adopting Medicaid authorities to expand
access to vulnerable populations of children, youth, and young adults. Oregon has
recognized the importance of local and regional voice in designing and implementing
services. As stated above, the state and its local and regional partners collectively have
spent years working to reform and improve its behavioral health system for children, youth
and families, which are reflected by the structures and financing.
However, there are several key areas that Oregon should strengthen. These include
adopting more consistent standards across regions and CCOs, providing additional
oversight and support for the implementation of EPSDT, and identifying opportunities to
better delineate services, requirements, performance measures, and workforce needs to
support children and youth with behavioral health needs.
Children and youth with behavioral health needs require a different approach to service
delivery, which necessitates specialized approaches to care pathways, coordination of
services, provider recruitment and retention, reimbursement, continuous quality
improvement, and engagement. Approaches that are successful for adults or in primary
care are not necessarily appropriate or effective for children and youth with behavioral

29
health needs. These approaches must be further customized to meet the cultural and
linguistic needs of the children and youth served by OHP and Oregon must elevate the
needs of individuals who identify as Black, Indigenous, and People of Color to ensure that
they are not marginalized, and their experiences are not lost among larger datasets and
feedback.
Currently, CCOs have significant latitude in developing provider networks, determining
care pathways, and determining reimbursement rates and billing codes. This has resulted
in an imbalanced system where children and youth across the state have inconsistent
access to services and supports and families experience a lack of transparency. Oregon
should provide clearer foundations and expectations statewide; this can be done
effectively without sacrificing local, regional, and CCO customization and innovation.
We encourage OHA and its sister agencies to review the findings of this report and its
recommendations and prioritize them, with input from partners, including families and
youth. We recommend using Results-Based Accountability
57
to support this prioritization,
an approach that encourages states and communities to rate strategies based on their
values, leverage, reach, and lift. We believe all of the proposed recommendations align
with SOC values, but partners should also assess this alignment. Oregon should consider
whether the proposed strategies will help to achieve the desired results (leverage), how
hard it will be to implement and, as appropriate, sustain the recommendation in terms of
human capital as well as fiscal resources (reach and lift).
Oregon’s child and youth public behavioral health system has a strong foundation based
upon system of care values and principles that permeate throughout administrative rules,
contracts, and guidance documents. This report provides a series of recommendations to
build upon that strong foundation and Oregon’s commitment to children, youth, and
families.
57
Results-Based Accountability has free training and resources, including tools and webinars, available
online: https://clearimpact.com/results-based-accountability/
.
30
Appendix
31
Appendix A: Review Process
Document Review
Innovations Institute reviewed a series of documents provided by the Oregon Health
Authority, as well as documents found online, referenced in other documents, and
recommended during key informant interviews. In addition to materials found on the OHA
website, the following documents were reviewed to inform this report:
• Comagine
o Comagine Annual report
o Comagine Contract renewal 2023
o Comagine PSK Amendment 2019
o Comagine Oregon Medicaid Utilization Review Quarterly Report - 2022 Q4
o Comagine Oregon Medicaid Utilization Review Quarterly Report - 2023 Q1
o Comagine Contract with OHA 2021-2023
2022 Amendment 01 to Contract
o Comagine Renewal 3/28/2023
Invoices 2022 and 2023
• CCOs
o CCO 2.0 Contract
o Trillium System of Care 2022
o Trillium Tri-county System of Care policy 2022
o Pacific Source System of Care policy 2021
o CPC North Coast System of Care 2022
o Eastern Oregon System of Care policy 2022
o Health Share Behavioral Health System of Care policy 2022
o InterCommunity Health Network CCO System of Care Policy 2022
o Jackson Youth System of Care policy 2022
o AllCare Health Behavioral Health System of Care policy
o Advanced Health System of Care Policy
o CHA System of Care policy 2022
o OHA Evaluation Criteria: 2022 System of Care (SOC) Policy and Procedure
o Children’s CFAA Agreements
2022 Mobile Response and Stabilization Services Administrative Rules
2022 SE26A Early Assessment and Support Alliance
• Medicaid
o 1115 Demonstration Waiver
o 1915(b)(4) Waiver
o 1915(c) Behavioral ICF IDD Model Waiver
o 1915(c) Children’s Home and Community Based Services Waiver
o 1915(c) Home and Community Based Services Waiver – Aged and
Physically Disabled
o 2022-2027 1115 Demonstration Approval
o 2022-2027 Demonstration Amendment
o 1915(k) Community First Choice State Plan Option, State Plan under Title
XIX of the Social Security Act
o Medically Fragile 1915(c) Waiver
o Medically Involved 1915(c) Waiver
o Oregon Approved Transition Plan Home and Community Based Services

32
o 1115 Demonstration waiver for Health Evidence Review Committee, with
CCO and global payment
2017-2022 waiver
Medicaid waiver webpage
2022-2027 waiver
o 1115 Demonstration waiver- Substance Use Disorder
2021 – 2026 waiver
o Oregon Department of Human Services overview and links to approved
waivers
o 1915(K) community first choice State Plan option
o 1915(i) Home and Community Based Services (HCBS); State Plan option
HCBS transition plan general
Seniors and Disabilities
1915(c) HCBS waivers operated through APD and ODDS
o Oregon Administrative Rules (OARs)
OARs HCBS
Outpatient OARS
Wraparound - OARs: 309 019 0163
Intensive In-Home Behavioral Health Treatment Services for Youth
(IIHBT) OARS: 410-172-0695
IIBHT Outpatient: 309-019-0167
IIBHT Prior Authorization: 410-172-0650
Mobile Crisis Intervention Services and Stabilization Services (MRSS)
Behavioral Rehabilitation Services OARs - 410-170-0000
Children’s CFAA agreements (SBMH, EASA, MRSS)
CoMagine contract for 1915(I) (special focus on transition into adult
system)
CoMagine contracts for ITS utilization management – 2021 – 2023
and pending
o Early and Periodic Screening, Diagnostic, and Treatment Benefit (EPSDT):
FAQ
OAR 410-151
Provider Guidance
EPSDT CCO Guidance
Provider Announcement EPSDT
Provider Change Log
o Oregon Health Plan Handbook (2023)
o Oregon Health Plan Open Card Member Handbook (2024)
o Prioritized List, Guidelines, Interventions, & Services for Non-Coverage
(2023)
o Early childhood crosswalk 2022
o EASA – SE26A and SE25A
o Trauma-Informed Policy 2014
o 2021 The Oregon Wraparound Best Practices Guide V.2
o Certification of Need for Services for Children’s Subacute Treatment,
Effective January 1, 2020
• System of Care
o System of Care Plan for Oregon Two Year Strategic Plan 2022-2023
o Trauma Informed Policy (2014)
• Other:

33
o Implementing the Child and Family Behavioral Health Policy Vision Paper
Roadmap 2020-2024
o CCO contract forms/required reporting
o 2022 HB 5299 Report: Barriers to Mental Health Services for Older Adults
and People with Disabilities Oregon Department of Human Services and
Oregon Health Authority
o 2022 Oregon FFS UR Annual Report
o Oregon Family First Prevention Services Act Plan
o SB4
o OHA Child & Family Behavioral Health Performance Indicators
o Ombuds Program Six Month Report
Key Informant Interviews
Key informants were interviewed virtually without a structured interview protocol. The
purpose of the interviews was to gain clarity and additional insight about documents
reviewed, identify additional documents to be reviewed and individuals to be interviewed,
and provide an opportunity for the individual(s) to share information or perspectives not
otherwise captured. Some interviews were conducted with groups. Hilary Harrison and/or
Chelsea Holcomb from OHA were present for most of the interviews.
The following individuals provided interviews:
• Angie Butler, Tribal Mental Health Specialist, Oregon Health Authority
• Hilary Harrison, System of Care Policy Strategist, Oregon Health Authority
• Dana Hittle, Interim Deputy Director, Office of Developmental Disabilities Services;
Senior Advisor on Medicaid Policy and Systems Integration, Director’s Office,
Oregon Department of Human Services (and former State Medicaid Director, OHA)
• Chelsea Holcomb, Child & Family Behavioral Health Director, Oregon Health
Authority
• Dave Inbody, CCO Operations Director, Oregon Health Authority
• Ebony Clarke, Behavioral Health Director, Oregon Health Authority
• Julie Johnson, Tribal Affairs Director, Oregon Health Authority
• Vivian Levy, Interim Medicaid Director, Oregon Health Authority
• Alex Palm, Policy Analyst, Oregon Department of Human Services
• Jason Steiner, Tribal Policy Analyst, Oregon Health Authority

Appendix B: Table of Recommendations
Subject Area
Recommendation
EPSDT Benefit:
Covered
Services &
Implementation
Support
1. Create a list of all covered specialty behavioral health services for children under 21 that are available
under the State Plan to serve as a guide to families, providers, and CCOs, emphasizing that this list
is a minimum floor and not a ceiling on services. The list of services should explicitly state the
required services provided by all CCOs.
2. Develop documentation outlining a pathway to requesting services not listed in the State Plan.
3. Engage families and youth in reviewing and adjusting the minimum list of covered services and
pathway, including methods for reaching families and youth and additional materials or messages
that could be further developed. Families and youth should have opportunities to provide
meaningful feedback on the design, implementation, and effectiveness of EPSDT, and how to ensure
that the minimum list reflects provider capacity, not service coverage allowability.
4. Work with provider associations and groups to support implementation of EPSDT and ensure
understanding of the documents and tools provided.
5. Enhance CQI processes to include specific quality performance metrics related to EPSDT; collection,
analysis, and use of these data to adjust statutory, regulatory, and contractual standards and
requirements; and meaningful opportunities for engagement and feedback. Monitor implementation
across metrics below to ensure that EPSDT is being implemented as intended.
a.
Metrics should be stratified by demographics, geographical area, and CCO coverage and
incorporated into the CQI process.
b. Implement oversight mechanisms of the CCOs to include
i. Ongoing and/or annual re-training on EPSDT;
ii. Review of who is and is not making EPSDT requests to support focused training and technical
assistance;
iii. Ensuring that no service limits or exclusions are being implemented inconsistent with EPSDT.
c. Recommended metrics include:
i.
Total number of primary care and pediatric providers and the penetration rate of those
trained with a minimum baseline established;
ii.
Total number of behavioral health providers serving pediatric populations and the
penetration rate of those trained training participation, with a minimum baseline established;
iii. The number and type of requests for behavioral health services under EPSDT and changes
to those requests over time;
iv. Questions and issues identified by families, youth, and providers for clarity or resolution; and,
v.
Achievement of network adequacy standards for specialty behavioral health services for
children and youth, by service type (discussed further below).
35
Expanding
Access and
Support
through the
1115 Waiver
1. Provide training, coaching, and implementation support to providers delivering services to young
adults ages 18-26 to ensure that they have the necessary expertise and knowledge of this unique
developmental stage of young adulthood.
2. Develop, collect, and analyze metrics, stratified by the above-recommended demographics,
reported by each of the prioritized populations and total overall.
a. Data should include the HRSN penetration rate for each of the prioritized youth populations,
with expectations that the CCOs will engage in outreach and training to providers serving these
populations to improve HRSN penetration rates.
b. Collect and report on provider network information that delineates providers with expertise in
emerging adulthood, much like is tracked for those with expertise in early childhood and make
this information available to young adults and CCOs.
3. As part of the Section 5121 requirements discussed below, Oregon will need to develop a plan for
certain screening and diagnostic services for youth in juvenile or correctional facilities. Given
Oregon’s plan to facilitate HRSNs, it will be important that the protocol to access HRSNs through
the CCOs align with Oregon’s Section 5121 plan.
4. As one of the first states providing services to address HRSN through an 1115 waiver, Oregon may
want to engage, formally or informally, with peers in Arizona, Arkansas, Massachusetts, New Jersey,
and Washington to share best practices and lessons learned. Oregon is applying for the Center for
Health Care Strategies’
Medicaid Health-Related Social Needs Implementation Learning Series;
regardless of acceptance, Oregon should track the work and findings of this Series.
5. Oregon should facilitate a learning collaborative with families, youth, and relevant state and local
partners to review the data, identify areas for improvement, and support implementation activities.
Child Welfare &
Juvenile
Justice-
Involved
Children
1. As part of CCO contracts, require CCOs to establish Memoranda of Understanding (MOU) with local
child welfare, juvenile justice, and developmental disabilities offices to improve coordination and
communication, support children and families to maintain continuity of care with providers, and
ensure that both the CCOs and the local agencies have a shared understanding of roles,
responsibilities, and expectations
2. OHA should leverage Federal Financial Participation (FFP) under Medicaid to support a children’s
behavioral health liaison between the child welfare agency and the CCOs to support improved
coordination and problem-solving.
3. Child welfare should track the implementation of FFPSA services and identify whether these services
are being provided in addition to or instead of children’s mental health services through the CCOs.
They should determine if the FFPSA services are supporting children and families to remain together
in their own homes and, if services are effective, explore coverage of them under the Medicaid State
Plan for Medicaid-eligible families.
4. OHA and DHS should jointly provide training and individualized coaching to child welfare and
Medicaid leaders and managers, as well as to local child welfare workers and supervisors and CCO

36
staff to support moving children out of temporary lodging and into the most effective, least
restrictive setting. DHS, in collaboration with OHA, families, youth, and other partners, should:
a.
Establish best practice standards, expectations, and guidelines for child welfare workers in
making individualized recommendations for out-of-
home placements for children who are
unable to remain in their own homes, prioritizing kin and fictive kin and other family-based
settings with additional supports as needed.
b. Integrate the CANS into care planning and use a standardized tool to support teams—including
youth and families—to identify goals and action steps, including timelines for discharging from
hospitals and congregate care settings and services needed to support a successful transition.
c. Develop a pathway to review and approve requests for individualized services and supports that
will enable children to be served in a family-based setting (e.g., one-on-one supports in the home
from 3-6pm on school days for a child that struggles during this time or access to an expressive
therapy or healing practice that is culturally responsive to the family’s needs).
d. Establish performance measures and a CQI process for congregate care placements for children
involved with child welfare and juvenile justice, looking at the clinical and behavioral health
services provided, the outcomes of the children in the programs, the ratios of direct care staff,
the length of stay in the program, and the discharge location (home, family-based setting, or
other congregate care setting). Data should be examined by demographic characteristics,
geographic location, and CCO enrollment.
5. In the plan in response to Section 5121, Oregon should ensure it aligns its screening and assessment
pathway to ensure a consistent approach for all individuals. It will be important to develop a pathway
not only with juvenile justice facilities, but with adult correctional facilities as well, given that youth
and emerging adults up to age 26 may be in adult correctional facilities.
6. Taking note of high trauma rates in this population, OHA should partner with other child- and family-
serving agencies to identify avenues for prevention, as well as expanding early evidence-based
treatment; these efforts should be incorporated into IIBHT programs.
7. Given the high percentage of youth in foster care in IIBHT, ODHS should be invited to regular reviews
of IIBHT to ensure that the needs of this population are being understood and addressed in IIBHT
programs.
8. OHA should ensure that the juvenile justice and child welfare agencies are part of the
implementation of the YSHCN and HRSN provisions of the 1115 Waiver to support alignment and
consistency across systems/payers, coordinate policies and procedures to leverage services and
supports for the shared population of youth, and ensure seamless access to services uniquely
available to this population to achieve shared outcomes (e.g., Foster Care Transition Funds,
Independent Living Program Provider Aftercare Support Services, Family Unification Program-Youth
vouchers, Foster Youth to Independence (FYI), Chafee Education & Training Grants).
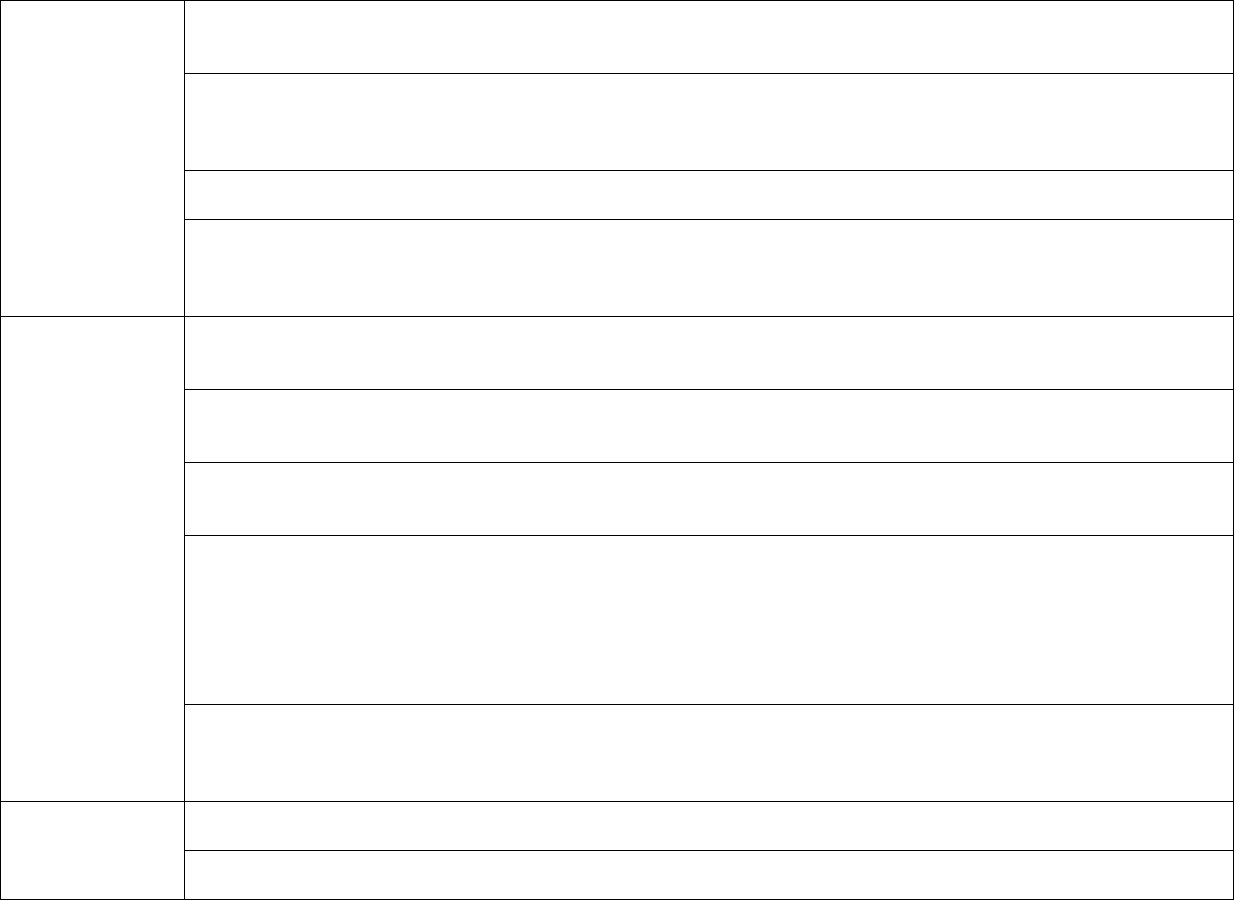
37
Additional
Managed Care
Oversight &
Regional
Design
Findings
1. In the new CCO contracts, Oregon should require that all CCOs use the same medical necessity
criteria, service authorization and utilization review criteria, billing codes, and pathway to care.
Oregon should consider standardizing reimbursement rates for providers, as discussed below.
2. Network adequacy standards should be further delineated for children’s mental health providers to
ensure consistent access statewide to a minimum array of services, including individual, group, and
family therapies; peer support; intensive in-home services; and mobile response and stabilization
services.
3. Clarify the roles and responsibilities of the BHRN versus the CCOs and how they are expected to
interface and support children and adults.
4. In the 1115 Waiver, the CCOs are required to implement various governance and organizational
councils to guide their work. Recognizing that consumers are specifically listed as participants, we
recommend further delineation to ensure that adult consumers, youth, and families are represented
and have an opportunity for meaningful participation.
State Plan
Options to
Support Youth
with Behavioral
Health & Co-
Occurring
Intellectual &
Developmental
Disability
(I/DD) Service
Needs
1. Ensure there is specific training and coaching for providers to address the screening, diagnostic, and
behavioral health treatment needs of persons with I/DD. Identify opportunities to support behavioral
health clinicians to receive training to use the most updated diagnostic tools and manuals.
2. Utilize population-level utilization and outcomes reports across waiver and state plan services to
ensure individualized planning and access to all Medicaid services across each CCO for individuals
with co-occurring behavioral health and I/DD service needs.
3. Ensure that processes and governance structures solicit meaningful input from families and youth
who experience behavioral health and I/DD service needs and support interagency coordination and
planning to align services and supports for individuals with co-occurring service needs.
4. Provide guidance to families, CCOs, and partners on the potential benefits of genetic testing for
children and youth with I/DD, particularly when they are demonstrating behavioral problems and
behavioral health conditions that are not being well-managed or treated. Support families and
caregivers to request testing if desired and appropriate, using such guidance to clarify that, under
EPSDT, genetic testing may be covered beyond what is detailed in the Prioritized List based on the
individual needs of the child and family, in keeping with guidance from the American College of
Medical Genetics and Genomics.
5. Ensure that efforts to expand access to K Plan services for children with behavioral health needs are
done in coordination and alignment with the existing service systems, including those serving children
and youth with intellectual and developmental disabilities. Support alignment and integration of care
pathways and access points rather than creating separate, parallel approaches.
Substance Use
Disorder 1115
Demonstration
Waiver
1. Ensure that the ASAM adolescent substance use levels of care are covered, including clarifying that
coverage through the CCOs includes ASAM Level 0.5 (EI), Level 1 (OP), and Level 2.1 (IOP).
2. Explicitly require that the CCOs provide coverage of SUD providers with demonstrated expertise in
delivering SUD services to the emerging adult population.

38
Open-Card
(Fee-for-
Service)
System
1. Clarify which services are provided through Open-Card and not CCOs, using the service list
recommended above as a guide. Clarify the services that are always provided through Open-Card
versus those that
may
be provided by the CCO and outline pathways for accessing services under
those scenarios.
2. Explore opportunities to provide support to OHP members during non-traditional working hours,
including evenings and weekends, to ensure individuals and families can access necessary support.
Intensive In-
Home
Behavioral
Treatment
(IIBHT)
Services
1. Continue to increase the availability of IIBHT statewide, including assessing availability using network
adequacy standards.
2. Continue to collect and analyze data on the implementation of IIBHT to assess whether the program
is serving the population as intended and the associated program outcomes. Consider collecting data
on length of time from referral to treatment start date as an additional metric to assess network
adequacy.
3. Revise the Administrative Rules and FAQ to align medical necessity criteria for IIBHT to clarify the
number of diagnoses required to access the service. Consider reducing the requirement for two
diagnoses to one diagnosis while maintaining a requirement th
at the conditions are impacting
multiple life domains (or the youth is at-risk for or transitioning from an out-of-home placement).
4. Convene a workgroup with mandatory participation by CCOs and county programs to:
a. Identify and address barriers to launching IIBHT in counties where it has not launched.
b. Identify and address barriers to adequate and timely coverage in counties where it has launched.
c. Clarify the responsibility of CCOs in supporting the effective operation of IIBHT.
d.
Work with CCOs to estimate current need by region, to identify who is accessing and not
accessing IIBHT services, as well as alternatives utilized by those not accessing IIBHT; and,
e. Clarify and improve pathways to care for youth eligible for IIBHT services who are not being
referred or otherwise getting access to the program.
Diagnosis to
Support
Effective
Treatment of
Young Children
1. Update the language associated with the Early Childhood Diagnostic Crosswalk to de-link it from
the List of Prioritized Services and align it with EPSDT implementation.
2. Provide regular and ongoing training to all behavioral health providers on the application of the early
childhood and CMS guidance to their assessment, diagnostic and treatment services.
Metrics and
Quality
Measurement
1. Provide data in age groupings that align with or are even more specific than what is required in the
CMS Core Set.
2. Ensure data collection efforts are implemented in alignment with recommendations provided above
(e.g., regarding network adequacy) and are reported in a manner similar to those already provided in
the dashboard.
3. To support implementation of IIBHT and to drive systems improvement, OHA and OHSU should:
a. Continue to highlight the importance of data collection to programs and to identify barriers to
timely and accurate data reporting;

39
b. Develop a mechanism to track referrals to IIBHT that are not accepted or delayed due to capacity
issues and to track the barriers preventing prompt enrollment;
c.
Develop mechanisms to integrate data about youth mental health programs and services,
including IIBHT, across the behavioral health continuum of care, to create a more comprehensive
picture of needs as well as strengths in the system; and
d. Develop and implement a follow-up family survey to obtain family perspectives on IIBHT services,
including barriers to care following IIBHT.
Workforce
Challenges &
Opportunities
1. In addition to general efforts to strength the child and youth behavioral health workforce, OHA should
focus on efforts related to:
a. Developing and supporting the IIBHT workforce;
b. Developing and supporting the peer workforce, with efforts specific to youth and caregiver peer
support embedded as part of a broader effort;
c. Providing training, coaching, and ongoing support to providers with expertise in serving older
youth and young adults; young children and their families; and children and youth with co-
occurring mental health, I/DD, and/or SUD service needs.
2. Consider developing a Center of Excellence to support sustainable and effective behavioral health
workforce initiatives across behavioral health, I/DD, child welfare, juvenile justice, and school systems.
3. Obtain data on the distribution of the 2023 rate increases to providers and require the CCOs to
provide updated data on their providers to assess whether the differential rates expanded access or
incentivized any providers to expand the share of their revenue from Medicaid. Explore whether it is
possible to implement another rate increase, taking inflation into account.
4. Ensure that the HB2235 Workgroup includes individuals with expertise in child and youth behavioral
health services and co-occurring services (mental health, SUD, and I/DD), including both providers
and individuals with lived experiences. The current workgroup membership includes some consumer
organizations, but none specifically focused on children and youth services and systems.
5. Ensure that the HB 2235 Workgroup explores specific needs of the public child and youth behavioral
health system, including the need for providers to be trained, coached, and compensated for working
across life domains and as part of interdisciplinary team
s. Members should understand the
relationship between the providers contracted by child welfare, juvenile justice, and other systems to
Medicaid.
6. Consider standardizing minimum rates paid to providers across the CCO and Open-Card systems to
support a robust workforce and consistency statewide.
7. Review rates paid under the Open-Card system for less traditional services to ensure that they are
sufficient. An initial review should look at services that may not be included in the Medicare fee
schedule, since many Medicaid rates are set at 70% of Medicare rates. Services to be reviewed could
include Wraparound, Multisystemic Therapy, care coordination, expressive therapies, peer support,
and mobile response and stabilization services for children and youth.
40
