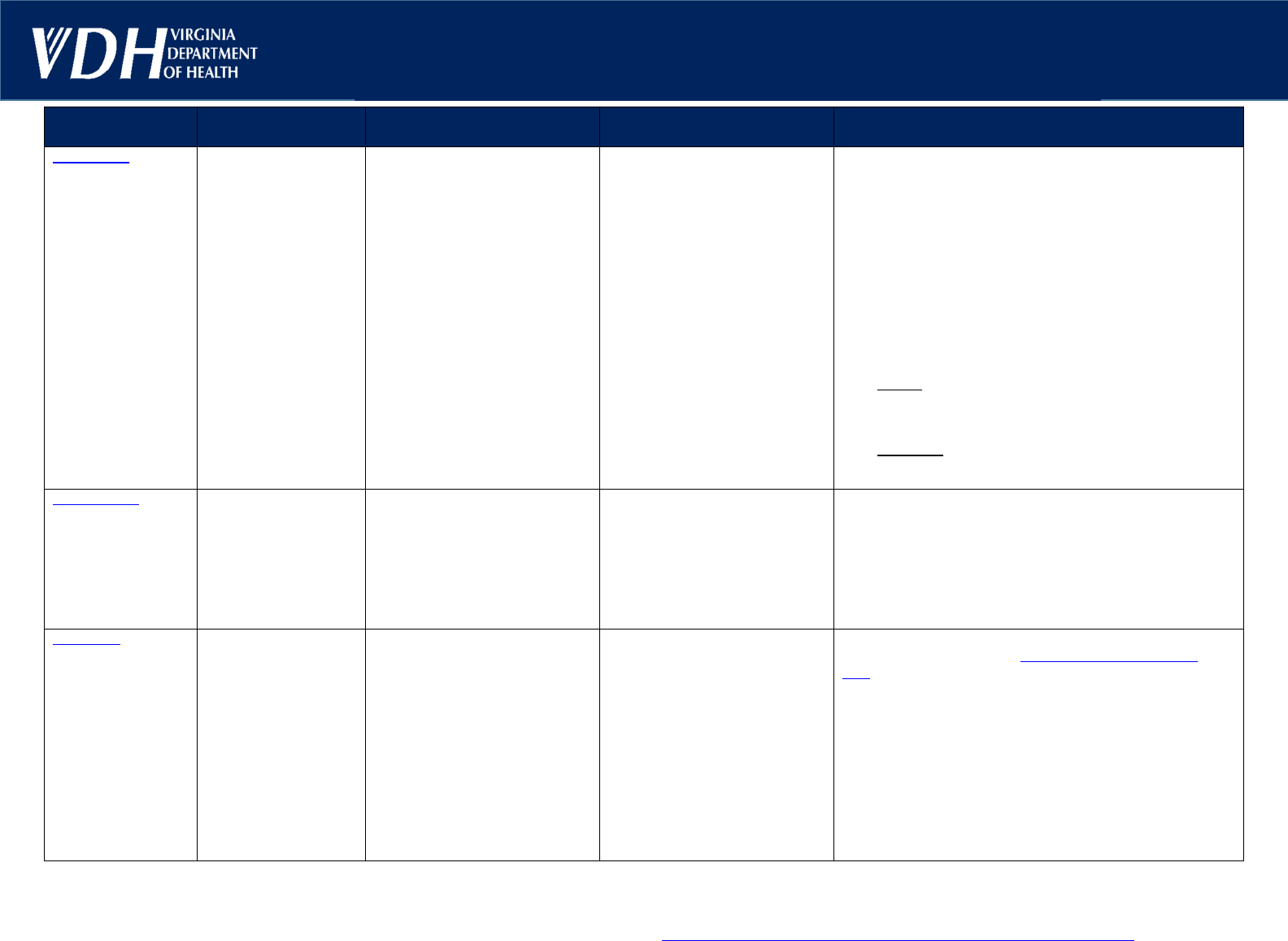
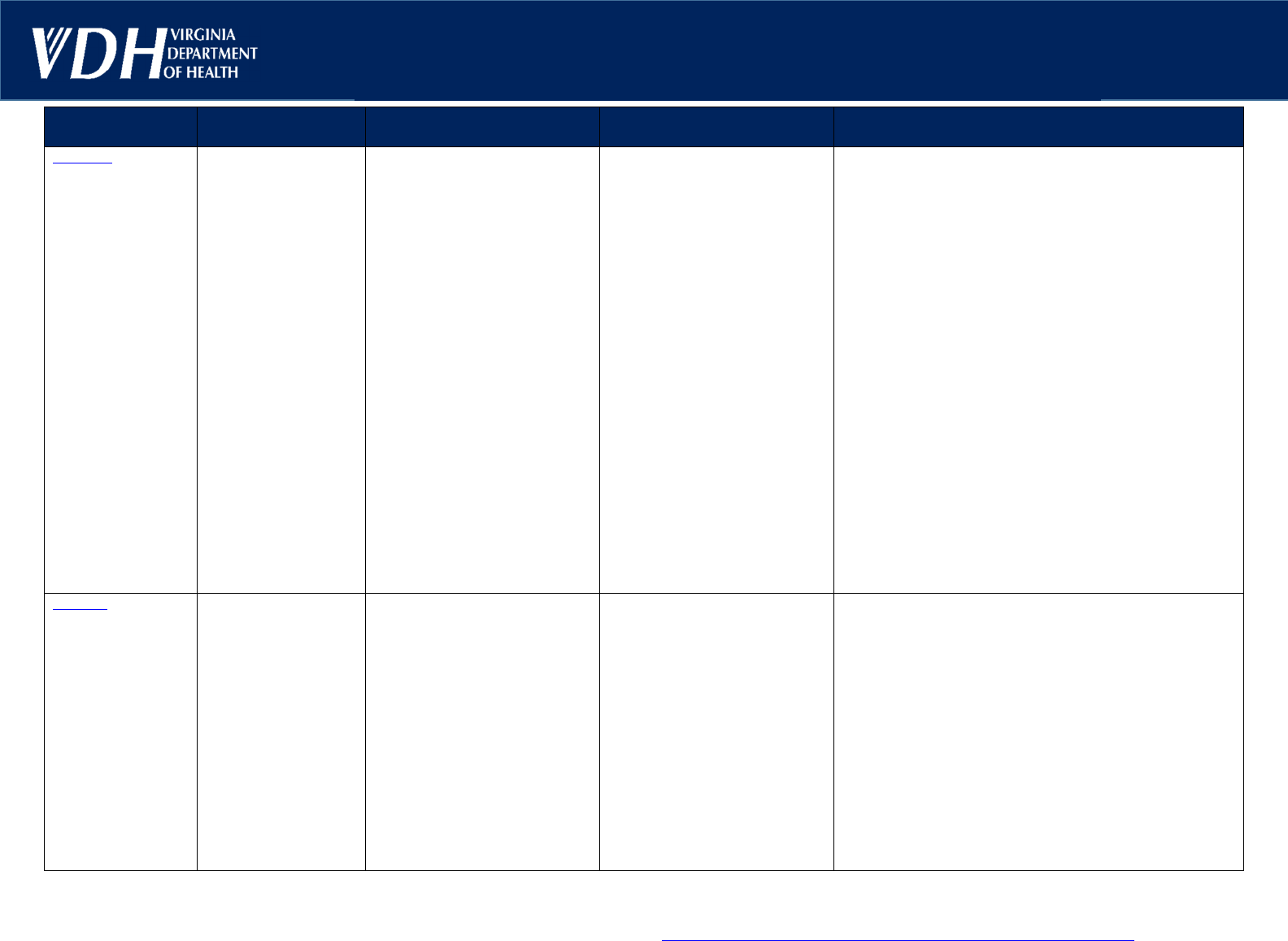
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Chickenpox
†
14
–
16 days Direct contact with vesicular fluid Sudden onset with slight fever, PATIENT: Exclude from school or child care until:
Uncomplicated varicella: the rash has crusted
Immunized patients without crust: no new lesions
appear within a 24-hour period
Patients with weakened immune systems: at least 5
days after eruptions first appear or until vesicles
become dry
Avoid exposure to women in early pregnancy who have not
had chickenpox and/or varicella vaccine.
CONTACTS: Check vaccination status of contacts in school
and child care and recommend vaccination if needed within
3 days and up to 5 days after exposure. For exposed
contacts without immunity:
School setting: exclusion not recommended unless an
outbreak is reported; monitor for varicella symptoms
for 8–21 days from exposure and until 28 days after for
those who received VariZIG or IVIG.
Child care setting: exclusion recommended for 8–21
days from exposure (28 days if VariZIG or IVIG given.)
If symptoms occur, exclude from school and child care.
(Varicella) (Range 10–21 days)
Incubation period may
be longer (28 days or
more) in persons who
receive immune
globulin for
postexposure
prophylaxis (VariZIG or
IVIG). Incubation
period may be shorter
in persons with
weakened immune
systems.
or by airborne spread from
respiratory tract secretions.
Infectious from 1–2 days before
rash onset until all lesions have
dried/crusted over and no new
lesions appear within a 24-hour
period (average is 4–7 days).
Communicability may be
prolonged in people with
weakened immune systems.
other systemic symptoms and
itchy eruptions which become
vesicular (small blisters) within
a
few hours. The rash first appears
on the chest, back, and face, and
then spreads over the entire
body. Lesions commonly occur in
successive crops, with several
stages of maturity present at the
same time. Typically, vesicular
rash consisting of 250–500
lesions in varying stages of
development (papules, vesicles)
and resolution (crusting).
Conjunctivitis
1–3 days
Variable depending o n
the cause.
Causes include
bacteria, viruses,
allergies, and
chemicals/irritants.
Contact with eye discharge or
contaminated articles, if the
cause is infectious (e.g., bacteria
or virus.)
Allergic and chemical causes are
not contagious.
Pink or red eye with swelling of
the eyelids, increased tears, and
eye discharge. Eyelids may be
matted shut after sleep. May
involve one or both eyes.
PATIENT: Exclude from school or child care while
symptomatic or until cleared to return by a healthcare
provider. Important to wash hands thoroughly after contact
with eye drainage. Do not share any articles that have come
into contact with the eyes.
CONTACTS: Exclusion not indicated.
(Pink Eye)
COVID-19
(Coronavirus
disease 2019
caused by SARS-
CoV-2 virus)
†
2–14 days
As virus variants
continue to emerge,
characteristics such as
incubation period and
ease of transmission
may change.
Inhalation or contact wit h
respiratory droplets; contact wit h
contaminated surfaces.
People are infectious 2 days
before symptom onset through
10 days after symptom onset,
with viral loads higher earlier in
the course of infection.
Patients may be asymptomatic or
may have a wide variety of
symptoms of variable severity:
Fever and/or chills
Cough and/or runny nose
Shortness of breath
Headache
Fatigue
Sore throat
Muscle or body aches
New loss of taste or smell
Nausea, vomiting, diarrhea
PATIENT: Please refer to CDC’s Preventin
g Spread of
Infections in K-12 Schools “When Students or Staff are
Sick.” Depending on severity of illness, refer to a healthcare
provider, urgent care center, or emergency department for
further evaluation and treatment.
CONTACTS: Quarantine is not recommended for contacts.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary o f major chan ges.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unu sual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 1 of10
Sep 2024
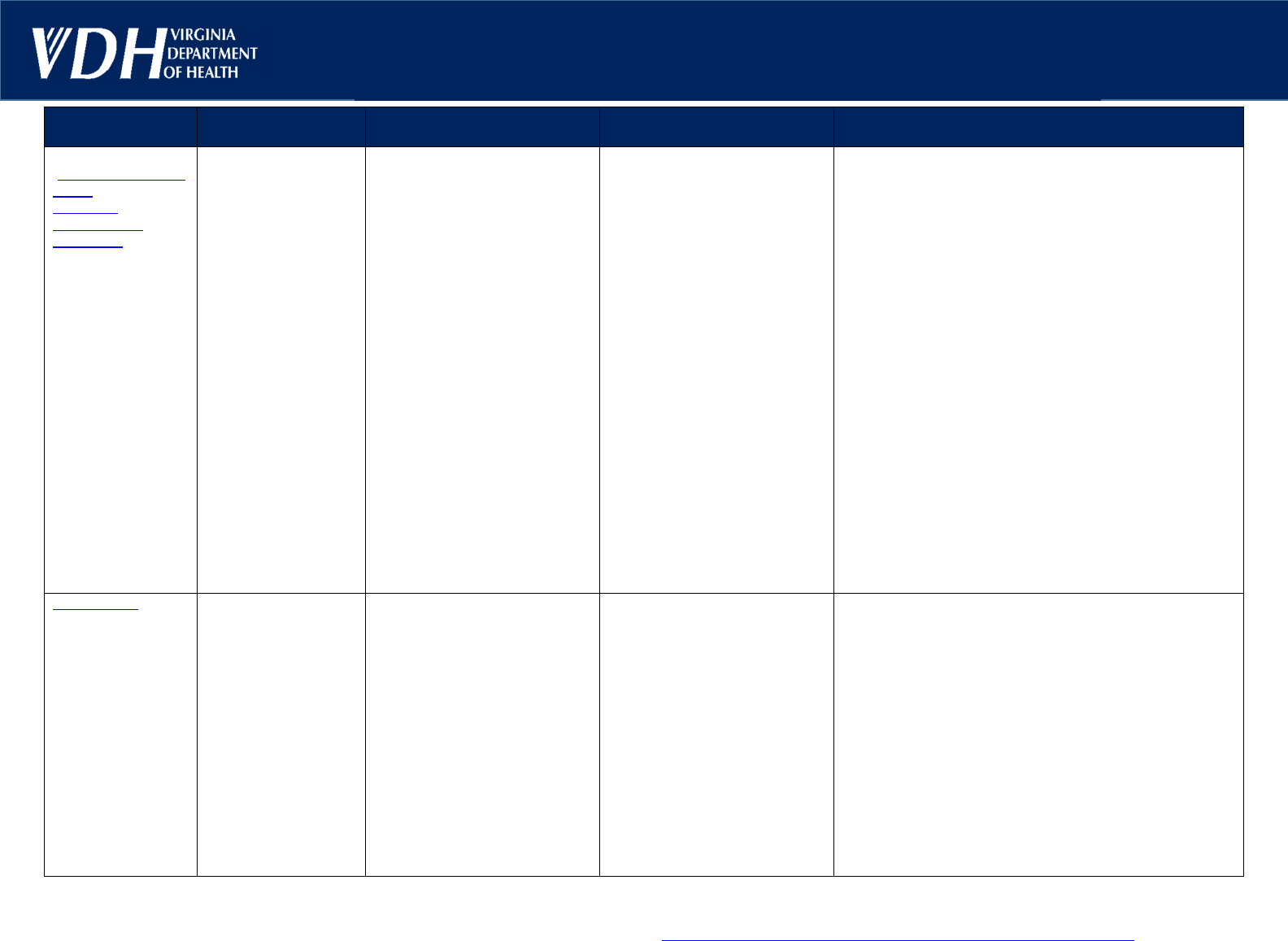
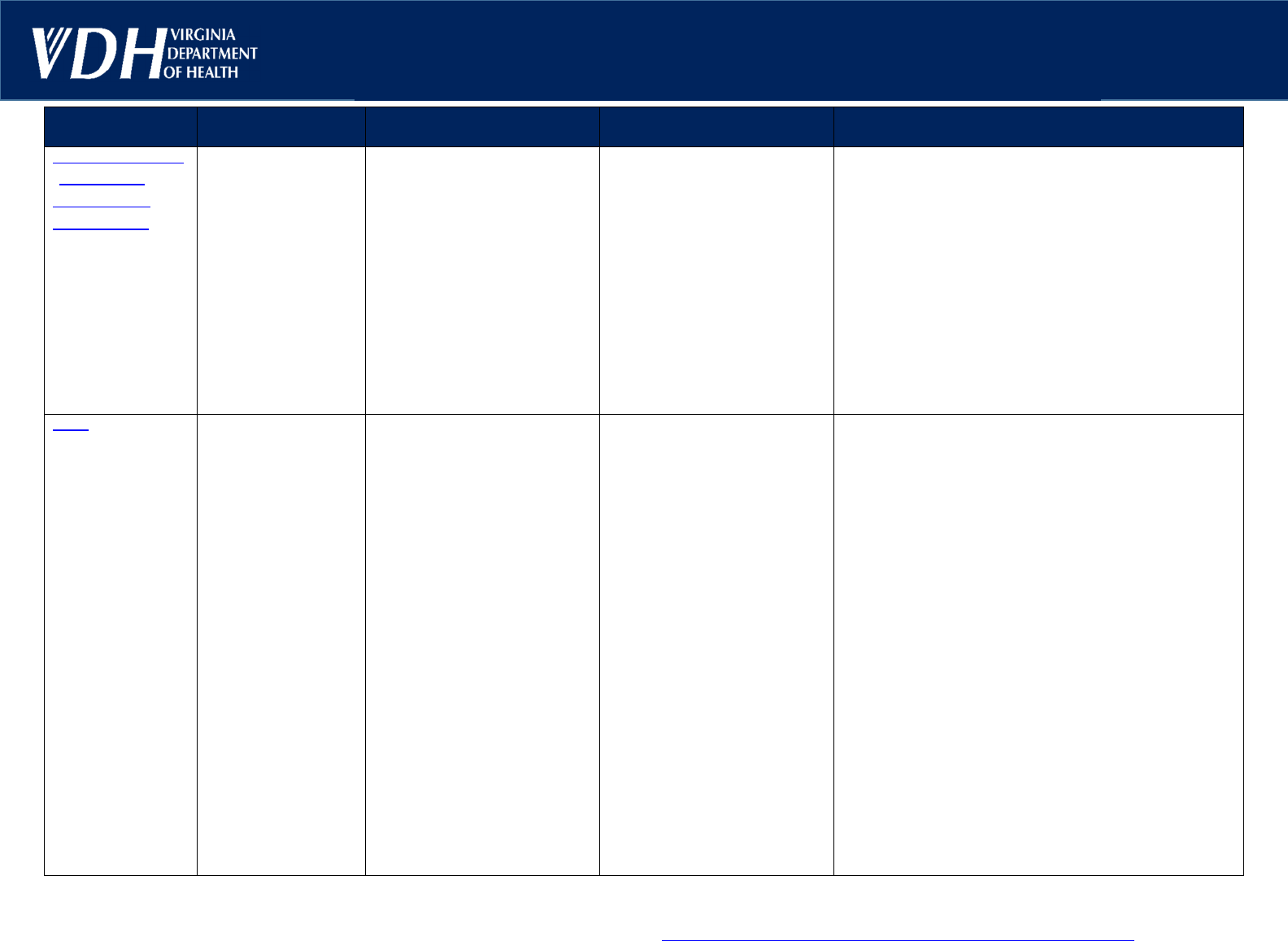
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Diarrheal Diseases
(Campylobacteriosis
E. coli O157:H7,
Giardiasis,
Salmonellosis,
Shigellosis, et
c.)
†
Campylobacteriosis:
2–5 days
(Range: 1–10 days)
E. coli O157:H7:
3–4 days
(Range: 1–10 days)
Giardiasis:
1–3 weeks
Salmonellosis:
12–36 hours
(Range: 6–72 hours;
though up to 16 days
has been reported)
Shigellosis:
1–3 days
(Range: 1–7 days)
Fecal-oral route through direct
contact or by ingestion of
contaminated, raw, or improperly
cooked food or untreated water
The most common symptoms
are diarrhea, abdominal pain or
cramping, malaise, and fever.
Stools can contain visible or
occult blood. Severe dehydration
may occur in young children.
Campylobacteriosis may mimic
appendicitis or intussusception.
E. coli O157:H7 may lead t o
hemolytic-uremic syndrome. I n
giardiasis, persons may be
asymptomatic or have
malabsorption wit h smelly,
greasy stool and weight loss.
Patients with weakened immune
systems can have prolonged,
relapsing, or extraintestinal
infections.
PATIENT: Exclude from school and child care until stools
are contained in the diaper or when continent patients no
longer have fecal accidents and when stool frequency
becomes no more than 2 stools above normal frequency for
the patient, even if the stools remain loose. Stress
importance of proper handwashing. In an outbreak setting,
consult local health department for clearance to return to
school/childcare setting. Please note that other resources
advise no return to school until diarrhea has ceased for at
least 24 hours.
CONTACTS: Exclusion and stool cultures not indicated i n
absence of symptoms. Contacts who are symptomatic
should be excluded until stools are contained in the diaper
or child is continent and stool frequency is no more than 2
stools above that child's normal frequency for the time the
child is in the program. Stool cultures are recommended for
symptomatic contacts, and these children should be
excluded from school and child care while evaluation is
pending.
Consult with your local health department for advice during
suspected school outbreaks.
Thorough hand hygiene and environmental cleaning is very
important.
Fifth Diseas
e
(Parvovirus B19,
Erythema
Infectiosum)
4–14 days
(Range: 4–21 days)
Contact with respiratory tract
secretions and percutaneous
exposure to blood or blood
products. It can also be
transmitted from mother to baby
during pregnancy.
Once the characteristic rash
appears, the child is not likely to
be contagious and can return to
school.
Distinctive rash characterized by
a vivid reddening of the skin,
especially of the face, which
fades and recurs; classically,
described as a “slapped cheek
appearance.” The rash may have
a lacey appearance on the trunk
and extremities. It can fluctuate
in intensity and recur with
environmental changes,
such as
temperature and exposure to
sunlight, for weeks to months.
Mild symptoms of fever, joint
pain, cough, sore throat, and
headache may occur 7–10 days
before rash.
PATIENT: Exclusion not indicated beyond facility-based
policies about fever.
CONTACTS: Exclusion not indicated. Pregnant women and
persons with weakened immune systems should seek
medical advice.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 2 of10
Sep 2024
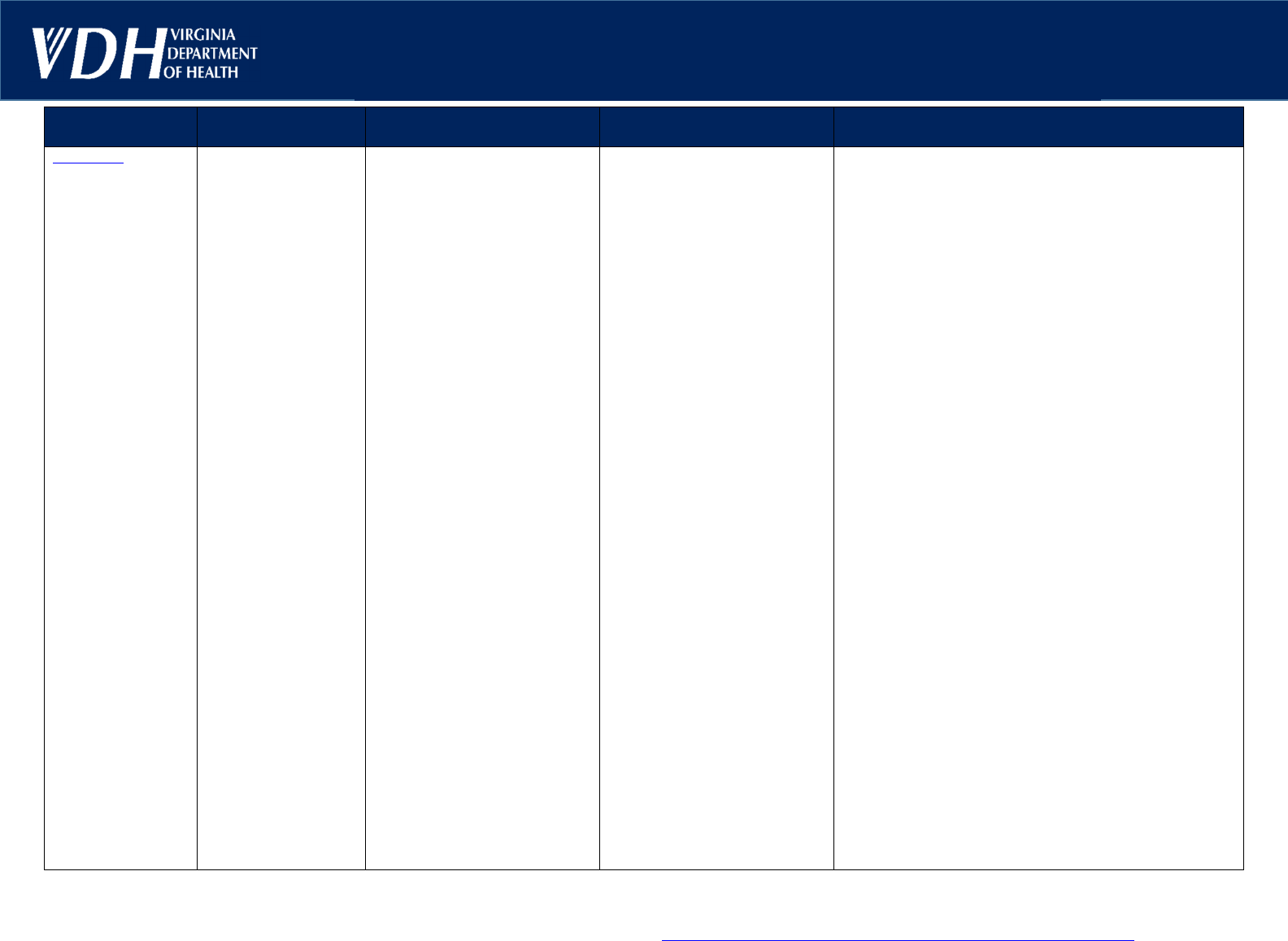
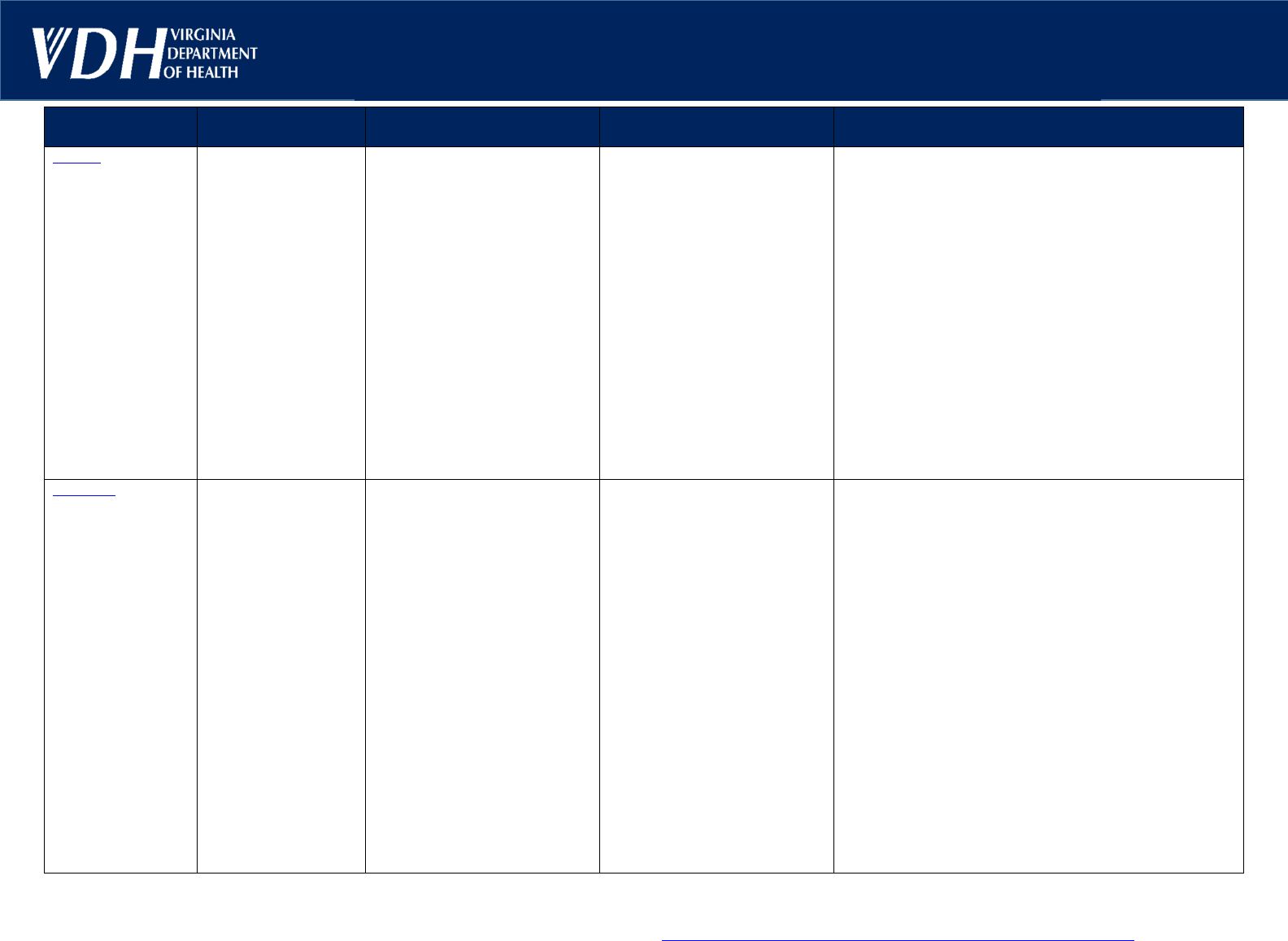
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Hepatitis A
All suspected or
confirmed cases of
hepatitis A are
rapidly reportable
to the local health
department
†
28 days
(Range: 15–50 days)
Fecal-oral route through direct
contact or ingestion of
contaminated food or water.
People with Hepatitis A virus
(HAV) infection are most
infectious during the 1–2 weeks
before illness onset, when
concentration of virus in the stool
is highest. Risk diminishes
significantly by 7–10 days after
symptom onset and is minimal by
the 3
rd
week of illness.
Initial symptoms begin abruptly
and include fever, nausea,
vomiting, diarrhea, fatigue, joint
pain, anorexia, and abdominal
pain or discomfort. Dark urine,
pale stools, and jaundice
(yellowing of the skin or eyes)
might be present initially or might
develop a few days to a week
later. The likelihood of symptoms
increases wit h age.
Symptoms typically last less than
2 months but can extend up to 6
months.
PATIENT: Patients with acute HAV infection who work as
food handlers or attend or work in child care settings should
be excluded for 14 days if symptomatic, or 7 days since
jaundice. If th e person is not a food handler or in a child care
setting, exclude for 7 days after onset of symptoms.
Serologic testing should be performed to confirm HAV
infection in suspected cases.
CONTACTS: Determine if contact is immune to HAV
through immunization records and/or serologic testing (a
positive Hep A IgG). Serologic testing is not typically
recommended if immunization records are unavailable.
Contacts who are immune do not need additional follow-up.
Determine if contact meets criteria for HAV postexposure
prophylaxis (PEP) with Hepatitis A vaccine, immunoglobulin,
or both.
Childcare staff
or attendees who might have been exposed
to HAV in the past 2 weeks should be excluded for 7 weeks
after last contact with the case during the infectious period,
unless they receive PEP within 14 days of exposure or
report immunity through vaccination or serology indicating
previous disease.
Contacts who are symptomatic and epidemiologically-linked
to a laboratory-confirmed case meet the case definition and
should be managed as a case, including appropriat
e
investigation and exclusion.
In a child care center, stress importance of proper
handwashing. In facilities with diapered children, if one or
more cases are confirmed in child or staff attendees or two
or more cases in households of staff or attendees, hepatitis
A PEP should be administered within 14 days of exposure to
all unimmunized staff and attendees.
In centers without diapered children, hepatitis A PEP should
be administered only to unimmunized classroom contacts of
index case. Asymptomatic contacts may return after receipt
of hepatitis A PEP.
If questions about management of cases and/or contacts,
please contact local health department.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 3 of10
Sep 2024
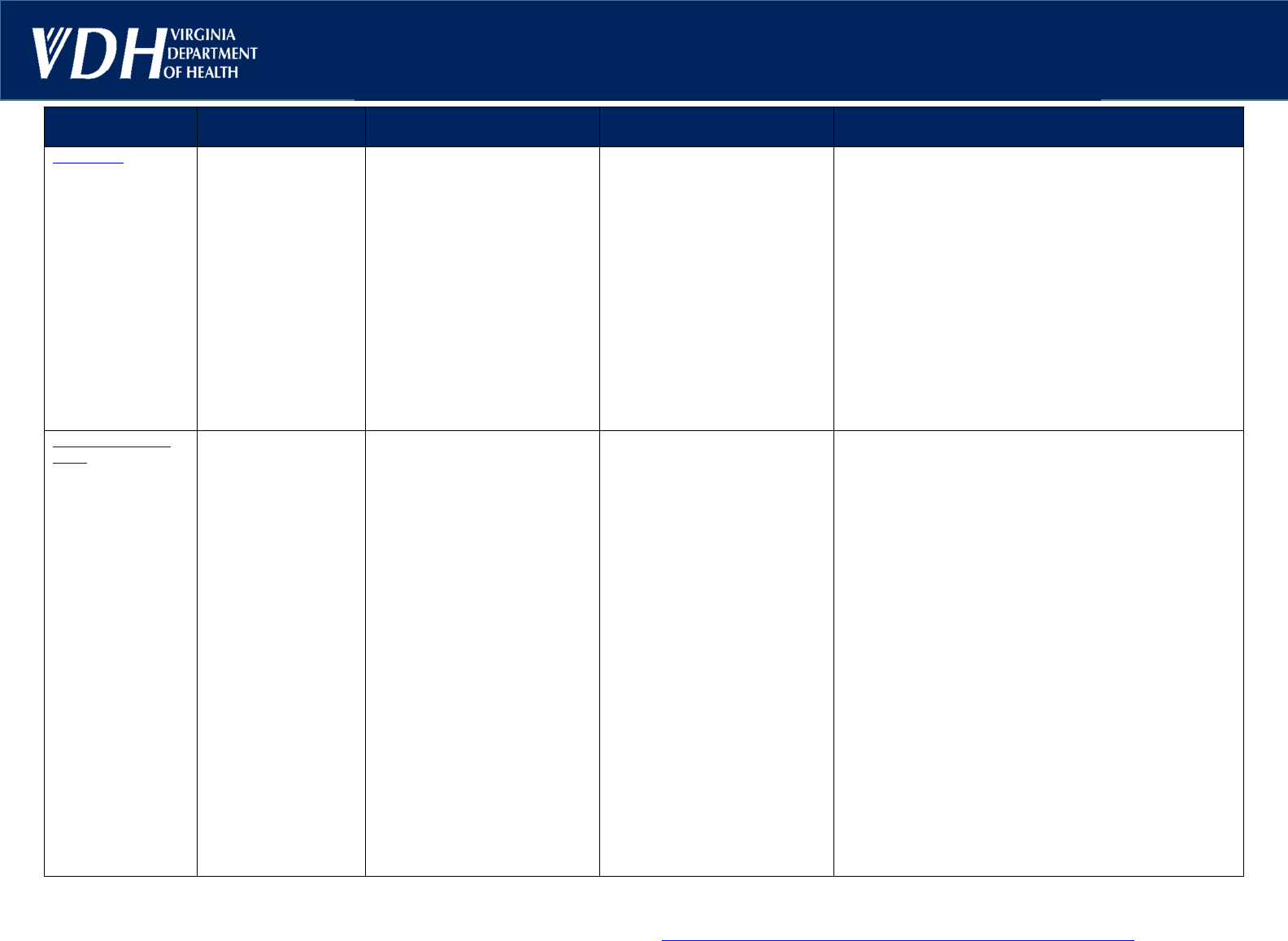
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Hepatitis B
†
60
–
90 days
(Range: 45–160 days)
Direct contact with infected blood
or body fluids. Transmission
occurs when the hepatitis B virus
enters the body through broken
skin or mucous membranes. The
risks of HBV acquisition when a
susceptible child bites a child
who has chronic HBV infection or
when a susceptible child is bitten
by a child with chronic HBV
infection are unknown. A
theoretical risk exists if HBsAg-
positive blood enters the oral
cavity of the biter, but
transmission by this route has
not been reported.
Developing symptoms of acute
hepatitis are age-dependent and
occur most commonly in adults.
The spectrum of symptoms and
signs is varied and includes
subacute illness with nonspecific
symptoms (e.g., anorexia,
nausea, or malaise), clinical
hepatitis with jaundice, or
fulminant hepatitis.
PATIENT: Follow advice of child’s healthcare provider
and/or your local health department.
CONTACTS: Exclusion not indicated.
HIV Infection
and
AIDS (Acquired
Immunodeficiency
Syndrome)
†
†
For untreated infants
and children who
acquire HIV infection
through mother-to-
child transmission, the
usual age of onset of
symptoms is 12–18
months of age. Some
children become ill in
the first few months of
life, but others remain
asymptomatic for more
than 5 years and,
rarely, until early
adolescence.
Acute retroviral
syndrome develops in
40–90% of adults and
adolescents. It occurs
7–14 days following
viral acquisition and
lasts 5–7 days. Most
patients are not ill
enough to seek
medical attention.
1. Sexual transmission (vaginal,
anal, orogenital)
2. Percutaneous blood exposure
(e.g., contaminated needles)
3. Mother-to-child transmission
4. Mucous membrane exposure
to contaminated blood or body
fluids
5. Transfusion of contaminated
blood or blood products, though
this has been virtually eliminated
in the U.S. since 1985
6. Cases of HIV transmission
have been reported from contact
of non-intact skin with blood-
containing body fluids
Clinical manifestations of
untreated pediatric HIV infection
include unexplained fevers,
generalized lymphadenopathy,
hepatomegaly, splenomegaly,
failure to thrive, persistent oral
and diaper candidiasis, recurrent
diarrhea, parotitis, hepatitis,
central nervous system disease
(e.g., encephalopathy,
hyperreflexia, hypertonia,
floppiness, developmental
delay), lymphoid interstitial
pneumonia, recurrent invasive
bacterial infections, and
opportunistic infections (e.g.,
viral, parasitic, and fungal
infections).
PATIENT: Follow advice of child’s healthcare provider
and/or your local health department.
CONTACTS: Exclusion not indicated.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 4 of10
Sep 2024
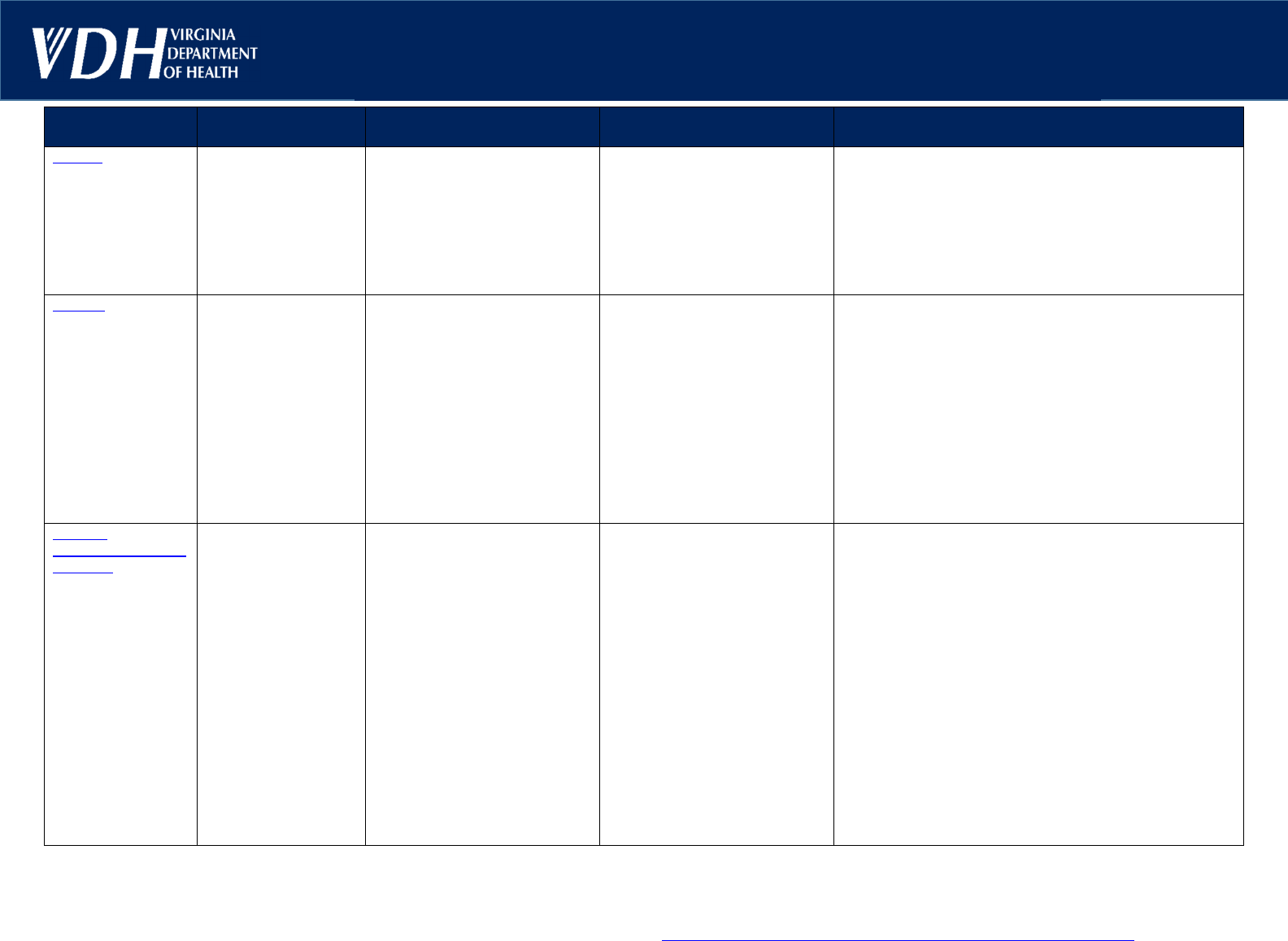
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Influenza
(Seasonal)
Note: Suspected or
confirmed novel
influenza virus
infections should be
rapidly reported to
the local health
department and may
have different
exclusion criteria.
2 days
(Range: 1–4 days)
Respiratory droplets (e.g.,
coughing or sneezing.),
contaminated hands or surfaces
(where it can remain for up to 24
hours), or airborne transmission
via small-particle aerosols in the
vicinity of the infectious individual
Patients may be infectious 24
hours before onset of symptoms.
Viral shedding in nasal
secretions usually peaks during
the first 3 days of illness and
ceases within 7 days but can be
prolonged (10 days or longer) in
young children and people with
weakened immune systems.
Sudden onset of fever, often
accompanied by nonproductive
cough, chills or rigors, diffuse
myalgia, headache, and malaise.
Subsequently, respiratory tract
symptoms, including sore throat,
nasal congestion, rhinitis, and
cough, become more prominent.
Less commonly, abdominal pain,
nausea, vomiting, and diarrhea
are associated with influenza
illness. In some children,
influenza can appear as an
upper respiratory tract illness or
as a febrile illness with few
respiratory tract symptoms. In
infants, influenza can produce a
nonspecific sepsis-like illness
picture, and in infants and young
children, influenza can cause
otitis media, croup, pertussis like-
illness, bronchiolitis, or
pneumonia. Acute myositis
secondary to influenza can
present with calf tenderness and
refusal to walk.
PATIENT: Exclude from school and child care until at least
24 hours following resolution of fever without the use of
fever-reducing medication(s).
CONTACTS: Exclusion not indicated.
Annual seasonal influenza vaccination for staff and children
≥ 6 months of age is strongly encouraged to prevent cases
of influenza or lessen severity of illness.
Measles
(Rubeola, Red
Measles)
All suspected or
confirmed measles
cases are rapidly
reportable to the
local health
department
†
From exposure to
prodrome:
11–12 days
From exposure to
rash onset:
14 days
(Range: 7–21 days)
Direct contact with infectious
droplets or by airborne spread
through inhalation of infectious
droplets when a person with
measles coughs, sneezes, etc.
The attack rate in a susceptible
individual exposed to measles is
90% in close-contact settings.
Patients infected with wild-type
measles virus are contagious
from 4 days before rash onset
through 4 days after appearance
of the rash.
Fever, cough, coryza, and
conjunctivitis, followed by a
maculopapular rash starting on
the face and spreading
downwards and outwards.
During the initial period, Koplik
spots may be present. The
characteristic rash may not
develop in patients with
weakened immune systems.
Koplik spots are typically 1-3mm
whitish, grayish, or bluish
elevations with an erythematous
base typically seen on the buccal
mucosa. Koplik spots are not
seen in all measles cases.
PATIENT: Exclude from school and child care until at least 4
days after appearance of the rash and when the child is able
to participate.
CONTACTS: Check immunization records of all contacts.
Additional measures are not needed for children and/or staff
who are fully vaccinated or have evidence of immunity to
measles. People who have not been immunized, including
those exempted from measles immunization for medical
reasons, should be excluded from school, child care, and
health care settings until at least 21 days after the onset of
rash in the last case of measles. Discuss with your local
health department. Every suspected measles case should
be reported immediately to the local health department.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 5 of10
Sep 2024
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Meningitis, Bact erial
(
H. influenzae
,
Meningococcal
,
Pneumococcal
)
All suspected or
confirmed cases of
invasive H.
influenzae disease
or meningococcal
disease are rapidly
reportable to the
local health
department
†
†
H. influenzae:
2–7 days
Meningococcal:
< 4 days
(Range: 1–10 days)
Pneumococcal:
1–7 days
Respiratory (e.g., coughing or
sneezing) or throat secretions
(e.g., kissing) through close or
lengthy contact.
Transmission can also occur by
sharing beverages, utensils, and
personal care products. Patients
should be considered capable of
transmitting the organism for up
to 24 hours after initiation of
effective antimicrobial treatment.
Acute onset of fever, neck
stiffness, neck pain, headache,
light sensitivity and other
neurologic symptoms or signs.
In meningococcal disease, rash
initially can be macular or
maculopapular but typically
becomes petechial or purpuric
within hours. Signs and
symptoms of meningococcal
meningitis may be
indistinguishable from those
associated with pneumococcal
meningitis.
PATIENT: Exclude from school and child care during acute
illness. Non-communicable after 24–48 hours of appropriate
drug therapy.
CONTACTS: Exclusion not indicated. Discuss with your
local health department to determine if close contacts need
prompt prophylactic treatment for H. influenzae or
meningococcal meningitis, especially contacts in a child
care setting. Students and staff should be advised not to
share beverages, eating utensils, or personal care products.
Mpox
†
(Previously known
as monkeypox)
3–17 days
Symptoms usually
start within 21 days of
exposure to the virus.
If someone has flu-like
symptoms, they will
usually develop a rash
1–4 days later.
Through close contact (including
intimate, sexual, or
household/caregiving contact)
with a perso
n with mpox (e.g.,
skin-to-skin, body fluids,
prolonged talking or breathing,
from mother to baby), and
through contact with
contaminated materials (e.g.,
clothing, bedding), or direct
contact with infected wild
animals.
Mpox can be spread from the
time symptoms start until the
rash has fully healed and a fresh
layer of skin has formed. The
illness typically lasts 2–4 weeks.
People with mpox get a rash that
may be located on the hands,
feet, chest, face, in or around the
mouth, or on or around the
genitals or anus.
The rash will go through several
stages, including scabs, before
healing. The rash can initially
look like pimples or blisters and
may be painful or itchy.
Other symptoms of mpox can
include fever, chills, swollen
lymph nodes, exhaustion, muscle
aches and backache, headache,
respiratory symptoms (e.g., sore
throat, nasal congestion, or
cough).
People may have all or only a
few symptoms.
PATIENT: Exclude from school and child care until the rash
has healed, all scabs have fallen off, and a fresh layer of
skin has formed.
This may take as long as 4 weeks after
symptoms began. Caregivers should work with a healthcare
provider and the health department to decide when the child
or adolescent can return to the educational setting.
CONTACTS: Exclusion not indicated in most cases. In some
cases, if contact tracing may not be possible and there was
a high or intermediate degree of exposure, the local health
department may consider limiting an individual’s
participation in activities. The health department will
consider the age of the individual and their ability to
recognize or communicate symptoms, the types of
interactions in the environment, and the risk of more severe
disease to others in the setting. If a contact had high- or
intermediate-risk exposure, the health department may
recommend postexposure prophylaxis with JYNNEOS
vaccine, ideally administered within 4 days of exposure.
Settings with children or adolescents in residence, (e.g.,
boarding schools, overnight camps, and other residential
environments) follow considerations for congregate settings.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 6 of10
Sep 2024
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Mumps
†
16
–
18 days
(Range 12–25 days)
Contact with infectious
respiratory tract secretions and
saliva. Highly contagious.
The period of maximum
communicability begins 2 days
before parotitis onset. The
recommended isolation period is
5 days after onset of parotid
swelling. However, virus has
been detected in patients' saliva
as early as 7 days before and
until 9 days after onset of
swelling.
Swelling and tenderness of one
or both parotid glands as well as
nonspecific symptoms such as
fever, muscle aches, loss of
appetite, malaise, and headache.
Asymptomatic infection occurs in
about 15-20% of cases, usually
in adults more than children.
PATIENT: In addition to standard precautions, exclude from
school and child care for 5 days after the onset of parotid
gland swelling.
CONTACTS: Determination of vaccination status should be
obtained for all contacts. In an outbreak setting, consult local
health department regarding outbreak management and
whether contacts need to be excluded from school or child
care.
If health department agrees, unimmunized contacts should
be excluded until at least 26 days after onset of parotitis in
the last person with mumps. Excluded students can be
readmitted after receipt of a dose of MMR vaccine at the
discretion of the health department. Moreover, if the school
or child care is considered to be at high risk for mumps, a
recommendation may be made for students and staff who
have had two doses of a mumps-containing vaccine to
receive a third dose of MMR vaccine.
Norovirus
12
–
48 hours Fecal-oral or vomitus-oral route
through direct contact, ingestion
of contaminated food or water,
touching contaminated surfaces,
and aerosolized vomitus.
Viral shedding may start before
onset of symptoms, peaks
several days after exposure, and
in some cases, may persist for
≥4 weeks. Prolonged shedding
(>6 months) has been reported
in people with weakened immune
systems.
Sudden onset vomiting and/or
watery diarrhea, abdominal
cramps, and nausea. Symptoms
typically last from 24–72 hours,
but prolonged illness can occur.
Systemic manifestations,
including fever, myalgia, malaise,
anorexia, and headache, may
accompany gastrointestinal tract
symptoms.
PATIENT: In addition to standard precautions, exclude from
school and child care until 48 hours after symptoms resolve.
This includes resolution of vomiting and diarrhea. Infants
and children should be excluded from child care centers
until stools are contained in the diaper or when toilet-trained
children no longer have accidents using the toilet and when
stool frequency becomes no more than 2 stools above that
child’s normal frequency for the time the child is in the
program, even if the stools remain loose. Stress importance
of thorough handwashing with soap and water, especially
when caring for diapered children, as virus may be shed in
stool for weeks after symptoms resolve.
CONTACTS: Exclusion not indicated.
Environmental cleaning is a very important component of
the response to a norovirus outbreak. A high-concentration
bleach solution can be used—this solution must remain on
the surface for enough time to kill norovirus. Surface must
be rinsed with water to remove bleach residue.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 7 of10
Sep 2024

Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Pediculosi s
(Head Lice)
8–9 days for eggs t o
hatch after being laid
(Range 7–12 days)
Lice mature into adults
about 7 days later.
Direct head-to-head contact wit h
hair of an infected person.
Transmission by contact wi th
personal belongings (e.g.,
combs, brushes, sporting gear,
hats) is uncommon.
Head lice infestation occurs most
commonly in children attending
child care, preschool, and
elementary school, and is not a
sign of poor hygiene.
Severe itching and scratching.
Adults, eggs, and nits (empty
egg casings) are found on the
hair, often seen behind ears and
at the nape of the neck.
Excoriations and crusting caused
by secondary bacterial infection
may occur.
Many children are asymptomatic.
PATIENT: Notify parents; inform that child has lice an d
should be treated. Children should not be excluded or sent
home early from school or child care because of head lice,
because head lice have a low contagion within classrooms.
“No-nit” policies should be discouraged.
CONTACTS: Household and close contacts should be
examined and treated if infested. No exclusion necessary.
Routine classroom or school-wide screening for lice is
discouraged. Parents who are educated on the diagnosis of
lice infestation may screen their own children's heads for
lice regularly and if the child is symptomatic. Refer for
treatment if infested.
Pertussis
(Whooping Cough)
All suspected or
confirmed cases of
pertussis are
rapidly reportable
to the local health
department
†
7–10 days
(Range 5–21 days)
Close contact through large
respiratory droplets generated by
coughing or sneezing.
Catarrhal stage: mild upper
respiratory tract symptoms (e.g.,
common cold). Lasts 1–2 weeks.
Paroxysmal stage: cough,
usually coughing fits,
characterized by inspiratory
whoop (gasping) after repeated
cough on the same breath, which
commonly is followed by post-
tussive emesis. Fever is absent
or minimal. Older children may
not have the whoop. Lasts 1–6
weeks, up to 10 weeks.
Convalescent stage: symptoms
wane gradually over weeks to
months. Lasts 2–3 weeks.
PATIENT: Exclude from school and child care until 5 days
after initiation of appropriate antibiotic therapy. A 5-day
course of azithromycin is usually treatment of choice and is
also used for postexposure prophylaxis. Untreated
individuals should be excluded until 21 days have elapsed
from cough onset. If questions about pertussis treatment or
postexposure prophylaxis, discuss with your local health
department.
CONTACTS: PEP is recommended for all household and
close contacts (including children in child care), people at
high risk of severe pertussis (infants <12 months of age,
people with certain pre-existing conditions), and those who
will have contact with people who are high risk (including all
people in child care settings) regardless of immunization
status.
All close contacts should be
monitored closely for
respiratory tract symptoms for 21 days after last contact with
the infected person. Close contacts with cough should have
medical evaluation. Exclude on first indication of symptoms
pending evaluation by healthcare provider.
Ring worm
(Body: Tinea
Corporis, Scalp:
Tinea Capitis, Groin:
Tinea Cruris, Feet:
Tinea Pedis)
1–3 weeks
Can be shorter, as
reported cases have
occurred at 3 days of
age.
Skin-to-skin contact with lesions
of infected persons or animals,
shared objects (e.g., brushes,
combs, hats, towels), shared
surfaces (e.g., locker room
floors), soil or fomites
Circular, red to brown, well-
demarcated skin lesion(s). May
have a scaly, vesicular, or
pustular border with central
clearing. Small confluent plaques
or papules can occur. Itching is
common.
PATIENT: Exclusion not indicated if child is receiving
treatment. Child does not need to be sent home early from
school but should begin treatment before returning. Cover
lesions if able. (Scalp lesions do not need head coverings.)
CONTACTS: Exclusion is not indicated.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 8 of10
Sep 2024
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
DISEASE
INCUBATION
PERIOD
TRANSMISSION COMMON SYMPTOMS RECOMMENDATIONS
Rubella
(German Measles)
All suspected or
confirmed cases of
rubella are rapidly
reportable to the
local health
department
†
17 days
(Range: 12–23 days)
Direct or droplet contact from
nasopharyngeal secretions.
Most contagious when the rash
is erupting, but communicable for
7 days before onset of rash and
at least 7 days after onset of
rash.
Mild, maculopapular rash wi th
swollen lymph nodes (often
behind ear or at base of skull)
and slight fever. Rash usually
starts on face and spreads to the
rest of the body within 24 hours.
Rash typically lasts 3 days. Joint
pain may occur, especially in
older children and adults.
PATIENT: Exclude from school and child care for 7 days
after onset of rash. Avoid exposure to women in early
pregnancy. Check immunization records of all students.
Discuss with your local health department.
CONTACTS: In outbreak setting, children without evidence
of immunity should be immunized or excluded for 23 days
after onset of rash of the last case in the outbreak. Pregnant
contacts should be evaluated.
Scabies
Persons without
previous exposure:
4–6 weeks
Previously infested
and sensitized:
1–4 days
Prolonged close, personal
contact. Infection from dogs/
animals is uncommon. Casual
skin contact unlikely to result in
transmission. Fomites are not
likely to lead to classic scabies
but can transmit crusted scabies
because the parasite burden is
Intensely itchy, red pimple-like
rash around finger webs, wrists,
elbows, knees, armpits, shoulder
blades, waist, thighs, buttocks
and/or genitalia. In children <2
years of age areas such as the
scalp, face, neck, palms, and
soles may be involved. Burrows
PATIENT: Exclude from school and child care until after the
first course of appropriate treatment has been completed.
Children identified during the school day should not be sent
home early from school or child care because scabies has a
low contagion within classrooms.
CONTACTS: Close contacts with prolonged skin-to-skin
contact should receive treatment at the same time the
much higher. (Crusted scabies is
a severe, very contagious form
that can occur in those with
chronic conditions,
developmental disabilities, or
weakened immune systems.)
are thin, gray or white, thread-
like lines. Extensive scratching
can result in secondary infection.
infected person does. Bedding and clothing in contact with
the skin of infected people should be laundered.
Group A
Streptococcal (GAS)
Diseas
es
(Including Impetigo,
Streptococcal
pharyngitis “Strep
throat”, and Scarlet
Fever)
Impetigo:
7–10 days
Strep throat/
Scarlet Fever:
2–5 days
Impetigo:
Direct contact with skin lesions or
their discharge.
Strep throat/Scarlet fever:
Respiratory droplets or contact
with respiratory secretions.
Fomite transmission and
foodborne outbreaks are
uncommon but can occur.
Impetigo: Red, itchy sores that
break open and leak clear fluid or
pus, then develop a honey-
colored crust. Commonly found
on the arms, legs, mouth and
nose.
Strep throat: Sudden onset of
fever, sore throat, tonsil
inflammation, palatal petechiae,
strawberry tongue, and enlarged
anterior cervical lymph nodes.
Scarlet Fever: A sandpaper-like
rash that occurs with strep throat
(or rarely with an infected
wound).
PATIENT:
Impetigo: Exclude from school and child care until
at least 12 hours after antibiotic treatment has started and
all sores on exposed skin are covered. Close contact with
other children should be avoided during this time.
Strep throat: Exclude from school and child care until 12
hours after appropriate antibiotic therapy has been started
AND afebrile without the use of fever-reducing medications
(e.g. acetaminophen or ibuprofen).
CONTACTS: Impetigo: Exclusion not indicated.
Strep throat: Symptomatic contacts should be medically
evaluated and treated if positive. Routine lab testing or
school/child care exclusion of
asymptomatic household
contacts is not indicated except during outbreaks or if the
contact is at high risk of developing sequelae of infection. In
general, chemoprophylaxis against Group A Strep is not
recommended in school/child care settings.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 9 of10
Sep 2024
Communicable Disease Reference Chart
for School and Child Care Facility Personnel
*
Summary of Major Changes in the August 21, 2024 Update:
Reviewed and updated content for all diseases using the Control of Communicable Diseases Manual, 21st Edition (2022) published by the American Public Health
Association, the 2021-2024 Report of the Committee on Infectious Diseases, 32nd Edition (The Red Book) published by the American Academy of Pediatrics, and the
relevant CDC website.
Added link to Virginia Reportable Disease List in footer: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf.
Updated information in the footer about consultation with the LHD, especially for outbreaks and reportable conditions, and added information on school-specific policies.
Added link to CDC website for each illness, if available.
Updated language from “immunocompromised” to “people with weakened immune systems”
Chickenpox – updated to indicate that incubation period may be shorter in those with weakened immune systems, added more details about the rash, updated language
regarding vaccination and exclusion of contacts
COVID-19 – added language about variants, updated isolation and quarantine guidance
Fifth Disease – added additional information about the onset of rash and infectious period
Hepatitis A – updated exclusion criteria
Hepatitis B – updated incubation period
Influenza – clarified that recommendations only apply to seasonal influenza; added a note about novel influenza virus infections.
Measles – updated incubation period with information about prodrome and rash onset
Mpox – updated transmission information, exclusion criteria, and information on postexposure prophylaxis
Mumps – updated contact exclusion criteria to indicate that students can be readmitted after receipt of a dose of MMR vaccine at the discretion of the health department.
Pertussis – updated clinical description to include stages of illness; updated PEP recommendations to align with CDC
Ringworm – Expanded from ringworm of the body to ringworm in general, which may include the scalp, groin, or feet. Updated exclusion guidance.
Salmonellosis – updated incubation period
Streptococcal Diseases – standardized language across the row to “strep throat” for “strep pharyngitis”
Summary of Major Changes in the February 21, 2023 Update:
Conjunctivitis (Pink eye) – Expanded from “acute bacterial” conjunctivitis to “all causes,” removed the requirement to be on antibiotics to return to school/child care, and
added clearance by a healthcare provider to return while symptomatic.
COVID-19 – Aligned transmission information with the Centers for Disease Control and Prevention (CDC). Removed information on close contacts.
Fifth Disease (Parvovirus B19) – Added information about the characteristic rash.
Hepatitis A – Clarified length of exclusion for patients who are food handlers and those who work in or attend child care.
Mpox – Updated disease name from “monkeypox” to “mpox.”
Pertussis – Aligned PEP recommendations for contacts with CDC recommendations.
Rubella – Updated exclusion of unimmunized contacts from 21 days to 23 days.
Streptococcal Diseases – Changed exclusion criteria from 24 hours of antibiotics to 12 hours of antibiotics for impetigo, and to 12 hours of antibiotics AND afebrile for strep
pharyngitis.
NOTE: THESE RECOMMENDATIONS APPLY ONLY TO CHILDREN IN K-12 SCHOOLS OR CHILD CARE - A more complete discussion of these conditions and other communicable diseases may be found in Control of Communicable Diseases Manual, 21
st
Edition
(2022) published by the American Public Health Association and the 2021-2024 Report of the Committee on Infectious Diseases, 32
nd
Edition
(
The Red Book) published by the American Academy of Pediatrics. Additional information and consultation are also available
through your local health department, especially for outbreaks and reportable conditions. School divisions may develop local policies for condition-specific recommendations.
*Please see last page for a summary of major changes.
†
Officially reportable in Virginia to the local health department. All disease outbreaks and unusual occurrences of disease are also reportable: https://www.vdh.virginia.gov/content/uploads/sites/134/2023/03/VIRGINIA-REPORTABLE-DISEASE-LIST.pdf
Page 10 of 10
Sep 2024
