
1
AMSER
GUIDE
TO
APPLYING
FOR
RADIOLOGY RESIDENCY
VERSION
12
–
JULY 2023
Updated
with
the
latest
statistics
and
information
on
Diagnostic and Interventional Radiology Residency
INTRODUCTION
Contributors: Atul Agarwal
1
, Garrett Barfoot
2
, Biren A. Shah
3
, Kathryn W. Zamora
4
1
Indiana University School of Medicine,
2
Ross University School of Medicine (Medical Student),
3
Detroit Medical Center/Western
Michigan University Homer Stryker M.D. School of Medicine,
4
The University of Alabama at Birmingham
TIMELINE
Contributors: Atul Agarwal
1
, Garrett Barfoot
2
, Biren A. Shah
3
, Kathryn W. Zamora
4
1
Indiana University School of Medicine,
2
Ross University School of Medicine (Medical Student),
3
Detroit Medical Center/Western
Michigan University Homer Stryker M.D. School of Medicine,
4
The University of Alabama at Birmingham
GENERAL
ADVICE
ABOUT
APPLYING
TO
RADIOLOGY
RESIDENCIES
Contributors: Vikas Agarwal
1
, Peter Haar
2
, Anugayathri Jawahar
3
, Shivam Khatri
4
, Nisa Cem Oren
5
, Donna
Magid
6
, Biren A. Shah
7
, Chris Straus
8
, Carissa White
9
, Aaron Wyse
10
1
University of Pittsburgh Medical Center,
2
Virginia Commonwealth University School of Medicine,
3
Northwestern University,
4
The City
University of New York School of Medicine (Medical Student),
5
University of Chicago Medical Center,
6
John Hopkins Medicine,
7
Detroit
Medical Center/Western Michigan University Homer Stryker M.D. School of Medicine,
8
University of Chicago Medical Center,
9
Penn
State Health,
10
The Mayo Clinic Arizona
WHAT
MAKES
A
SUCCESSFUL
APPLICANT
AND
HOW
SHOULD
I
PREPARE?
Contributors: Vikas Agarwal
1
, Peter Haar
2
, Anugayathri Jawahar
3
, Shivam Khatri
4
, Nisa Cem Oren
5
, Donna
Magid
6
, Biren A. Shah
7
, Chris Straus
8
, Carissa White
9
, Aaron Wyse
10
1
University of Pittsburgh Medical Center,
2
Virginia Commonwealth University School of Medicine (Medical Student),
3
Northwestern
University,
4
The City University of New York School of Medicine (Medical Student),
5
University of Chicago Medical Center,
6
John
Hopkins Medicine,
7
Detroit Medical Center/Western Michigan University Homer Stryker M.D. School of Medicine,
8
University of Chicago
Medical Center,
9
Penn State Health,
10
The Mayo Clinic Arizona
HOW
TO
APPLY
FOR
A
RADIOLOGY
RESIDENCY
Contributors: Peter Haar
1
, Anugayathri Jawahar
2
, Jason Kim
3
, Donna Magid
4
, Biren A. Shah
5
, Natalie Stratemeier
6
,
Kathryn Zamora
7
1
Virginia Commonwealth University School of Medicine,
2
Northwestern University,
3
California Health Sciences University (Medical
Student),
4
John Hopkins Medicine,
5
Detroit Medical Center/Western Michigan University Homer Stryker M.D. School of Medicine,
6
OU
Health – University of Oklahoma Medical Center,
7
The University of Alabama at Birmingham
SO
YOU
GOT
THE
INTERVIEW, NOW
WHAT?
Contributors: Peter Haar
1
, Anugayathri Jawahar
2
, Jason Kim
3
, Donna Magid
4
, Biren A. Shah
5
, Natalie Stratemeier
6
,
Kathryn Zamora
7
1
Virginia Commonwealth University School of Medicine,
2
Northwestern University,
3
California Health Sciences University (Medical
Student),
4
John Hopkins Medicine,
5
Detroit Medical Center/Western Michigan University Homer Stryker M.D. School of Medicine,
6
OU
Health – University of Oklahoma Medical Center,
7
The University of Alabama at Birmingham
ONLINE
RESOURCES
Contributors: Peter Haar
1
, Anugayathri Jawahar
2
, Jason Kim
3
, Donna Magid
4
, Biren A. Shah
5
, Natalie Stratemeier
6
,
Kathryn Zamora
7
1
Virginia Commonwealth University School of Medicine,
2
Northwestern University,
3
California Health Sciences University (Medical
TABLE OF CONTENTS

2
Student),
4
John Hopkins Medicine,
5
Detroit Medical Center/Western Michigan University Homer Stryker M.D. School of Medicine,
6
OU
Health – University of Oklahoma Medical Center,
7
The University of Alabama at Birmingham

2
This document is intended to give you guidance when considering or applying to a residency in
radiology. It includes answers to the most common questions that advisors have been asked, as
well as some “hard data” from the national websites. Some advice reflects the personal opinion of
the authors.
The following is general information about the specialty and the sort of personalities that tend
to enjoy it as a profession.
Resource: Careers in Medicine® (CiM)
Choose Your Specialty Radiology-Diagnostic
1. You can be a general or a multi-specialist radiologist, or specialize in
one or more areas, e.g., pediatric radiology, neuroradiology, ultrasound,
emergency radiology, body imaging, chest radiology, musculoskeletal
radiology, breast imaging, women’s imaging, nuclear medicine, interventional
radiology (IR), etc. Initial training in radiology is general – and area(s)
of subspecialty training can be decided upon after several years in
residency. In private practice, you will probably do general radiology,
possibly with an emphasis, and in academic radiology, you will
probably work in one area or only a few areas. IR is a dedicated pathway
which is determined in advance of other subspecialties in radiology
residency (See section on “How Long is Radiology Training”).
2. Subspecialties vary as to their level of patient contact - from little to
significant. Individuals can gravitate towards what they personally prefer.
3. Subspecialties vary in regard to the percentage of procedures vs.
interpretation.
4. There are opportunities, even in private practice, for those who enjoy teaching
and research, e.g., by being affiliated with or by volunteering at an academic
center.
5. Radiology is evolving as new and improved modalities become available.
6. Radiologists are rarely bored – they deal with a wide variety of modalities
and pathology.
7. Vacation and salary packages in radiology tend to be good, and it has
been one of the higher-paid specialties. It is difficult to give a figure as it
depends widely on the area of the country, years of service and private
vs. academic practice. Vacation may range from 4-13 weeks.
INTRODUCTION
WHY RADIOLOGY?
3
8. Teleradiology gives some radiologists the ability and flexibility to work
100% remotely from home or in a hybrid work model.
9. Radiologists tend to be happier with their career choices than many other
professionals.
10. There are opportunities to work and volunteer internationally.
What kind of people enjoy radiology?
1. People who are “task-oriented” do well in radiology. Did you like to do
problem sets in high school?
2. People who enjoy the consultative medical role, “a physician’s physician” with
considerable range of pathology and work across all medical specialties.
3. People who can make informed decisions and “move on” do well – we
make many more “disease/not disease” decisions during a working day
than most specialties.
4. People who enjoy puzzles and mysteries, and the problem solving,
analytical nature of the profession.
5. The stereotype of the “visual learner” (although that includes most people!),
including those who love anatomy, and seeing disease processes “in life.”
6. People who like surgical procedures but don’t want to be a surgeon. Many
radiology subspecialties do procedures in addition to IR.
7. People who enjoy continual change and new advances, often
technical/computer with “cool toys.” Technical/computer whizzes love the “cool
toys” as part of the job. The ability to produce spectacular images…but most of
us are not computer geeks, we work with medical physicists and experts as
needed!
8. People who want to be able to work part-time, given we work as consultants
and in groups, allows for shifts and ability to be flexible when you are “on.”
9. People who don’t mind that other physicians “get the credit” for the diagnosis or
treatment, especially from the patients. This is changing as there are more
“radiology clinic” models where the patients talk to the radiologist about their
studies.
We know that radiology is not everyone’s cup of tea! Some aspects to consider:
1. Longer residency compared to primary care specialties. Almost all radiologists
do a fellowship, which also adds training time.
2. More independent study time required than in most other specialties, where you
learn “on the job” by direct patient interaction.
WHY NOT RADIOLOGY?

4
3. More study time required due to the breadth of knowledge required, i.e., all
organ systems and diseases.
4. More study time required throughout career to keep up with new technologies
and trends. (Are we seeing a pattern?)
5. Variable patient interaction and follow up.
BUT: specialties such as women’s imaging and IR have significant
patient contact and designated clinics. “Radiology clinics” are becoming
more popular and direct patient impact is becoming more evident year
over year.
6. More physician consultation time – your workday is often balancing several
activities, exam production, physician consultation and interpretation, leading
to shifting expectations or interruptions.
7. A desirable trait is work efficiency. Need to have focused attention over
extended periods of time to be able to read 50 head CTs or 100 chest x- rays.
8. Imaging represents a large part of the cost of healthcare costs, anticipate
changes in reimbursement in future years, i.e., salary support.
9. Radiology is a “24/7” subspecialty.
10. Competition with other specialties regarding imaging.
BUT: this tends to fluctuate over time.
Quite often students do not get exposed to radiology until their third or fourth year of medical
school. As a result, students may have a hard time deciding whether radiology is a specialty
to consider as a career. The timeline illustrated below is an ideal guideline, however, it is
important to realize that even if you decide as late as mid-summer, or even fall, in your 4th
year of medical school that you wish to apply to a radiology residency program, it is not “too
late.” In these situations, it is important to seek out guidance and mentorship at any point in
the process. Most importantly, do not assume you are at a huge disadvantage. Generally,
students overestimate the negative – get informed with quality information before making
assumptions.
GENERAL
• Job one: Study hard!
° We can’t underestimate the value of having a solid knowledge
base… and doing well on USMLE Step 2 and/or COMLEX (for
D.O. students), shows you are diligent and likely to succeed in
FIRST YEAR OF MEDICAL SCHOOL
TIMELINE

5
residency.
Despite Step 1 (and COMLEX 1) now being pass/fail, the value of studying for and
passing Step 1 cannot be overstated as serving as a base of foundational knowledge.
° You will have greater options – i.e., you won’t be shut out of any
specialty if you have a solid Step score.
• Be well-balanced:
° Join student interest groups to learn about different fields. You
aren’t obligated to pursue a particular specialty just by checking
it out.
° Check into the availability of a Radiology Interest Group at your
medical school and consider joining RadSIG. If there is not a current
radiology interest group, consider starting one.
° Get involved with one volunteer/charity organization.
° While prioritizing performing well academically and adjusting to
the rigors of medical school, if after a semester or two you feel
you have the capacity, consider joining student government,
curriculum committees, engaging in peer tutoring, or becoming a
teaching assistant for subjects such as anatomy. Although such
opportunities are potentially better suited for later years of
medical school, they may not exist at your institution
following basic sciences, so becoming involved early on may be
important.
• Join professional radiology societies including different radiology
subspecialty societies:
° Many radiology societies are free or have only a small
membership fee for students.
° Looks good on residency application, reinforces general
awareness, and demonstrates interest in the field - e.g., Radiological
Society of North America (RSNA), Association of University
Radiologists (AUR)
• Get to know the field of radiology: (See: “WHY NOT RADIOLOGY?” section)
° Radiology is a consultation field that needs a deep and broad
knowledge base. The specialty has been responsible for all imaging
breakthroughs and is far from stagnant. Our efforts often reflect
continually changing modalities, workflow, and techniques. It is a field
that requires a serious commitment and acceptance to consistent
studying to maintain skills and stay current.

6
° Shadow radiologists and talk to residents to get to know the field. If
there are radiology faculty advisors at your school, take time to meet
with them. Do not hesitate to seek advice from other resources if your
school programming does not have options locally.
° For schools that do not have a dedicated academic radiology
department, one may look into seeking mentorship from past alumni
that are radiologists or radiology residents. In addition, one can seek
out mentorship at radiology meetings (e.g. RSNA, AUR, etc.).
SPRING
• If you’re not involved in a research project already, begin to look for a project
for the summer. Programs like to see that you have the discipline and interest
to do research – and it does not have to be in the field you finally decide on.
At some point you may have an opportunity to do research in the specialty
you choose. A research project will:
° Broaden your experience and knowledge of the field.
° Provide opportunities to present your work at a conference and
even submit it for publication.
° Help you work closely with a faculty member, who can write you a
strong letter of recommendation. (see “LETTERS OF
REFERENCE” section)
° If your medical school does not have a dedicated academic
radiology program, finding a mentor through AUR, RSNA, AMSER,
RRA, etc. may be one of the only ways to find a comparable
research opportunity. Another option is making a connection with an
alum who is willing to involve a M1 student on a project.
• Have a game plan for your research project.
° Assess your interests, unique skills, inclinations, and shortcomings.
° Look for major radiology society national meetings: Radiological
Society of North America (RSNA), Association of University
Radiologists (AUR), American College of Radiology (ACR), Society
of Interventional Radiology (SIR), American Roentgen Ray Society
(ARRS), etc.
° Approach a potential research mentor with a CV or summary of
your experiences and skills.
° Exercise ingenuity and initiative in finding a project. Start early
and be persistent.

7
Pick your research mentor wisely: this is one of the most crucial
factors in being productive.
♦ Ask around for research opportunities and be
persistent until you find one. If one doesn’t work or
the timeline doesn’t seem right, consider pursuing
another one.
e.g., email the student director(s) in areas of radiology
you are interested in for suggestions. They often
circulate emails in the department.
♦ It may help to confirm that the attending you
picked has been productive recently.
♦ Do not expect the attendings to have menus of
instantly available projects ready to go.
♦ You may present your own ideas and ask for
mentorship.
° Projects listed as “in progress” or “submitted” do not yet officially
exist
♦ Show initiative in finishing a project – try to set a goal
with your mentor, such as an exhibit or presentation
at a national conference, rather than vague “research.”
♦ Consider doing several projects, with different mentors, as
you may not know which ones will be fruitful.
SUMMER
• If you have done a research project already (paper, exhibit), you may
do something else that will strengthen your application, e.g., working
abroad on a medical mission, volunteer work, charity work.
• Summer Stipends - there are multiple opportunities so apply for these.
° Check with your Dean's Office.
° Check with professional societies: e.g., RSNA, AUR, Alliance of
Medical Student Educators in Radiology (AMSER), Society
Nuclear Medicine (SNM), National Institute of Health (NIH), etc.
• If you haven’t done so, consider shadowing radiologists, in several
specialties.
• Enjoy this summer - this is also a great time to travel and have fun.
• If your school does not provide a break between 1
st
and 2
nd
year, the
opportunities listed here must be completed concurrently with coursework

8
during 1st/2nd year, or during the break/gap between basic sciences/Step 1
(COMLEX 10 and the start of clinical sciences.
GENERAL
• Continue to be active in your interest groups and other extracurricular
organizations. Become an officer of a group, e.g., the Radiology Interest
Group.
• Continue your “summer” research or start another project.
• Schedule your 3rd year rotations.
° Schedule early rotations in areas of your interest - to confirm or
reject areas. But don’t panic if you can’t take it early or you don’t
have a 3rd year radiology rotation at your school – most students do
not! It is not about factual knowledge you have learned, radiology
programs assume you know very little when you arrive, it is entirely
about you feeling both comfortable and confident that the career is
a great fit.
° If your school does not have a radiology residency program it likely
has hospital affiliations at a site that has a program. Planning 3
rd
year
rotations at a site with a radiology residency program could
potentially offer a few distinct advantages:
♦ Increasing your exposure to the field of radiology.
♦ Increasing your exposure to that respective radiology
program and its residents, faculty, coordinators, and
advisors.
♦ Providing opportunities to develop long-standing
relationships with residents and faculty by working on
radiology-specific projects, which could lead to a strong
letter of recommendation.
♦ Allowing ample time for radiology project completion,
publication, presentation, etc. BEFORE the match
application/interview cycle begins the Fall of fourth year.
° If radiology is a 4
th
year rotation, to get exposure in radiology, you
should:
♦ Follow up your patients’ radiological studies on other
rotations.
SECOND YEAR OF MEDICAL SCHOOL

9
♦ Shadow radiologists/talk to radiology residents if you
haven’t done so already.
♦ Stay involved with interest groups, if possible.
° *Special note for International Medical Graduates (IMGs):
Sometime during the last semester of M2 year, students need
to begin the ECFMG application and certification process with
their school. This ensures that upon completion of M2 year,
there are no unnecessary, delays and registering for and taking
Step 1, and transitioning into M3 year. Oversights with ECFMG
requirements/procedures and/or coordination with your medical
school can create significant delays.
HOW TO STUDY FOR STEP 1:
• Not all students take Step 1 in June of their second year due to changes in the
medical curriculum, it could be in January of the second year or much later.
• Study hard during year 1 and year 2. Grades and Step exam performance do
count.
° Despite Step 1 now being pass/fail, it is important to study equally
hard for this test, not only to pass it, but also because doing well lays
a solid foundation for your clinical years.
° January Year 2: Begin to review material from year 1, with your
priority being to do well in class.
° Once classes end in year 2, take 4-5 weeks for the intensive Step 1
studying.
° Take a few full exams to assess where you are and what you should
concentrate on.
° For at least 3 weeks before the exam, go to bed early (e.g., 10p),
wake up at 6a, take multiple sets of 1-hour exams – so you simulate
the exam day and improve your endurance.
• What to use for studying:
Pick a few resources and stick to them.
Use these while studying for the first- and second-year exams. For example:
° Online question bank
♦. USMLE World
° National Board of Medical Examiners (NBME) website
♦ Mini-tests that use real questions, which may
appear on the real test
♦ Timed and give you a score report – correlates well
to end score

10
° Rapid Review Pathology by Edward Goljan
° First Aid for Step 1 - good review resource, but not enough material
or detail.
° A well-known acronym for resources utilized by many successful
medical students to aid with both basic sciences and Step 1 is
"UFAPS"; Which stands for:
U - U-World
F - FirstAid
A - Anki (The “AnKing" deck specifically)
P - Pathoma
S - Sketchy
The “AnKing”deck specifically utilized images, mnemonics, and
explanations from each of these high-yield resources with a built in
spaced repetition tool to maximize retention.
° Note for D.O. students: While taking Step 1 and/or 2 is/are no
longer required in addition to the COMLEX-USA to enter the Match,
it is strongly encouraged to take Step 1 and Step 2 due to the
growing competitive nature of the field. Programs with osteopathic
students may “know” the conversion of COMLEX performance to
USMLE scores. However, having a (strong) USMLE score may give
you more options. Historically, students who achieved an excellent
score on USMLE Step 1 are likely to be favored over those who took
only the COMLEX exam. It remains to be seen what programs will
prefer now that Step 1 is pass/fail.
GENERAL
• 3rd year rotations:
° Start reading the weekend before the start of the rotation, so you
don’t come in like a “deer in headlights”.
° Read a short textbook (200-300 pages) rather than go deeply into
literature about particular cases.
° Radiology residencies look for excellent grades in the core rotations.
• How to do well in 3rd year:
° Work and study hard to get honors, especially in medicine and
surgery, if you can.
° Consider talking to several students who got into the AOA (Alpha
Omega Alpha) national medical honor society to see if any of their
strategies might work for you.
THIRD YEAR OF MEDICAL SCHOOL

11
° The grading system for year 3 is subjective. The grade is based on a
combination of your evaluation and a “shelf” exam (multiple choice
tests taken by all students nationally).
♦ Always show up on time, be enthusiastic, offer to help,
ask a lot of appropriate questions, and try to learn as
much as you can.
Stand out from the crowd - do more than “just pass.”
♦ Study hard, like you did in years 1 and 2, for the “shelf”
exams.
° If this is your first opportunity to be under the same roof as an
academic radiology department, take advantage of that! Outside of
the time needed to earn honors marks in your current rotation, make
an effort to get to know the radiology residents and faculty at time and
places that are convenient for them. Express interest, ask questions,
ask for advice, and see if there are any projects (research or
otherwise) that you might be able to help with.
• Letters of Reference (see “Letters of Reference” section):
° If you do well in a rotation, ask for a letter right away so your attending
still has details fresh in their minds and will be able to write a more
personal letter. It’s best if they offer an unsolicited letter, but at any
rate, ask if they feel comfortable in writing a strong letter.
• Plan your 4th year schedule
° Ask current 4th year students at your school, especially students that
matched into radiology, as to how, where, and why they scheduled
their 4th year schedule and what they would have done again or
changed. Talk also with your faculty advisor.
° If Radiology is not a year 3 rotation at your school, apply early for
year 4 radiology clerkships - July or August. If you can’t get one,
meet with the radiology clerkship director to explain your interest in
radiology. (see “WHEN SHOULD I TAKE MY RADIOLOGY
CLERKSHIP?” section)
° With Step 1 now being pass/fail, planning the timing of “WHEN” to take
Step 2 following completion of 3
rd
year core rotations/shelf exams is
important. Give yourself enough time to get your Step 2 score back
before the application/interview season begins in the Fall of 4
th
year.
12
SPRING/EARLY SUMMER
• Contact the Radiology faculty advisor (and any other areas that you
are interested in) and arrange a preliminary meeting to discuss your grades
and career plans.
• Set up an email account that sounds professional and one that will roll over
when your school email closes if it does not have an alumni account.
• Schedule a physical exam and update immunization records and titers,
including varicella, in case needed.
• Check the website of programs you are interested in to see if they require
anything special.
• Get a letter that you are in good academic standing from academic affairs.
• Update your CV: make it professional-looking and 1 page, longer only if
multiple publications.
° Summarize research, including citations for all your publications –
another page if needed.
° Summarize hobbies/interests to add dimension to your profile.
• Start working on your Personal Statement (see “PERSONAL STATEMENT”
section) – 1 page only
• Begin filling out your ERAS
®
Application Worksheet
° This includes up to 3 geographic preference essays, setting
preference or lack of preference essays, and up to 3 most
meaningful essays. This may take some time to complete.
° Presume much of what you write and early versions will never be
seen by others. The greatest benefit is you starting to formulate
coherent answers and self-awareness used in interviews later in the
process.
° A great personal statement reflects new information not necessarily
present in the general application. A read through should generate
meaningful adjectives with which you would want to be labeled. It is
your opportunity to present more information/skills/qualities
otherwise lost to an application reviewer in the more traditional
required sections.
• Photograph for applications
° Play it safe: look professional and show that you understand the
unwritten conventions.
Don’t give anyone the chance to say, “what was he/she thinking….”
No weird stuff. No pets. No significant others.
° The photograph will be used during ranking to help remember who is
who so make sure it looks like what you will look like on the day of
your interview (clothes, hairstyle, facial hair etc.)

13
° Pleasant smile – reshoot if needed.
° Head-and-shoulders only.
° Send as jpeg, not too low or high resolution so it prints as ~ 3x4 cm.
Away rotations: (see “AWAY ROTATIONS” section)
Consider scheduling at a place where you think you may want to do residency: at a
target, not a “reach” or “safe” place.
*Special note for D.O. and IMGs: The NRMP match data as well as school-specific
match data can provide valuable insights into which programs are “IMG-friendly” or
“D.O.-friendly” programs, and historically match competitive applicants from your
school. This can aid you as an applicant to set appropriate expectations/goals,
strategically plan away, rotations, and be judicious in your expenses related to
application fees.
“Meet the Experts” get-together
Many schools arrange a meeting or dinner for interested 3rd year students with
the matched 4th year students (they are the REAL experts in this!) for an
information exchange session. If this does not occur at your school, start one
by contacting the Radiology faculty advisor (also a great thing to add to CV, in
addition to being valuable for you and your classmates). Students who have
participated in these get-togethers have found them incredibly useful. Make it
informal, e.g., over pizza.
Remember: You are being evaluated at all times at these activities so don’t
criticize other people or places, gossip, or get drunk.
Also remember you have something to sell - yourself - so be confident.
Mock Interviews
Given the current situation of residency interviews being virtual, it is highly
recommended to practice interviewing. Check with your medical school if
mock interviews are offered. Otherwise, you can set one up with a faculty
member you don’t know so they can give you feedback.
SUMMER
• If possible, do a Radiology Clerkship/Selective/Elective if you have not done
so previously. HOWEVER, do not fret if you are not able or allowed. You are
far from alone. It is about self-awareness – not having “radiology activity on
your transcript” – that is what is needed.
FOURTH YEAR OF MEDICAL SCHOOL
14
• Meet with the Radiology faculty advisor to discuss your draft personal
statement, letters of reference and program application lists (see sections
below). Consider doing Sub-internship or Acting Internship in medicine or
surgery early during 4th year.
° Can boost your grades/evaluations if needed.
° Can yield a strong letter of recommendation, if needed.
° Often required for transitional year or preliminary year applications.
ERAS (Electronic Residency Application Service)
• You can register and start working on your residency application on June 8.
• ERAS timeline
MEDICAL STUDENT PERFORMANCE EVALUATION (MSPE)
• Schedule a meeting for your Medical Student Performance Evaluation
(MSPE) with your dean.
TRANSCRIPT
Check your transcript to make sure all of your grades have been submitted
and submitted correctly. Don’t let that HONOR you earned get transcribed
as a PASS. If you are missing grades, contact the department secretary
and use gentle encouragement: “Is there any additional information I can
provide to help my evaluator complete this?”
Plan to take Step 2
• See “WHEN SHOULD I TAKE STEP 2” below.
SEPTEMBER/OCTOBER
Diagnostic Radiology participates in the NRMP Match.
SUBMIT APPLICATIONS AS SOON AS POSSIBLE ON OR AFTER SEPTEMBER 6.
RESIDENCY PROGRAMS START RECEIVING APPLICATIONS ON SEPTEMBER 27.
It shows how motivated and enthusiastic you are about applying to residency.
• Many programs grant interviews on a rolling basis. The earlier you apply, the
greater the chance you have of being considered for interviews.
• Make a tentative calendar, making blocks of time for each region you plan on
interviewing in. Though grouping interviews by region is less important in
current times, given virtual interviews, you may still find it helpful in comparing
neighboring programs. The earliest programs start sending out interview offers
in late September or early October.
15
OCTOBER/NOVEMBER
• MSPEs are released September 27 along with MyERAS applications and
supplemental ERAS applications (if applicable).
• Be strong! You may feel crushed when those rejections start to come (possibly
by the end of October or the first two weeks of November)… and then the
interview invitations start rolling in.
• Interview offers will come in more steadily until the end of November/beginning
of December. California programs usually send out interviews later - often in
December.
• Schedule as many interviews in November as your schedule allows, enabling
greater flexibility later.
• Do not write off a program even if you do not hear from them by December.
• No news means you are still on the list. Applicants cancel interviews so
programs may contact you even at the last minute. Always be available to take
an interview offer. (See “WHEN YOU CAN CONTACT A PROGRAM
DIRECTLY” section)
NOVEMBER/DECEMBER
Take a vacation. You want to present your best self at interviews. You want to have
time to exercise, rest, and eat well. You’ll want to have time to research the program
beforehand.
Interview season: late October - early February, with the peak in late November to mid-
January. Schedule flexible rotations, e.g., online course, research, self-study, flexible
clerkships. Consider using vacation/discretionary time in November, December, or both
months. If you are unable to take vacation/discretionary time off, ensure that you are on a
rotation that gives you flexibility to take time off for interviews.
LATE JANUARY-FEBRUARY
• Make your rank list: set up meeting with advisors to help with rank
order. (see “RANKING PROGRAMS” section )
FEBRUARY-APRIL
• Consider taking BLS/ACLS early so you won’t have to take it at the
last minute before internship (and you might get that time off during
internship orientation).

16
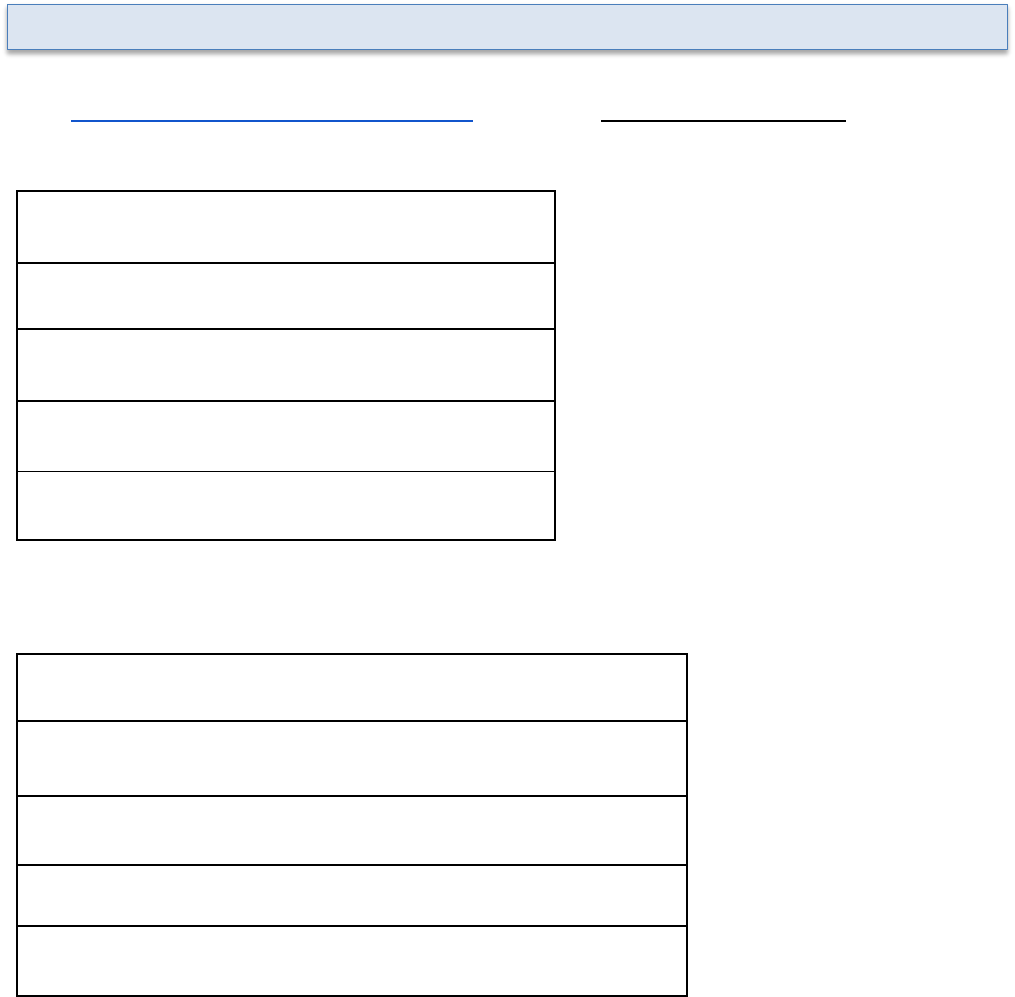
MARCH-MAY
“Meet the Experts Meeting” - Arrange a meeting with the other 4th years to celebrate,
commiserate, and share with Radiology faculty advisor and 3rd years about what you
did right or wrong.
Contact radiology faculty advisor
As soon as possible, or by March of Year 3
Meet the Experts” Dinner/Meeting
March/April, Year 3
Group Meeting with radiology faculty
advisor
April-July, Year 3
Mock Interviews (can arrange if not
offered)
May-October, Year 3-Year 4
Radiology Clerkship/Selective/Elective
If not in the Year 3, take early in Year 4
Draft personal statement, geographic
preference(s) essay(s), and most
meaningful experience essay(s)
June/July, Year 4 (send to advisors/friends)
Final personal statement
July/August, Year 4
Develop program lists
July/August, Year 4, discuss with faculty
advisor or dean
ERAS application submission (NRMP
Match)
September 6, Year 4
STRONGLY RECOMMENDED on day 1
ERAS applications close
Variable
MSPE released
End of September, Year 4
Interviews
November to January, Year 4
Rank list entry open
Mid-January
Rank list entry close
Mid-February
Did I match?
Mid-March, Monday
Match day
Mid-March, Friday
SUMMARY TIMELINE (VARIES WITH SCHOOL)
17
• As soon as you are considering radiology as a career, meet with the
radiology faculty advisor at your school. If there is no official faculty
advisor, meet with the radiology clerkship director and/or the
residency program director.
• If you are in your 1st or 2nd year of medical school with a diagnostic
radiology residency program, the advisor can direct you to a PGY-2
radiology resident to discuss the field (and the application process)
with you, and the advisor can help set up opportunities to shadow
radiologists and to get involved in research.
• When shadowing, ask about procedures. There are many types of
procedures that are done outside of Interventional Radiology by
Diagnostic Radiologists.
• Be honest with your advisor: Does something personal or professional
need addressing?
Diagnostic Radiology Residency – 5 years
Application methods:
• Most common application method (PGY 1 + PGY 2-5): apply separately
for the intern year and advanced radiology program
° One year in a preliminary internal medicine, transitional year, or
preliminary surgery program – PGY 1 applied separately from
the advanced radiology program.
° Four years in advanced diagnostic radiology PGY 2-5, start at
PGY 2 at the same or different institution from the intern year.
• Less common application method (PGY 1-5): Categorical programs: PGY
1 intern year and the PGY 2-5 radiology residency are combined and
applied to as one at the same institution.
Diagnostic Radiology Fellowships – 1 year
• Most radiology residents complete 1 year of fellowship training.
• Most common fellowships are: Abdominal imaging, breast imaging,
cardiothoracic imaging, musculoskeletal imaging, neuroradiology (1 to 2
years), nuclear medicine, pediatric radiology, and women’s imaging.
GENERAL ADVICE ABOUT APPLYING TO RADIOLOGY RESIDENCIES
WHEN SHOULD YOU CONTACT THE MEDICAL STUDENT RADIOLOGY FACULTY
ADVISOR?
HOW LONG IS RADIOLOGY TRAINING?

18
• Though the above fellowships are diagnostic radiology categories,
many, including musculoskeletal, breast, abdominal, etc., involve
procedures unique to those subspecialties.
Interventional Radiology – 6 to 7 years
Overview of IR training options outlined in chart form here:
(https://www.sirweb.org/learning-center/ir-residency/) as well as described below.
• Integrated IR Residency
° Apply for during year 4 of medical school
° 1 year of internship (usually preliminary surgery), 5 years of
residency, 6 years total
° https://www.sirweb.org/learning-center/ir-residency/integrated/
• Independent IR Residency
° Apply and match into DR residency as a medical student
° Apply for independent IR residency during year 3 or PGY-4 of DR
residency
° Complete 2 years of Independent IR residency after DR
residency graduation
° 1 year of internship, 4 years of DR, 2 years of IR, 7 years total
° https://www.sirweb.org/learning-center/ir-
residency/independent-ir-residency
• Early Specialization in Interventional Radiology (ESIR)
° Apply and match into DR residency as a medical student
° DR residency must have associated IR residency and ESIR
designation
° Within the program, apply to ESIR during year 1 or 2 of DR
residency
° Transition into ESIR
° 1 year of internship, 4 years of DR with ESIR, 1 year of IR, 6
years total
° https://www.sirweb.org/learning-center/ir-residency/esir/
• Some academic radiology departments may offer additional options such
as research tracks. Check individual program websites.
How do I apply to different types of programs?
• The majority of DR and IR programs are for advanced positions
(start as PGY2) and do not include the intern year. You would
apply for and rank the intern year separately.

19
• There are some programs that include the intern year (categorical),
for which you do not need to interview separately.
• You need to apply for DR and IR programs separately.
• If you are applying to a diagnostic radiology residency, a general
diagnostic radiology clerkship/elective is critically important. This can
help to confirm your interest in the field, help you to meet faculty, and
potentially get a letter of recommendation.
• Take it as early as possible, if available in your 3
rd
year. This will confirm
your interest in radiology and help you get involved in relevant activities.
Do an elective in interventional radiology if you are applying to IR residency. You may
consider doing this as an away elective.
Additional radiology electives after doing an initial radiology experience may be
considered:
• Help confirm or deny interest if you are still tentative.
• Show potential programs your interest in a particular region –
especially in a region you may want to move to, to which you may not
have apparent ties.
• Increase your potential sources for letters of reference. However, most
programs will be more interested in strong letters from your non-
radiology clerkships, such as internal medicine and surgery.
If you do an additional radiology elective, you should:
• Do a subspecialty elective rather than repeat the basic elective, e.g.,
neuroradiology, interventional radiology, women’s imaging. Take a
musculoskeletal radiology elective if you were previously interested in
orthopedics, or a breast imaging elective if you are wondering about a
more procedure and patient interaction-heavy specialty besides IR.
° You will likely have more personal interaction and will get to know
the radiologists better (good for letters of reference – see
“LETTERS OF REFERENCE” section). Remember, the
goal of electives is to solidify your interest, make connections
with faculty and get LORs.
° Subspecialty rotation reads better on your transcript.
WHEN SHOULD I TAKE MY RADIOLOGY CLERKSHIP?
WHAT OTHER ELECTIVES ARE THERE IN RADIOLOGY AND SHOULD I TAKE THEM?
20
• Consider a research elective in radiology. This is an opportunity to get to
know a radiology mentor better (good for letters of reference—see
“LETTERS OF REFERENCE” section). It will also allow you to produce
something from it – e.g., a paper, case report, poster, abstract, teaching
module.
• Consider a different institution to get a different perspective and
experience (see “AWAY ROTATIONS” section) and to let them get to
know you.
Don’t do more than one extra radiology elective because:
• You have the rest of your life to do radiology. You do not NEED to start
learning radiology before residency.
• Other electives will broaden your understanding of medicine
and make you a more interesting candidate.
• This might be your last chance to do something outside of
radiology.
It will be more beneficial for you to take a non-radiology elective than a second radiology
elective.
• Consider rotations that will expose you to the broadest understanding of what
referring clinicians do and ultimately become more aware of what and how a
radiologist can support fellow physicians in alternate specialties. Radiologists
serve patients and clinicians, so the better we understand what they are doing
day-to-day, the better we can support clinicians as an effective consultant.
• Take advantage of your elective time to explore that other niche non-radiology
specialty such as ophthalmology or radiation oncology to make sure you don’t
like it better.
• Take a research elective with a radiology mentor to build your
CV.
• If you are interested in IR, consider a vascular surgery elective
to see the difference between the two.
• Take an elective that will help prepare you for internship.
Away radiology rotations are not necessary. Not all programs take outside students. Away
rotations can be a double-edged sword:
• Pros
WHAT NON-RADIOLOGY ELECTIVES SHOULD I CONSIDER?
AWAY ROTATIONS
21
° You get insight into what the program is like, and what it is like
living in the region.
° The program gets to know you well and it shows your interest in
the program.
° It may get you an interview when you might not have been
offered one based solely on your application – yet historical
data shows this is not likely. There are very few interviews
granted out of kindness.
• Cons
° No guarantees for interview or matching.
° It is like a month-long interview: you will be compared to the best
student they’ve ever had.
° If you go: Optimize your performance. Be first in, last out. Dress
professionally.
Spend your evenings looking things up, preparing, and studying.
° Comments from all house staff are likely to be incorporated, so you
are not just “on” with attendings or specific attendings.
° If you do poorly, you lose only one of your potential interviews. We
have all had students who have been great for the first couple of
days (a.k.a., an interview), but didn’t look so good after 4 weeks.
Where to do the away rotation:
• In an area of the country in which you must match. You can consider getting
a letter from the program to send to that particular geographic area.
• At an institution you’re particularly interested in. This should be a high
“target” program where you are likely to get an interview and you want
to maximize your potential at matching at the program - not at a “reach“
program that you are unlikely to get into.
What - Do your homework:
• Talk to students or residents with ties to the program; look online to
identify appropriate meaningful queries/questions about the program.
• Identify your area of interest/ability, and an area which will expose you to the
residents, program director, or other people vital to the selection process.
• If you are planning to do research there, set it up ahead of time so you’ll hit
the ground running.
• Consider a subspecialty away elective. It is important to use your elective
time to expand your experience rather than repeat it.

22
When
• Latest by October of Year 4. You might be offered an interview if you
are there in November or December but don’t count on it. Consider
what it will look like if you leave an away elective to interview at another
program.
How
• Multiple institutions participate in AAMC’s Visiting Student Application
Service
• If the ones you want do not, then you have to apply through the institution
directly.
• Many schools temporarily halted their in-person radiology electives during
the COVID-19 pandemic. Most also stopped accepting visiting students at
that time. However, now that the pandemic has subsided, many schools
have chosen to continue their virtual electives. Refer to AAMC Visiting
Student Learning Opportunities (VSLO) for a list of schools offering virtual
radiology electives and for application information.
Keep in mind:
° Virtual electives are for your own educational benefit, don’t
expect them to be helpful to your residency application.
♦ While it may be tempting to apply for these electives as
audition rotations, they will likely not provide the faculty
interaction necessary to boost your application of
generate LORs.
♦ The virtual electives also may or may not involve
interaction with residency and give you a feel for the
program.
° If at all possible, do a radiology rotation in person. If your school
doesn’t offer a radiology rotation, you can apply for in person
away rotations through VSLO, although these are harder to
succeed/stand-out on, as discussed above. You can also take
advantage of shadowing opportunities at your home institution.
Repeat shadowing and long-term relationships with radiologists
will be more helpful to your application than a virtual radiology
elective.
VIRTUAL ELECTIVES
23
° In your application and during the interview process, you need to
be able to strongly articulate your interest in radiology and
convince the program that you have what it takes to succeed as
a radiologist. If you have any doubts, take a virtual elective as
your last resort to solidify your interest, again, not to boost your
application.
° If you have already done in-person radiology electives and need
a flexible elective during interview season, virtual electives may
be a good option.
• You will likely have an orientation to your radiology elective. Make sure
you understand the expectations and specifics such as: time to arrive
each day, dress code, how you will be evaluated, etc.
• Whenever you enter a radiology reading room, politely approach each
person and introduce yourself. If possible, start with a resident. (Most
radiology programs have resident and faculty rosters posted online, or you
can get one from your rotation coordinator.)
° If the person is actively dictating, the proper etiquette is to wait
until they have finished and signed off the exam rather than
interrupt.
° Say, “Hi! I am [your name]. I am a __ year medical student on
my [radiology elective name]. I want to learn as much as
possible. Who should I sit with or what should I do to learn the
most and be the most helpful?”
***Most important- Always be interested! ****
• Ask questions.
° A good question pace is every other cross-sectional study or
once every 10 minutes. You don’t want to interrupt the workflow
too often.
• Offer to look up clinical history in the EMR or differential in a book or
online resource if you are sitting with a resident.
•. If there is an interesting case, make note of the case and follow up on
imaging or pathology reports and inform the attending radiologist or
resident the next time you see them. This makes a positive impact that
you care and are invested in learning.
APPROPRIATE BEHAVIOR ON THE RADIOLOGY ELECTIVE

24
• Ask if you can observe procedures and if there is anything you can do to
be helpful while in the room.
° Introduce yourself to the patient as a medical student and ask if
they mind you observing.
° Ask a follow-up question AFTER the procedure.
• Ask if there are any educational conferences or tumor/interdisciplinary
boards you can attend.
° If attending a tumor board, consider asking to present a
patient.
• At the end of the day or whenever leaving, be sure to thank each person
for their time.
• Look for opportunities while on the rotation to participate in research
projects that you can accomplish; for example, you can write a case report
(do not be over ambitious since not being able to follow up to completion
will act against you). Most programs will appreciate if you complete it even
after the rotation is over and score more points during the interview.
• Be genuine.
• High rank in the first 2 years, good grades in the clinical years, high Step
2/COMLEX scores, research experience, strong letters of reference, a
solid personal statement, your overall personality and how you present
yourself at the interview are all important.
• According to NRMP’s 2022 3
rd
ed. Chartering Outcomes in the
Match: Senior Students of U.S. MD Medical Schools, the
average of matched Diagnostic Radiology US MD senior
candidates are:
° STEP 1 – 244 (Step 1 scores disappear in 2023-2024
application cycle; applicants with pre-2023 Step 1 on record
will likely see that score be considered)
° STEP 2 – 253
° AOA members – 19.3%
° Abstracts, presentations, and publications – 8.0
• According to NRMP’s 2022 3
rd
ed. Chartering Outcomes in the
Match: Senior Students of U.S. DO Medical Schools, the average of
matched Diagnostic Radiology US DO senior candidates are:
° COMLEX-USA Level 1 score - 625
WHAT MAKES A SUCCESSFUL APPLICANT AND HOW SHOULD I
PREPARE?

25
° COMLEX-USA Level 2-CE score - 661
° STEP 1 – 242 (Step 1 scores disappear in 2023-2024
application cycle; applicants with pre-2023 Step 1 on record
will likely see that score be considered)
° STEP 2 – 250
° Abstracts, presentations, and publications – 3.9
• According to NRMP’s 2022 3
rd
ed. Chartering Outcomes in the
Match: IMG MD Medical Schools, the average of matched
Diagnostic Radiology IMG MD candidates are:
° STEP 1 – 241 (Step 1 scores disappear in 2023-2024
application cycle; applicants with pre-2023 Step 1 on record
will likely see that score be considered)
° STEP 2 – 247
° Abstracts, presentations, and publications – 7.0
• According to NRMP’s 2022 3
rd
ed. Chartering Outcomes in the
Match: Senior Students of U.S. MD Medical Schools, the average of
matched Interventional Radiology US senior candidates are:
° STEP 1 – 245
° STEP 2 – 253
° AOA members – 20.8%
° Abstracts, presentations, and publications – 12.2
• According to NRMP’s 2022 3
rd
ed. Chartering Outcomes in the
Match: Senior Students of U.S. DO Medical Schools, the average of
matched Interventional Radiology US DO senior candidates are:
° COMLEX-USA Level 1 score – 646
° COMLEX-USA Level 2-CE score – 664
° STEP 1 – 244 (Step 1 scores disappear in 2023-2024
application cycle; applicants with pre-2023 Step 1 on record
will likely see that score be considered)
° STEP 2 – 254
° Abstracts, presentations, and publications – 7.8
• According to NRMP’s 2022 3
rd
ed. Chartering Outcomes in the
Match: IMG MD Medical Schools, the average of matched
Interventional Radiology IMG MD candidates are:
° STEP 1 – 261
° STEP 2 – 270
° Abstracts, presentations, and publications – 5.0
• While the NRMP data above is a snapshot of past data, the
components to a successful applicant matching into Diagnostic
Radiology are continually shifting and it is about “the complete
package” of an applicant to demonstrate the qualities that make
a future great radiology colleague.
26
• Doing things you enjoy is important - if you are an interesting person,
happy and self-confident, and feel good about yourself, this will show
when you work on the wards and when you interview.
Increasingly medical schools are not including class rank in the MSPEs. In combination
with Step 1 now pass fail, this means that quantifiable data to screen applicants is
decreasing and therefore Step 2 scores will become increasingly important.
The 2021 NRMP Program Director Survey shows that Diagnostic Radiology program
directors, for invitations for interview, give the highest importance to:
1. USMLE STEP 1 score
2. Medical Student Performance Evaluation
3. Letter of recommendation in specialty
4. Grades in required clerkships
5. Personal statement
For ranking of the candidate for the Match, they give the highest importance to:
1. Interactions with faculty during interview
2. Interactions with house staff during interview and
visit
3. Interpersonal skills
4. USMLE STEP 1 score
5. Feedback from current residents
WHAT PROGRAM DIRECTORS ARE LOOKING FOR

27
The top priority for programs is interactions with faculty and residents during interview, as
emphasized in 4 of the 5 important factors listed above. This is because radiology is a 4-year
training period and programs need good candidates who are easy to work with rather than
just smart residents who might be difficult to work with on a daily basis.
The 2021 NRMP Program Director Survey shows that Interventional Radiology program
directors, for invitations for interview, give the highest importance to:
1. Letters of recommendation in the specialty
2. USMLE STEP 1 score
3. Medical Student Performance Evaluation
4. Personal Statement
5. Perceived commitment to specialty
For ranking of the candidate for the Match, they give the highest importance to:
1. Interactions with faculty during interview
2. Interpersonal skills
3. Interactions with house staff during interview and
visit
4. Perceived interest in program
5. Perceived commitment to specialty
We suspect that in the absence of Step 1 scores, Step 2 scores will ascend in
importance.
28
General information: Overall Radiology is a competitive specialty choice but comparing to
other specialties using known metrics is mildly problematic. Students are already somewhat
self-selective and are not equivalent. It may be best to identify and consider personal traits
that are endemic to the specialty and their role in the patient care. Within this larger
framework a student may be interested in trying to determine their personnel relative rank,
yet this is equally limited. It is best to converse with a radiology adviser or mentor, given
many candidates have skills and advantages not properly captured by the standard metrics
such as board scores or class ranking.
It is important to be able to demonstrate why you as a candidate represent a better option as
a future resident. That is skills, capacity, interests, and future goals are not captured in
traditional scores and clinical clerkship grades. The following more traditional measurements
are outlined but not to be considered absolute.
The parameters are changing so that it might be best view the most recent NRMP data.
HOW IMPORTANT ARE YOUR BOARD SCORES?
• While DR residency programs may not have a specific minimum score
to grant an interview, many may use Step 2 board scores as a
threshold to screen applicants for an interview since Step 1 results is no longer
reported as a numerical score. Currently, we are unsure how this change will
affect Program Directors’ preferences.
• Don't let a slightly lower score scare you away from applying if you have an
otherwise strong application. However, it is important that you talk with a
radiology faculty advisor, so that you are realistic in your goals and have made
back-up plans.
WHEN SHOULD I TAKE USMLE STEP 2?
• With Step 1 score now disappearing, we believe Step 2 will likely become its
surrogate and be closely scrutinized for applicant stratification. However,
performance on core clerkships will also play more of a factor in the
comprehensive review of an applicant’s application.
• Aim high, so take a month off (or a less rigorous elective if you’re more
confident). Use something like USMLE World questions.
• It takes about 3 to 4 weeks to get the Step 2 score.
• If Step 2 results are released before you submit the ERAS application,
results cannot be withheld.
• If the scores come after the ERAS application submission deadline, you are not
obligated to release these scores, but do so if you score well.
HOW COMPETITIVE IS RADIOLOGY?

29
So…
• Prepare for and take Step 2 EARLY, in July or August. But take it only when
prepared.
Since Step 1 is now pass/fail, we anticipate that Step 2 will likely be required at the time
of the ERAS application.
DO I NEED TO DO RESEARCH?
Research is a priority, especially at competitive and academic programs, as it shows
that you are proactive and a contributor. While publications are not mandatory, they will
greatly increase your competitiveness for matching at these programs. There are also
many strong programs that are more clinically oriented and may put little to no
emphasis on research.(See “TIMELINE” First Year of Medical School section)
• The average number of abstracts, presentations, and publications for matched
DR and integrated IR applicants are 6.4 and 10.3, respectively (NRMP’s 2022 3
rd
ed.
Charting Outcomes in the Match: Senior Students of U.S. MD Medical Schools).
• It is great if the research is related to radiology, but it doesn’t have to be, i.e., in
the case of a late decision.
• Rigorous scientific pursuits and publishing in any field have much in common
and show dexterity and experience.
• Although it is best to start in year 1, it is not too late, even in July of year 4 –
you can do something short.
° Case reports
° Exhibits/ Abstract presentations at regional/national/
international conferences
♦ Educational/Scientific
♦ Case of the Day (e.g., ACR Case in Point)
♦ Interesting Case Submission (AMSER)
° Educational resources – e.g., programs, websites that the
department of radiology is producing.
• If you started research or published something after you submitted your application,
submit a brief summary of this to the programs you’ve applied to and take this to the
interview. If you publish after the interview, you should send this to the programs as
well. (See “WHEN CAN YOU CONTACT A PROGRAM DIRECTLY?” section)
Research is helpful but not an open mandate or required.
• With all applicants and applications, you goal is to appear as desirable and
beneficial to the selection committee. All applicants and the best applicants are
not identical.

30
• Your goal is to demonstrate as many of the desirable skills needed as a trainee.
These skills however vary between sites and types of programs; that is larger
academic programs place a higher value on elements of the application which
pertain to their greater mission. This concern may not be as significant for a
community-based program or where faculty are not personally pursuing
research routinely.
Where does research fit into the application process?
• It demonstrates skills and awareness of the scientific profession not
easily demonstrated in other venues.
• It shows your capacity and interest to further the quality of care our profession
brings to patients.
• It also can show whether you’re open to challenging questions and
assisting in finding solutions.
Research topics and options are numerous - too much so to list, given that no one area
is more or less important.
• The deeper benefit is more about how the experience affected you.
• What this means however remains open - it does NOT have to necessarily
be research in the field of radiology. You can easily make your case about
personal interests morphing with time and schooling - what is key is having
gone through the process of doing research or a scientific presentation, such
as: identifying a needed question, formulating a project, collecting evidential
support and presenting it; either as an oral/poster presentation or written article.
• Ability to or demonstration of communicating and sharing your knowledge is as
much of the process - showing you’re more experienced than another
applicant.
• Research shows that you as an applicant have more dimension and skills to
share with others.
Research as a member of a group
• Being a part of a larger team is also beneficial.
• Not all work needs to be a personal project and understanding how you can be
a member of a larger challenge and assist are skills with value too.
• The real question each applicant needs to ask and ponder is: How did the
experience affect you?

31
Research performed with a mentor or advisor
• Being a member of an authorship group also can provide you with access to
potential mentors and letter writers.
• Consider your role or roles in the process (or if multiple projects) consider what
skills you have learned and or have following the experience.
• These new skills/elements are most important over the actual science or results
presented.
• What an application reviewer is most interested in and trying to gauge is
whether you are likely to repeat and redeploy these skills downstream as well
as whether you will represent their program well in the future.
What if you don’t finish the project or succeed in presenting or publishing the work?
• Clearly any effort that is completed is more valuable than incomplete or
“conceptual.” It is a question of seeing an effort through to its finish line and
generally, Program Directors want house staff that won’t leave things undone.
• These self-generated projects are a great gauge of personal traits.
• If you have unfinished efforts - you’re far from alone. There are many causes of
derailment. Do not place blame or give excuses; focus on what positives were
achieved - possibly and most importantly - self-reflection and personal insights
learned.
HOW IMPORTANT ARE EXTRACURRICULAR ACTIVITIES?
• Better to do one extracurricular activity in depth than many superficially.
• An interest group and some type of volunteer/charity organization is a great
start.
• Being an officer or having a leadership position is even better.
• Traditionally, as in many fields, many groups were and still are
underrepresented. Virtually every program in the country is working to address
this.
• There are only a few military programs in the country so it is difficult to
determine how competitive these may be in any one year. Generally military
programs are less competitive than the non-military programs.
DIVERSITY IN THE APPLICANT POOL
WHAT ABOUT MILITARY MATCHING?

32
• Strongly consider doing an away elective at these programs.
• Programs vary widely as to whether they take osteopathic students: some do
not or rarely interview DO candidates and others welcome them. Students
should look at the "track record" of a program (how many DO students have
been matched in the last few years) and may consider taking an elective at
programs of interest, particularly at allopathic institutions that may not know
their osteopathic school well.
• DO candidates should get involved in research to be competitive with their
allopathic colleagues.
• Programs with osteopathic students may “know” the conversion of COMLEX
performance to USMLE scores. However, having a (strong) USMLE score may
give you more options. Consider taking USMLE Step 1 and 2 exams as well as
COMLEX. Students who achieved an excellent score on USMLE Step 1 are
likely to be favored over those who took only the COMLEX exam. It remains to
be seen what programs will prefer now that Step 1 is pass/fail.
Students from international medical schools, US-IMG or non-US-IMG, can consider applying
to radiology residency programs. They share the same disadvantages with the osteopathic
students, as detailed above. High USMLE scores (in particular, USMLE Step 2), radiology
experiences in the USA, and strong support from a mentor are critical for their successful
match.
• They should obtain their ECFMG certifications before their graduation with
high USMLE scores.
• They should experience general radiology practice in the USA with elective
clerkship, subinternship, or observership programs specifically in academic
centers.
• They should prove their fundamental medical knowledge and
communication skills while they are in their rotation as well as being a
good team player is another key for their success.
• They should get involved in research in the radiology field to improve their
CVs as well as their network.
Letters of recommendation supporting their application from their native country are
WHAT ABOUT OSTEOPATHIC STUDENTS?
WHAT ABOUT INTERNATIONAL MEDICAL GRADUATES?

33
acceptable, however, letters from clerkships or research fellowship programs in the US
are preferred. If obtaining letters of recommendation from one’s native country, it is
advisable to request the letter writers to upload them to the ERAS website as waived
letters rather than candidates uploading them as unwaived recommendation letters.
In the past, applicants from other specialties who have decided to go into radiology have
successfully matched into radiology. It is understood that a career choice made as a third-
year student sometimes does not work out. Programs do vary as to their interest in these
candidates. Experience in another field can be an advantage to some programs.
The applicant’s personal statement should definitely address the reason(s) for this change of
heart. Also, it will help if their current program is supportive and writes strong letters of
reference. The student MUST have at least one current LOR. However, this is a double-
edged sword if the program is not supportive.
Applicants who change specialties more than once are at a disadvantage.
Applicants who fail to match into radiology the first time around can be successful in
matching in the next application cycle.
• For repeat radiology applicants, see “I DIDN’T MATCH, WHAT SHOULD I
DO?”
• If you are applying into radiology after failing to match into another
specialty, you MUST convince program directors that you are sincere and
sure of your new choice. If radiology is just a fall back because it seems
easy, program directors will see through that.
° Try to get a radiology elective your last month or two of medical
school.
° If you matched into internship: Ask your internship coordinator if
you can do a radiology elective EARLY, either at your internship
institution or at your medical school program as an “away”. For
the latter, you will need to contact the radiology residency
program director and/or radiology advisor at your medical school
ASAP for approval and to help facilitate – especially if your dates
don’t align with the medical school rotation schedule.
WHAT ABOUT APPLICANTS WHO ARE IN OTHER SPECIALTIES?
WHAT ABOUT REPEAT APPLICANTS

34
These resources, most of which offer opinions based on years of observation and
experience are in the end subjective editorialized opinions and do not necessarily
reflect official policy or AUR/AMSER’s stances:
• BeMo's Ultimate Guide to Residency Personal Statements: How to
Write Compelling Statements Even If You are Not a Natural Writer
• APPS of STEEL on Teamrads.com
Being mainstream and “safe” here is OK but make it personal and engaging.
• Have a lot of people read it, including those who read a lot of them
° Friends and family
° Advisors in student affairs
° Radiology faculty advisor
• Basic language skills are required: SOUND LITERATE
° It should be readable with short sentences and no
spelling/grammatical errors, no factual errors
° Proofread well - don't trust spell-check
° It should be concise & coherent
° No more than one page, ¾ is fine. A paragraph is too short!
° Original & eloquent is welcome, but less important
• Being interesting and witty, with a “hook” to draw the reader in, is of course
desirable.
• Don’t assume it will get read but make the first couple sentences good in
case it does. Not all programs read them at the initial ERAS review stage.
• Keep in mind that someone skimming the statement may read only the first
line of each paragraph.
• It can be based on one or more stories that illustrate your life. You
want to sell yourself and show personality.
• ERAS will allow you to select a different personal statement for each
program.
° It will increase your odds of getting an interview at certain
locations, if you include a few lines on why you want to go to the
area or to a specific program – i.e., family lives there, significant
other is there/going there, grew up there, want to live there in
the future, etc., why a New Yorker might go to Texas or vice
HOW TO APPLY FOR A RADIOLOGY RESIDENCY
PERSONAL STATEMENT

35
versa. The Supplemental application may replace this but will be
new for 2023.
° BE CAREFUL – don’t send the wrong statement to the wrong
program.
WHAT TO WRITE ABOUT:
Your essay puts a face on the applicant.
Cast yourself in the most flattering light while being honest – be humble yet assertive.
• Things that do not appear elsewhere on your application.
• Something interesting about yourself or your background that we can talk
about at interviews.
• What attracts you to radiology? Make this short - the readers already know
the “pros” of radiology!
• What you intend to do in radiology.
• What you can bring to the program – e.g., special skills.
• Something outstanding from undergraduate years or outside interest, e.g.,
Olympic swimmer.
• Programs want applicants who want to come to their program to stay there,
so you can make this clear.
• If you have clearly changed career paths, explain why.
• If you have low scores and have a valid reason, explain why, as this will most
probably be asked in the interview. If you think you do not have a strong
reason to validate, it is preferable not to include in the statement as this can
also be detrimental to your interview.
• Problems to address - “odd things” in application – years out of medical
school, prior residencies (why are you changing), etc.
° If you are changing residencies specifically, have concrete
reasons why you know now that radiology is the right fit for
you. Show that you have done your homework either by
participating in research projects and/or by shadowing
radiologists and that you know what working in radiology
entails. Don’t just use generic phrases like “I enjoyed going
to the reading room during my “___” residency and that’s
how I know that radiology is for me.”
DON’T:
• Put anything in that you can’t/don’t want to talk about at interviews.
Anything that you put in your application is fair game for interview material!
• Mention your love of photography or puzzles.
• Tell us you are a “visual learner.”
• Make your personal statement weird – do not stand out in a bad way.

36
• Sound pompous, arrogant, or tactless.
NEVER LIE!
Can a personal statement be too short?
Although we say that you should keep your essay short, this is an example of
(a real but anonymous) personal statement that is a tad too short:
“When I was trying to decide which specialty to apply to, I asked various
physicians how they had chosen their medical specialty. Some described
having an initial interest in several specialties, then deducing the best fit for
their personality. Others related a personal experience that had directed them
toward a specialty. A single respondent stated, “It wasn’t a choice. I just knew.”
Like the latter respondent, I just know. I know who I am. I know what I do well.
I know what I do poorly. And I know that I am a radiologist.”
Personal statements are preferably kept within one-page length; however, it is
advisable to not be shorter than 3 paragraphs.
An example outline could be:
• First paragraph: The most important paragraph that grabs the
attention of the reviewer, so do your best to make it unique and
catchy.
Some prefer to start with a storytelling pattern.
• Second paragraph: Focus on the reason why you chose radiology.
• Third paragraph: Focus on your strengths and personality attributes
you will bring to the program and radiology, why a program should
choose you, and why you are specifically interested in that program
if you are creating a customized statement for your top choice
program.
• Final paragraph: Plans and aspirations after completing residency
training.
• Highly recommended to use the Association of University Radiologists
(AUR) Standardized Letter of Recommendation
(https://www.aur.org/resources/standardized-letter-recommendation) when
submitting letters of recommendations to diagnostic or interventional
radiology residency programs.
• Plan to get 4 letters of reference.
LETTERS OF REFERENCE

37
° You can submit up to 4 letters/program.
Plan on 4 so if one writer doesn’t get it done, you have a backup
letter.
° You can submit different letters to different programs but be careful.
• Submit 3 letters, the 4th is optional:
° 2 from core clerkships – these are generally more important than
radiology letters, as students play a more active role in the non-
radiology core clerkships than in a radiology rotation.
° 1 from clinical radiology clerkships – this could be from a radiology
faculty that you worked with during the general radiology clerkship or
a subspecialty radiology clerkship.
° The fourth is optional, however recommended. It could be from an
additional radiology faculty or research faculty. Because of the
intimate nature of the radiology community, the interviewers may
see a letter from someone they know and respect, which will
especially mean a lot. Research faculty may be important if applying
to research heavy academic programs.
° Ensure the letter writers know the specialty for which their letter is
meant. For example, letters for preliminary and categorical programs
can sometimes be confused and will be brought up during the
interview.
• Get the letters from someone who knows you well enough to talk about
your personal and professional strengths.
° It’s best if they offer an unsolicited letter, but you can scout out if they
think well of you. For example, if they write glowing comments on
evaluations such as “I wish the candidate were going into my
specialty,” it’s likely they’ll write you a strong letter.
° It is not important to get a letter from a “big name,” but if a “big
name” knows you well enough to write a genuine and personal
letter, it does not hurt. Usually, the department chair will not know
you well enough to write a personal letter and that will show in the
superficiality of the letter.
° If your first-choice program is of highest priority for geographic or
other reasons, you could request your letter writer to have
specifically addressed letters be sent to the programs which can
carry more weight.
38
For letters that are based on your clinical rotation performance, you may want to ask
your clinical preceptor for a letter of recommendation while your performance is still
fresh in the minds of the letter writer – it will make for a more personal letter, hopefully
with relevant anecdotes. Provide your letter-writer with your current CV and transcript.
For faculty that have known you for a significant period of time (e.g., radiology advisor,
research mentor, etc.), you should reconnect with them by mid-June to update them
(rotational experiences, research activity, evolving interests, etc.) and ask for a letter of
recommendation. Provide your letter-writer with your current CV and transcript.
Don’t ask for letters at the last minute – you may want to give the letter writer lots of time.
These are ideally ready to submit at the same time as your ERAS application around the
first week of September of year 4. Also, asking at the last minute suggests to the letter
writer you may procrastinate or that you are disorganized. Ask the Radiology advisor if
the Standard Letter of Recommendation (SLOR) should be forwarded to each LOR writer
(This also is relatively new and not yet mandatory).
How to go about asking for a letter of recommendation:
• Approach first by email asking whether the individual can write a strong letter
of recommendation. If the individual agrees, offer to meet to discuss your
career interests, rotational experiences, research activity, and other interests
outside medicine. Provide your CV, transcript, personal statement, any
evaluations you may think are helpful, and the ERAS Letter of
Recommendation Request.
• Leave them wiggle-room to refuse and look for cues when you meet with them
that make you sense they are not interested in/ able to write a strong letter of
recommendation.
By end of mid-July:
• You should have asked faculty for letters by now and be sure to check if
they are able to do it by the first week of September.
• Now it is obligatory to upload letters of recommendation through the Letter of
Recommendation Portal (LoRP)
° All letters of recommendation must be uploaded by the author
or the author’s designee using the LoRP. Medical schools will
no longer be able to upload letters on an applicant’s behalf.
TIMELINE FOR LETTERS OF RECOMMENDATION
39
By Labor Day:
• Remind faculty gently if the letters are not submitted.
° “I am so honored that you are writing a letter of reference. Just a
reminder, my advisor insists my package be complete by the first
week of September. Please feel free to contact me if you have
any questions or need more information to assist you in
completing my letter.”
° NOTE: You can and should submit your application by the first
week of September, but your letters do not have to be in by that
date. You will indicate on your applications from whom they
should expect letters.
• Ask your student affairs office to double-check for mistakes on the
letters, including your name/sex and that the correct residency
program is stated – that is, radiology, not e.g., orthopedic surgery.
Social media platforms have emerged as digital residency recruitment hubs, serving as
virtual environments for programs and applicants to share and learn information as well
as connect with each other before, during, and after recruitment season. Although many
residency programs use more than one social media application, Twitter has emerged
as a primary platform for both programs and applicants.
• It is most prudent to stay cyber squeaky clean and to remove any
compromising photos. Avoid any content relating to alcohol, drugs, sex,
politics, or dubious judgement.
• Social media, such as Twitter, can be used strategically to highlight your
accomplishments and to communicate your personal brand.
• There is a vibrant radiology community on Twitter for which applicants can
get information of virtual open houses offered by residency programs,
connect with program directors, as well learn of potential leadership and
mentorship opportunities.
• Below is a menu of Twitter handles that may be useful. These Twitter sites
are not validated or endorsed by AMSER or AUR and are the opinion of
others. The goal is to offer potentially helpful resources, with an
understanding that the information and application process is ever
changing.
° The American College of Radiology (ACR) Resident, Fellow, and
Student (RFS) Section: @ACRRFS
° AMSER: @AMSERRads
SOCIAL NETWORKING SITES

40
° American Association for Women in Radiology (AAWR): @AAWR_org
° Future Radiology Residents: @futureradres
° Radiology Student Interest Group: @RadiologySIG
• Most radiology residencies will also have an active Instagram account that
you should consider following, especially if you are interviewing at that
program. They may post announcements for events during the interview
season and their posts can also provide you with insight into interactions
between residents and the personality of a program, especially in the
setting of virtual interviews. However, keep in mind that this is their own
curated page. This page may also provide you with information about their
wellness activities, which can be mentioned during your interview day to
show that you have done your homework and how you may fit into a
program (“I really enjoyed seeing that you held a pet event at the park last
year, that’s something that I would be interested to participate in with my
dog.”) Direct messaging programs is possible, though not necessarily
recommended on this platform. As always, all interactions must be
professional and respectful.
Be careful with forums such as Aunt Minnie, Student Doctor Network, and Reddit.
There is a lot of bias and misinformation on these sites. Some anonymous applicants might
talk down a program to get others to rank it lower, hoping for a better chance to match. Also,
people from the programs may skim these sites, so something you write on them may come
back to haunt you. That said, some advantages to looking at these forums include finding out
when residencies are releasing interview invitations, when other applicants cancel interviews,
and if there are other applicants trying to swap interview dates.
If you have questions about the application process, it is recommended that you not rely
exclusively or even primarily on online forums to guide your decision-making. Direct
communications with your advisors, local faculty, and programs are the gold standard for
information gathering.
ONLINE FORUMS

41
HOW DO I APPLY?
• The Electronic Residency Application system (ERAS) is the central
application for residency.
• You create one application online and submit it to as many programs as
you want.
• The more programs you apply to, the more expensive it is. Think of this as
an investment.
• Complete your application by the first week of September opening date to
maximize your chances.
• Programs start reviewing applications as soon as they arrive so
you have the best chance of an interview if you apply early.
• The National Resident Matching Program (NRMP) is a private, not-
for-profit corporation established in 1952 to provide a uniform date of
appointment to positions in graduate medical education (GME) in the
United States.
• Applicants need to register both with ERAS and NRMP.
WHEN DO I HEAR FROM PROGRAMS?
• The majority of interviews are offered after the programs receive the
Medical Student Performance Evaluation, which is released to them by
ERAS on October 1.
• You will start hearing from programs via email in October or even
earlier, with the majority responding between mid-October and
January. (see “TIMELINE” Fourth year of Medical School section).
Check email OFTEN!
THE MyERAS
Ⓡ
APPLICATION
• There are new changes to the MyERAS
®
application for the 2023-2024
application cycle. These changes include updates to the experiences
section, geographic preferences, program signaling, and a new
impactful experiences section.
• The MyERAS
Ⓡ
application is to help students share more information
about themselves and their medical education journey. It also helps
programs better identify applicants who are genuinely interested in
ELECTRONIC RESIDENCY APPLICATION SYSTEM (ERAS) NATIONAL RESIDENT
MATCHING PROGRAM (NRMP)

42
their program and whose interests and experiences align well with the
program’s setting, mission, and goals.
• Components of the MyERAS
Ⓡ
application:
° Experiences section
♦ Identify a maximum of 10 experiences (previously
unlimited) and up to 3 meaningful experiences from the
following categories:
- Work
- Research
- Volunteer [Do not add any volunteer or
extracurricular activity that is not real as you
might be asked about during the interview and
can act against you if found fake]
- Education/Training
- Military Service
- Professional Organization
- Teaching/Mentoring
- Hobbies
♦ Designate a Primary Focus Area to each experience
♦ Identify a Key Characteristic associated with each
experience
♦ Describe the context, roles, and responsibilities (up to
1,020 characters)
♦ Identify up to 3 especially meaningful experiences and
why (up to 300 characters)
° Impactful experiences
♦ The impactful experiences prompt is identical from the
2022-2023 ERAS
Ⓡ
Supplemental Application, but now
has its own section in the MyERAS
Ⓡ
application.
° Geographic preference
♦ Applicants have an opportunity to communicate
regional preference(s), now using standardized fields
across the application.
- Select up to 3 of the 9 U.S. Census divisions
and share information and short explanation
(up to 300 characters)

43
- Section “No region preference” and short
explanation (up to 300 characters)
- Select “Do not wish to communicate a
preference”
♦ Applicants have an opportunity to communicate urban
and rural setting preference(s) separately and share a
short explanation.
° Program signals specific for Radiology
♦ Signals to diagnostic radiology (DR) and Interventional
radiology (IR)/DR will be combined.
♦ Applicants will be given up to 12 signals total.
- 6 gold
- 6 silver
♦ Gold signals designate your “most preferred” programs
♦. Silver signals designate your “preferred” programs
♦ Signals are appropriate to use in the interview offer
phase only
♦ Signals are only seen by programs you signal
♦ It is recommended to use the maximum allotted signals
per specialty
♦ Applicants should signal programs they are most
interested in – This includes home and away rotation
programs
♦ Based on prior year data, sending signals results in a
higher probability of interview invitation, however, sending
a signal does not guarantee an interview invitation

44
♦ Not every program participates and programs use signals
in different ways
- Programs may use signals as a screening tool
- Some may use as a tiebraker to help decide
who to interview
♦ Cannot send signals for individual tracks
♦ Code of conduct
- Programs shall NOT ask interviewees where
they have signaled
- Programs shall NOT disclose the number of
signals they have received
♦ Be prepared to answer why you signaled a program in an
interview
HOW MANY PROGRAMS?
Obviously, this depends on the student but there are trends and suggestions to
consider.
• In the 2021-2022 DR interview season, U.S. medical graduate applied to
an average of 66 programs and international medical graduates applied to
an average of 64 programs.
• In the 2021-2022 IR/DR interview season, U.S. medical graduates applied
to an average of 39 IR/DR programs and international medical graduates
applied to an average of average of 25 IR/DR programs
• It is a numbers game, and you want to maximize your chances of
matching.
• The Interventional Radiology (IR) residency program is EXTREMELY
competitive, more than Plastic Surgery and Orthopedic Surgery when you
consider the number of applicants to number of spots. If you absolutely
want to do Interventional Radiology, you might need to apply to almost
every program. Interview at all the programs offered and rank all the
programs you interviewed with.
• Most students applying to IR residency will apply to BOTH IR and DR
programs, because positions for IR residency are limited which
means it is EXTREMELY competitive. There is a good chance for not
matching IR residency but at least those applicants will match into
DR residency and still have the opportunity to do IR through ESIR or
Independent IR residency.
TO HOW MANY PROGRAMS AND WHERE SHOULD I APPLY?

45
• If you are selected for IR residency interview at a program, you are often
also selected for DR residency interview at the same program. The reverse
is not true. Some programs interview for both residencies on the same day
and some programs require you to come back separately for IR residency
interviews.
• You know where you stand based on how competitive you are, and
what kind of program you are interested in matching at. If you are more
competitive, you may be able to apply to fewer programs. Unfortunately,
geography counts, so students from more competitive regions should
apply to more places. For some people it may be 15 programs (for DR)
while others may want to apply to 50.
• One should apply to as many programs as you think you need to be able
to get at least 10 to 12 interviews.
• IMGs generally need to apply to more programs compared to U.S.
graduates, but with a similar goal of landing at least 10-12 interviews.
• If you applied to “too many” programs, you could always decline the
interview offers.
• It can be expensive if in-person interviewing resumes but think of applying
for residency as part of the investment in your education.
• You do not want to be in the position of having to SOAP (Supplemental
Offer and Acceptance Program) into a position after not matching. The last
few years, the unfilled radiology spots were very competitive – and went to
unmatched very strong students who didn’t match into dermatology,
orthopedics, plastic surgery, etc. (See: “I DIDN’T MATCH WHAT SHOULD
I DO?”). In 2023, there were no DR and no IR positions in the SOAP.
WHERE TO APPLY?
Generally:
• Academic programs at large universities are more competitive than
smaller community programs.
• Larger programs may have more didactic teaching, but you may get less
responsibility and “hands on” experience due to larger numbers of fellows.
• Larger programs may offer more research opportunities. Medium-sized
programs may have more hands-on opportunities.
• Some community programs may have less didactic faculty teaching.
• That said, there are wonderful programs, world-class teachers and
mentors, and gratifyingly affordable lifestyles waiting in unexpected
places.
46
Also remember that even with only minimal resources, you can teach
yourself anything.
• It is best to know what you are looking for in a program (size,
personality, activities outside of the hospital) and have honest
conversations with current residents about how different areas may
be able to offer that to you. Remember that you are going to be
spending at least 4 years at the program that you match into– you
want to make sure that you will be happy by finding the best fit for
you!
• Before applying to the list of programs, it is a good idea to make a
spreadsheet of the programs with their highlights like geographic location,
score requirement, research opportunities, and other perks. Most of the
general information is available on the FREIDA website including the visa
status required/ sponsored by the programs which is important information
for IMGs. This worksheet can be updated after the interview process and
might help you during the ranking process by reminding you about what
you liked about the program since it might be a couple of months between
the interview and ranking process.
Apply broadly to a combination of programs with the goal of obtaining at
least 10 to 12 interviews for DR and as many possible for IR.
• Apply to a range of programs (reach, middle tier target, less competitive)
and spread your net wide geographically and apply off the beaten trail.
• It’s best to apply to a broad range of programs in a limited number of
geographic locations that you like.
• If you have a special connection to a region or city, consider mentioning it
in your personal statement to programs in that region. You can upload
multiple versions of your personal statement in ERAS but only submit one
per program.
• Some regions are very competitive (see below). Location is a strong driving
factor in the competitiveness of a program, sometimes more than the quality
of the program itself.
How do I know if a program is university, university-affiliated or
community?
Search for individual programs here: FREIDA Online
There are “unofficial” rankings of diagnostic radiology residency
programs:
Doximity Residency Program Ranking

47
Aunt Minnie Minnies 2022 – Best Radiologist Training Program
For additional information, please review How to choose residency programs that
best fit
• Couples matching makes the process much more difficult.
• You both must apply to more programs than you would as an individual.
Again, it is a numbers game.
• Shoot for regions where there is a lot of overlap and where there are a lot
of programs.
• If one of you gets an interview at an institution or area and the other does
not, communicate with those programs to let them know about your
situation.
• Both people are regular NRMP matches: Make paired rank lists.
• If one person is an early match (ophthalmology, urology, etc.):
° The good news is the early match results come out before
the regular match rank deadline.
° The key is once again communication with the programs in
the area. Let them know the situation instantly – i.e., that you
are ranking them number 1 (if you are) or that you will be
ranking the programs in the area highly.
• For additional information, please review Navigating the Match as a
Couple
Communicate! But not too much! Be careful - do not annoy the program coordinator or
director. Times you might consider contacting the program director and/or the coordinator:
1. After you apply, but before you get an interview to show your interest.
You can do this as early as late October or early November if others
have gotten interviews at the program – especially if you think you are
competitive for the program, and if you are really interested in the
particular program, and it isn’t obvious.
2. If you have not heard about an interview and it is late in the interview
season, or you got a rejection.
3. If you have updates to your CV.
COUPLES MATCH
WHEN CAN YOU CONTACT A PROGRAM DIRECTLY?

48
4. After you interview - your “thank you note” or ”I really loved your
program” letter (see “SHOULD I SEND THANK YOU NOTES
AFTER INTERVIEWING?” section)
5. At the end of the interview season, before programs put in their final
rankings for applicants.
EMAIL ETIQUETTE IN BUSINESS COMMUNICATIONS:
• Headers are important - succinct summary of what the recipient will find
within.
e.g., “Update to Application for Radiology Residency/------ MSIV”
• Absence of a header/ subject line may lead to deletion by the viral-
cautious.
• Use professional format and phrasing.
• Do not address Program Director OR Program Coordinators by first name.
• Use an appropriate, identifiable email name.
• Make sure your contact information is there like email and telephone(s) -
have a signature block
WHEN YOU DON’T GET AN INTERVIEW:
Don’t take this personally. Programs receive hundreds of applications for a few
positions. Programs interview between 10 and 25 students per spot available.
• They are looking for reasons NOT to interview, and these may be
fairly superficial, especially towards the end of the application season.
CONTACTING PROGRAMS:
Correspondence with programs IS THE KEY to success!
• Programs want applicants who are interested in their program and did
not just apply there because it was another easy click on ERAS.
• Remember, they only choose 100 out of over 500 applications for
an interview so be proactive and show your interest.
• Programs want happy residents who don’t transfer after 1 or 2 years to the
place they really wanted to be.
Which programs to contact:
• Choose your top programs - e.g., your top 10.
• Programs you haven’t heard from.
• Programs that have sent you a rejection.
° Try these only if you are realistically competitive at and
obsessed with a particular program/locale - some initially

49
excluded students have gotten interviews and matched at
programs this way.
Who to contact:
• 99% of the time, contact the program coordinator, and cc the
program director, (their contact information is listed either on
the program website or on ERAS).
How to contact:
• Do not be annoying.
• Brief, professional, articulate email or phone call reiterating your interest.
• Email is better: You have more control - it is more difficult to mess up.
• Phone call - a pleasant call to a coordinator can be more personal, but…
• You may have to rehearse what you will say.
• If you call when he or she is busy, it could be annoying.
• Cell phone calls may be hard to hear. Consider landlines.
• The call may be forgotten/the program director may never get notice
of your inquiry.
• Information may not be correctly conveyed.
What to say:
• Tell the program you are interested in them, and you would love to
have the opportunity to interview with them.
• Tell them about why you are interested in their program.
° This is particularly important if you are applying to a markedly
different geographical area, i.e., Grew up there? Spouse job
opportunities? Couples matching? Have children and need to
stay in a specific area? Or specific details about their program
and why you like it.
° “I would love to do residency in an area I have never lived before”
is absolutely appropriate, but it doesn’t carry as much weight as “I
have family in the area.”
° Program directors know that most applicants match in areas where
they have a family connection or in the region they attend medical
school.
• You could send selected data, but keep it VERY BRIEF, just enough to
catch their interest. e.g., your medical school, grades, board scores,
AOA/awards, publications, updates, etc.
• It is prudent to include the AAMC or NRMP ID in the email communication

50
so it is easy to add note to your application in case the program wants to
refer to your application following your email.
NOTE: Don’t be offended if the program directors do not reply - they get hundreds of
emails from students.
A common e-mail could read:
The majority of diagnostic radiology residents choose to do a preliminary medicine
year or transitional year for internship, with surgery as a strong second choice. For IR,
surgery is suggested. However, almost all specialties including pediatrics, emergency
medicine, and obstetrics/gynecology can be considered a preliminary year.
Transitional years:
There are few programs, so these are the most competitive.
• In general, offers more flexible schedule and electives than
preliminary medicine or surgery. Work hours are usually less than
the other two options.
• Most are located at community hospitals.
• Variable - look up the details for each program.
Dear Dr. ...
I'm a fourth-year student at _________________ Medical School. I'd like to reiterate
my interest in your program and I hope that you’ll consider me for an interview. (If
you’ve been rejected, write “I’d like to reiterate my interest in your program and ask
if you’d reconsider my application for an interview.”) I am particularly interested in
your program because (…my family lives in the area/I have heard outstanding
reports of your program from a radiologist at my institution/I love the outdoors and
wish to move to a rural area…etc.)
After that---you could include a short paragraph with a few facts – grades, updates,
etc. – 2-3 sentences at most.
Thank you for your time.
Your Name
_________Medical School
Class of 20XX
Good professional address
Reliable phone number
INTERN YEAR
51
• VERY COMPETITIVE because Dermatology, Ophthalmology,
Radiation Oncology, and Anesthesiology applicants also apply for these.
• If you are applying to transitional year, you should also apply to
preliminary medicine programs for backup. These interviews are
hard to get and matching is also difficult.
Preliminary medicine:
Most residents do medicine.
• Some are flexible and offer various elective options.
• Your schedule will be like an internal medicine PGY-1 resident with usually
2 ICU, 2 electives which can be radiology, and other IM rotations.
Preliminary surgery:
These are less competitive, but often required for IR residency, sometimes at the same
institution.
• It may be an advantage for radiology – as you learn anatomy and
procedures.
• Try a less busy program that has less “scut” and more hands-on work to
learn the “what & how.”
• Since these may be less competitive, if location is paramount to you,
this gives you the best chance of getting your top location.
Why do I have to go on twice as many interviews?
• As a radiology applicant you must apply, interview, and rank separately
for the intern year (PGY 1) and your advanced (PGY 2-5) radiology
years unless you match into a categorical (PGY 1-5) radiology program
(small minority of programs).
• If interested in IR training, you will likely have to interview for both DR
and IR residency. Programs that offer both will often interview you for
both on the same day – for instance, morning for the DR program,
afternoon for the IR program.
• It is easier to match into preliminary medicine and surgery than into
radiology so applying to 8-10 should suffice unless you pick very
competitive locations (Boston, Manhattan, California, and Seattle).
Consider applying to local programs affiliated with or familiar with your
medical school to increase your chances of matching. However, if you
want to have options for a prelim year then take that application
seriously as well.

52
• Though the intern year is easier than the advanced radiology
residency matching, there have been situations where the students
have matched into radiology but not for the intern year. In such
situations, students try to scramble through the SOAP process. If still
unsuccessful, they usually have time until the end of June to try to
match into any unfilled program in the country. If still not matched into
the intern year, they will have to forfeit their radiology matched
program as they cannot proceed without an intern year. Hence, taking
the intern year application process seriously is advisable.
• Don’t count on unfilled positions to scramble into as they are
becoming less common. (See: “MATCH WEEK!” section)
• The majority of programs you interview at for radiology are for
advanced positions and do not include the intern year.
• Some programs do include the intern year, which you do not need to
interview for separately.
• Some radiology programs offer an intern year at the same institution
(with same day interview) but you have to rank and match them
separately.
• Other programs let you rank them for both their advanced positions
and for their categorical positions (this will be 2 separate entries on
your rank list).
As you’re applying, you have to decide what is important for you regarding
intern year.
• Do you want to be in a specific location, such as in the same area as your
radiology residency, which will likely reduce the number of times that you
will have to move?
• Do you want a less intense year with minimal floor months?
• Do you want to get intense training?
• Do you want to be in Hawaii for a year?
• Due to the COVID-19 pandemic and statements issued from the
Association of American Medical Colleges (AAMC) and Coalition for
Physician Accountability, most residency and fellowship programs
SO YOU GOT THE INTERVIEW, NOW WHAT?
SCHEDULING INTERVIEWS
53
adopted online interactive virtual interviews in the 2020-2021 and
continued in the 2021-2022 and 2022-2023 interview cycles.
• In 2023 the AAMC again issued a statement recommending programs
continue to use a virtual interview format moving forward. The
recommendation was based on the following ideas:
° Virtual interviewing improves equity by eliminating cost of
application (travel, etc.)
° Opens opportunities for applicants that may have otherwise
declined an interview due to financial constraints
♦ Relative ease of scheduling virtual interviews
♦ Reducing time away from clinical rotations
° Reducing applicant stress and anxiety
° Increased number of faculty willing to participate in the
interviewing process due to reduced time commitment
° IMPROVED SCHEDULING FLEXIBILITY
° Virtual interviewing is more environmentally responsible.
Candidates are generally offered a select few days to interview on a first response first
serve basis.
• Respond to interview offers ASAP. Do not put off signing up for an
interview while you are waiting to hear from another program. Interview
spots often fill up within hours of being sent out. Consider setting up an
ERAS-only email account with push notifications (so that you know
those notifications are related to residency applications) and/or linking
this email account to a pager so that you can reply as quickly as
possible.
• Do a preliminary year interview first, or a school destined to be low on
your list. If possible, do the ones you care about in December or
January – you have more practice, and they remember you more for
when they rank their list.
• Canceling interviews is ok, and common towards the end of the
interview season. But you MUST contact the program.
° Not turning up is VERY BAD and will get both communicated
and remembered later…
° Program and student directors get together annually and
have long memories.
CANCELLING INTERVIEWS

54
• Try to avoid last minute cancellations. You may be preventing another
student from an interview.
° But even if it is last minute, it is courteous and respectful
to let the program know you are not coming, and it is
possible that the spot still can be offered to someone else.
Last minute cancellations due to personal reasons (sick family
members, etc.) are ok– program directors and coordinators understand
that applicants have personal lives and that there is more going on than
just applications! Again, always communicate with the program and if
you are still interested in interviewing at that program, let them know
and ask if it is possible to fit you in on another day.
It is a small world - not acting professionally gets around!
• Practice virtual interviewing.
• If there are workshops at school, attend these.
• Arrange for a dress-rehearsal mock virtual interview with a faculty member
you don’t know.
• Find out exactly what time your interview day begins (keep in mind of the
time zone) and plan to log in at least 5 minutes early to give yourself time
to troubleshoot any connection issues.
• You can ask the program coordinator what to expect. You also can
typically check your interview day schedule in advance (can log into
Thalamus if they are using this platform; if Zoom is being used, a PDF with
your schedule will often be sent out beforehand).
• You may have anywhere between 2 and 9 interviews. Some programs do
“speed interviewing” (5 to 6 10-minute interviews).
• Look up information about the program and your interviewers on their
website.
° Lack of knowledge about the program and the use of only
generic questions are a turn off.
° Looking up information shows that you are interested,
resourceful, and unafraid of doing a little bit of work.
° Write down specific questions on your portfolio pad. During
the interview you can refer to the questions and show the
preparations you’ve made.
PREPARATION

55
° So, then, during the interview you can focus more on if you
like the place or not based on things that can’t be found on
the website.
• It is important to have at least 2-3 specific questions ready to ask the
interviewer in case your conversation ends before the allotted time. Do
your homework, look up the program, learn about the unique aspects of
the program, come up with questions related to the interviewing faculty
member’s subspeciality or work/publication etc. (you will receive a list of
interviewing faculty names before the interview date) rather than asking
generic questions. This will also show your interest in the program. There
might be situations and times where you might run out of questions or
might have already been answered by the program members during the
introduction. In such cases and when you don't have any more questions,
but the interviewer asks if you have any questions, you can answer by
saying "My questions were already answered by the previous interviewers
in detail, and I thank you for giving me the time and opportunity to make
sure all my questions are answered".
• You can send new information/updates and/or bring it to the interview:
New research, AOA election, brilliant Step 2 scores (see “When you can
contact a program directly” section). If you have updates after the
interview, send them also.
• Know everything on your application including exactly what each research
project was. Also be able to speak knowledgeably about the hobbies that
you’ve listed! You should be able to carry on a conversation about your
research and your hobbies that goes deeper than just surface level with
any interviewer that may know something about these areas.
• Dress neatly and conservatively (hopefully the same as in your picture).
They should think you know the unwritten rules.
Clothing doesn’t have to be all black: a little color is okay, such as an
interesting blouse or tie.
° Avoid trendy fashions.
° Not too short a skirt—you don’t want to be tugging at it.
° Clean hands and fingernails (consider removing all nail
polish or making conservative choice).
° Limit external ornamentation.

56
SETUP:
• You will need a quiet area with a fast and reliable internet connection to do
your virtual interviews to avoid lag in the conversation during the interview.
If your living space is noisy and not suitable for residency interviews, some
people have done their interviews at their medical school in a personal
study room. If you plan to do this, be sure that the space you intend to use
is going to be available.
• Test your computer in advance to make sure that both the camera and the
microphone are functional. If they are not, it is likely worthwhile to invest in
a new computer at this time to use for both interview season, residency,
and beyond. Virtual communications are here to stay.
• Make sure your computer is fully charged or, even better, connected to a
power source. You do not want to lose connection in the middle of the
interview.
• Set up your computer ideally around your eye level, about 2 feet from you
with your face centered within the field of view. Ensure good lighting–
some people have found that investing in a ring light (easily obtainable on
Amazon) is helpful, but this may not be necessary for your particular
interview space. Different camera angles (especially an extreme angle
from below combined with poor lighting) can sometimes be very
distracting for interviewers and will detract from the content of your
interview.
• If you have notes written on your desktop or a second monitor screen,
avoid looking at them/ scrolling while doing the interview as it might look
like you are not paying attention to the interviewer. It is advisable to have
notes on a paper pad during the interview and ideally make notes after the
session is over.
• Ensure your background is professional appearing. This can mean a
variety of things, ranging anywhere from a blank wall to tasteful, simple
pictures or plants behind you or even using the background blur function
on the video chat platform. Regardless of what you choose, make sure it
is reproducible (as not all institutions will use the same platform) and not
too distracting.
• If you have pets, we would recommend putting them in another room
unless they are extremely well behaved and quiet. If your pet DOES end
up interrupting one of your interviews, it’s probably best to acknowledge
this and explain to your interviewer VERY briefly (i.e., “Sorry, my cat got
out and is rubbing its head against my leg.”). Otherwise, your looking
VIRTUAL INTERVIEW SETUP AND ENVIRONMENT

57
down at your pet may be interpreted by your interviewer as disinterest in
the conversation or you being unable to carry the conversation and
referencing notes outside of the camera’s field of view.
• Log in to the virtual interview at least 5 minutes early to make sure there
are not any technical issues.
INTERVIEW DAY ETIQUETTE:
There will be a lot of overlap between in-person and virtual interviewing etiquette.
However, there are some unique areas, outlined below:
• Clothing: Wear what you normally would wear for an in-person interview,
including pants for men. Some applicants in the past felt that since only
their upper half was visible, pants were not necessary, but if you get up
while your camera is still on for some reason, which others have done,
you will not make a good impression. Depending on how egregious the
exposure was, you may end up not getting ranked by that program, and
again, programs talk to each other. Best to not take that risk and just wear
your entire outfit.
• Open chat rooms: Most programs will have a chat room open throughout
the interview day staffed by residents. You should always stop in with at
least one question, since even though these are listed as being optional,
programs take note of who is attending what events and may view a lack
of attendance at an optional event as disinterest on your part. That being
said, there is a balance and you should not overstay your welcome in that
room. If you have had your questions answered, there is nothing else that
you want to discuss, and the conversation feels like it’s wrapping up, thank
the resident for their time and leave the room. If you are still having a lively
conversation with the resident though, feel free to stay! This is a good time
to evaluate whether or not you think you would fit in with the personality of
the residents at the program. The moral of the story here is to clearly
demonstrate your interest in the program while also reading social cues to
interact appropriately with the resident(s) manning the chat room.
• Do your best to maintain eye contact. This is just as, if not even more,
important for virtual interviewing as compared to in-person interviewing,
since the interviewer cannot tell what you are breaking eye contact to look
at when virtual.
• Do not end your interview early. This goes for both in-person and virtual,
but it does not come off well if the interviewee abruptly ends an interview
before it is scheduled to end. However, you should be cognizant of the
time and your schedule so that you do not run over into the time allotted
for your following interview. If this happens, tell your interviewer “I’ve really

58
enjoyed our conversation, but unfortunately, I think that we’ve used up all
of our time and I’m scheduled for another interview in a couple of
minutes.” Thank them for their time.
• The interview season can be long and grueling, especially when
interviewing for preliminary and categorical positions separately. Despite
this, it is critical for you to maintain your energy throughout, as a lack of
engagement, even if due to interview fatigue, will inevitably be noticed.
Backup/ Troubleshooting:
• Have your phone on silent but easily available to you. Video chats are
reasonably reliable but will never be 100%. Sometimes it will be necessary
to convert your video interview to a phone interview, and sometimes you
will need to dial in to the video chat on your phone if the audio from the
video chat is not functional. That being said, DO NOT allow your phone to
become a source of distraction for you. We recommend keeping it face
down unless you need it.
• Make sure that you have the program coordinator’s phone number in
advance. If you are unable to connect to a video chat, try calling the phone
number provided through the video chat platform. If you are still not able to
reach anyone, call the program coordinator to see if he/she can connect
you with your interviewer.
• Ensure that the phone number that you provided on your ERAS
application is current and active– your interviewer may attempt to call your
listed cell number if the video chat is not working.
PRE-INTERVIEW MEET/GREETS:
The vast majority of programs will have these sessions before your interview day so that
you will have the opportunity to virtually interact with the residents without faculty being
present.
• Though these are technically optional, you should do your best to attend
the events for all the programs that you are interested in. Programs will
take note of who has and has not attended these events and may interpret
a lack of attendance as a lack of interest. If you are unable to attend the
event on the date that you are assigned, email the program coordinator to
find out if there is another session that you can attend.
• Be personable with and have questions for the residents. Though this is
not an official part of the interview day, programs will still ask their
residents for input on applicants that they have encountered during these
sessions. Applicants have both risen and fallen on the rank list based on
these events.

59
• Maintain friendly interactions with all your fellow applicants. Not only will
it look bad in the short term if you are confrontational with another
applicant, but that person may end up being a co-resident in the not-to-
distant future and will also most likely be a future colleague in some
capacity. Radiology is a small world, and you never want to burn bridges.
• Make sure you interact with the residents of the program and be
friendly with your co-applicants. This will reflect your congeniality. Be
respectful of the time and let others have time and opportunity to talk as
well. Sometimes, a few candidates take up most of the allotted time
leaving minimal to no time for other candidates who are not outspoken/
introverts. Try to be a team player/ good sport.
• There are a variety of platforms that may be used for these sessions. Do
your best to be familiar with them so that you can focus on the interaction
rather than navigating a chat room.
• This is one of your opportunities to interact with current residents and to
see if you will fit in with the “personality” and “culture” of the program and
its trainees. Make the most of it.
• You may or may not receive a gift card to be used for a meal during this
session from the program.
AT THE INTERVIEW:
Most find radiology interviews to be very friendly and mostly a get-to-know-you
session. If you've made it to the interview the program is very interested in you
and just wants to see what kind of a person you are.
Particularly in radiology, where you spend a lot of time sitting next to people in the
reading room and interacting with clinicians and radiology personnel, they want to
make sure you are the sort of person who is friendly, fun, honest, responsible and
hard-working.
The easier the interaction during the interview, the better the outcome.
• From when you pull onto campus to the time you leave, you must be in
interview mode.
° Even during lunch or just sitting around waiting, be
appropriate and respectful.
° The non-medical staff can exercise astonishing veto
power. No one wants a resident who may be rude to
technologists, nurses, and secretaries in the future.
° Coordinators also have the power to help you, so treat them
well.

60
° YOU ARE NEVER “OFF THE RECORD.” Sorry, but it’s true.
• This is your time to shine - you are trying to sell yourself, but do not come
off as arrogant.
• Relax and enjoy yourself. Be yourself, act interested and be enthusiastic.
Interviewers will notice.
• Don’t fall asleep during the Chairman's presentation (yes, it’s happened!).
Get a feel for the program.
• Are the residents happy? Do you have an opportunity to meet the
residents?
• Some programs may try to “hide” their residents - this is a warning sign!
• Do you feel comfortable during the interview day and in the area where
hospital is located?
• Is it somewhere you would want to work and live?
QUESTIONS DURING INTERVIEWS:
Specific answers don't matter. Be prepared to be crisp, professional, and
eloquent without sounding as if you pre-memorized every word. Use every
opportunity you can to sell yourself to the program and to keep a conversation
going. Never just respond with a “yes” or “no” answer even if asked a “yes” or
“no” question.
SMILE☺!
Write notes right away to help you write thank you emails (if you do so) and especially
during ranking the programs. Otherwise, the details of the programs will run together.
Common questions for the candidate:
• You must know and be able to answer questions about everything
on your application. You will be amazed by what some interviewers
pull out of your application and by what some don’t seem to notice.
° Most of the questions you will get are phrased like this:
“I see on your application…” or “Tell me more about …”
• Why did you apply here (second most common)?
• Tell me about yourself - have a nice 4 to 5 sentence synopsis about YOU.
Don’t say, “What do you mean?” Decide ahead of time if you’re going to
talk about your life story, about academics, etc. Make it short and sweet –
and interesting if possible.
• What particularly interests you about our program?
• What can I tell you about our program?
61
• What are you looking for in a program?
• Why radiology?
• If you couldn’t do radiology, what would you do? Why didn’t you do (your
answer) anyway?
• What seminal papers has your letter writer written?
• What was your worst hospital experience?
• Tell me about a patient encounter… (be prepared to talk about a
specific patient you interacted with and something you learned about
this interaction; it does not have to be about a radiology patient. This
question has been especially common in preliminary program
interviews).
• Favorite organ system? Discuss imaging of that system.
• What do you think about the healthcare system?
• What are the challenges ahead for radiology?
• Read the papers during interview season – be aware of what’s going on.
• Where do you see yourself in 10 years?
• Tell me about your research.
• I notice you play…insert name of sport, instrument.
• What do you like to do for fun? You can say something that is not on your
application. e.g., “I like to go fishing” but don’t stop there.
• What was your biggest mistake?
• Describe a challenge you have surmounted.
• What was your one defining moment? What are you most proud of?
• Have you ever lost your temper in a clinical setting?
• What does it take to get you angry? Ever been in a fistfight?
• What are your strengths and weaknesses? Cliché, but you will
definitely get this question. Prepare an example of each, and
for your weakness, discuss how you are trying to improve it.
• What sets you apart from the other applicants?
• Tell me three things your best friend would say he/she liked about you.
And didn’t like.
• Tell me about a decision you've made in the last year.
• Tell me about a bad decision you’ve made.
• Tell me a joke (!!). Be careful.
• What was the last museum (theatre, movie, public park) you saw?
• What was the last/favorite book you read/movie you’ve seen? Be familiar
with the claimed book.
• If you were an animal, which would you be?

62
• If you were a plant, what kind would you be?
• Or to show you a paper, coin, or toothpick mind-teaser (“Using only
these 3 pennies, build a model of the Spaceship Enterprise…”) or ask
you to solve an odd puzzle question. And occasionally an interviewer
just sits there, silent, to see your reaction…try not to babble.
• What do you think about healthcare reform? (Avoid political answers
or taking sides).
• Where are we on your rank list?” (ILLEGAL!!! Be tactful and
evasive e.g., “I am still putting a lot of thought into my list and I
haven’t finished interviewing yet”)
• And of course, that great conversation-stopper: "Do you have any
questions for me?" Make sure you do! See below.
Questions for the attending interviewer
It is crucial that you know about the program and have specific questions to
ask. Research the program before you go and write a list of questions that
you can ask. Don’t let interviewers feel that you are just going through the
motions or using them as a “safety” program. Don’t be afraid to ask more than
one person the same questions. Don’t ask questions that were answered at
general sessions unless you want clarification; it makes you look like you
were not paying attention. Write questions down, it’s ok to look at your notes.
• Has your new Chairman changed the department significantly? Are more
changes to come?
• You have an animal MRI research lab. Can residents become involved in
projects?
• What kind of equipment do you have? (but do the research first
about what is available and what it means - and what they have on
the website already)
• Research opportunities? Is there protected time for research?
• How much didactic/case conference lectures are there? Is this time
protected for the residents?
• Teaching responsibilities for the residents?
• How do you prepare your residents for the CORE exam?
• Do residents attend any review courses for the CORE exam?
There is simply no way to anticipate or prepare for some things. Should
you freeze and flail, practice saying “I am sorry, I’ve never thought about
that question. Let me think and then start talking again.” And smile a lot.

63
• I see that you have 6 IR residents and fellows, how does this affect
resident opportunities for hands-on training?
• What kind of attending backup is there on call?
• Any changes to the program in the future?
• Patient population? Not if this is obvious from the website or situation – VA
hospital, County hospital.
• Do residents rotate at other hospitals?
• I have 2 school age children, what are the schools like in the area?
• Real estate is very expensive locally, so where do the residents live?
• What makes a good radiology resident?
• What is a typical day for a radiology resident in your program?
• Where have the residents ended up for fellowship and what specialty? (if
this information is not available on the program website)
• Moonlighting opportunities within the program?
• Is there research opportunities or support for research work in the
program?
• Is mentoring available for residents interested in leadership roles?
• Educational funds for residents presenting at national or international
conferences?
• Any outside rotations for residents? (e.g., pediatric radiology,
AIRP, etc.)
• Core exam passing rate for the program?
Questions for the residents (interviewers and others)
You may have resident interviews, and in between interviews you will have the
chance to ask the residents about the program. Many programs hold dinners or
lunches with the residents. They are your best source of information. Talk to
younger residents as well because they are closest to where you will be and some
of them will even be there when you start. Try to get a feel for the level of morale
and general resident satisfaction with the program.
• What is call like? Night float or overnight call? How is the backup during
call?
• What is the patient load like?
• Who gives the lectures? How do you like the didactics and teaching?
Ability to attend conferences?
• What is the interaction like between the residents and attendings?
How do you read out with the attendings?
• How prepared were you for the CORE exam?
• How much time did you get to study for the CORE exam?

64
• Faculty/resident ratio. Is there a lot of staff/resident turnover? Staff
support?
• Do they get good hands-on experience?
• Wide variety of cases?
• Boards pass rates?
• Opportunities for fellowship? But you can go to another, more academic
program for fellowship.
• What do you like about working here?
• What do you dislike?
• Benefits like meals, health insurance, vacation, pay, etc.?
• What are the social/family opportunities outside work?
• Housing costs? Where do residents live? Cost of living? What is the
parking situation?
• Spouse work opportunities?
• Is moonlighting available (be careful, sometimes this is a “don’t ask, don’t
tell” issue)?
For additional information, Interviewing residency programs
The following are direct quotes from interviewers:
Dislikes
• Having no questions to ask me.
• Asking me what are the strengths and weaknesses of my
program. Who is interviewing who? Too general and standard a
question.
• Having no knowledge of the program.
• I'm not a big fan of saying that the program looked good on the
website as a reason for coming here. Makes it seem like you liked
their pretty website-only! Specific reasons for choosing programs
(size, location, heard about from somebody that works here) is
advantageous.
• Inability to back up something they put on the application (e.g.,
concert level pianist who has only played at school concerts).
• When a medical student has already chosen their fellowship before
they have done radiology.
INTERVIEWERS LIKES AND DISLIKES

65
• Don’t overuse casual phrases – dude, man, like, awesome, totally.
• Don’t make a statement sound like a question: “I’m from California?”
• One-word, dead end answers to questions.
• Hedging.
• Nervous fiddling, playing with face or hair. Jiggling knees.
• Chewing gum.
• Very short skirts.
• Do the interview, and don’t come back to talk to me again, unless
there is a reason. I’m busy.
• Staring in a different direction than facing the camera.
• When the interviewer can see flashing lights in the candidates' eyeglasses
which is probably from the candidate browsing some website or watching
something else during the interview.
• Asking the interviewer what subspeciality they are in which indicates they
have not done their basic homework for the interview.
• Low volume without mic where the interviewer needs to ask them
repeatedly to speak again or louder.
• Candidate ending the conversation early and leaving the assigned room
before the allotted time.
• Making fun of the program's residents whom they met at the meet and
greet or pre interview dinner.
• If you follow up with me in some way, try to do it in a way that does not
require me to respond. I don’t want 50 new pen pals.
Likes
• Questions that show the student has prepared: looked at the
website, talked to someone, thought about it e.g.,
° Location/geography – “how does it affect case mix and
potential experience?”
° “The------ program looks interesting,” and then asking
specific questions about it, not just “Tell me about it,” while I
sit here and try to stay awake.
• Know something about the program, a few specific strengths even if
from the program's web site, can show that you did your homework
and are motivated to be a resident there.
• Just tell me about the issue/problem in medical school, the gap,
the foreign school, the unusual employment history - I’ll find out
anyway. It’s better to own up and tell me what it taught you.
• Show enthusiasm both for radiology and for the program specifically, but
don't overdo it.

66
• I want to see that they are excited by the practice of radiology not the
lifestyle, money or even that their primary interest is the technology
itself. I want to sense that what really turns them on is trying to figure
out what is wrong or not wrong with the patient, i.e., making the
diagnosis.
• I like when I can have an interesting conversation with the applicant and
get to know them as a person. They already made the cut academically,
or they wouldn’t be interviewing.
• Have something interesting to talk about from your application.
• I love it when I learn something in the interview.
• I like good eye contact and students that are genuine and
straightforward, comfortable being themselves, not trying to
play some role in interview mode.
• Firm handshake.
CORE exam pass rates, review courses, and dedicated study time
Conferences
• Quality
• Number
• Topics
• Cancellations
Is there a department/facility library?
• Teaching files
• Books
Opportunity to do cases
• Do the fellows stand in the way?
• Procedure log numbers
• Pick a particular procedure: e.g., Nephrostomies - How many do
residents do?
What are the elective opportunities?
• Legal rotation
• Practice management
• Personal finance
THINGS TO CONSIDER AT THE PROGRAMS WHEN INTERVIEWING AND RANKING
67
•. International experiences (e.g., Rad-Aid)
What are the benefits provided?
• Salary & how does it compare to others?
• Medical, dental, and optical insurance?
• Retirement plan and matching?
• Academic or book fund?
• Vacation days?
• Statdx, Radprimer, or e-anatomy?
• Conference funding?
• AIRP funding?
• Moonlighting opportunities?
° Contrast coverage
° Clinical moonlighting
• Parking included?
• Public transportation discounts?
•. House officers’ union?
Ultrasound scanning opportunities
How are the core competencies incorporated into the program? Do the residents
evaluate the faculty?
Is research available? Required or encouraged
Is preliminary year included?
Fellowship Opportunities
Size of Program
• Number of residents
• Number of fellows
• Number of staff
• Is it small, medium, or large?
Geographic considerations
Is there diversity in the program?
• Ethnic
68
• Gender
Camaraderie
• Between residents
• Between residents & staff
• Between residents & ancillary personnel
Relationship with colleague
Stability of the staff
• Are the numbers going up or down?
• Where has the staff trained?
• Is there a section of the department that is particularly strong or weak?
Is the Program Director approachable? And the residency coordinator?
• Is he or she a resident advocate?
PACS and IT
Volume and types of cases at the hospitals
• Admissions
• Surgeries
• ED visits – Trauma Center?
Facility
• Radiology equipment
• Physical plant
• Day care service
• Cafeteria
• Future expansion
Relationship of Radiology and the rest of the hospital
• Medicine
• Surgery
• Pediatrics
• OB
• ED

69
How does the hospital treat its employees?
Accreditation
• How many years?
Surrounding Area
• Childcare
• Schooling
• Shopping
• Housing availability
• Safety
• Social and cultural activities
• Sports
• No easy answer.
• It is not going to make a poor candidate a viable one, and if you are a
good candidate then it probably won’t make much difference to your
ranking.
• Send via email to the program coordinator and a few selected people in a
timely manner.
• Ask up front for PD preferences – some will ask you not to.
• Between the time of the interview and the Match, students should
exercise common sense and good taste, and bottom line: avoid
irritating or causing more work for the PD.
• Make notes right after finishing the interview day, to help when you write
these emails.
• Brief, professional, personal - one that states something specific
about the program or the interview day.
° Humor helps when in good taste.
° Grammar and spelling - all names should be correctly
spelled.
• Try to personalize the email, if possible, with specific conversations you
had with a particular interviewer. These reminders can come from any
notes taken during or in between interview sessions.
• Try to send the thank you emails the same day or at least within one week
following the interview when your face and interaction is still fresh in their
SHOULD I SEND THANK YOU NOTES AFTER INTERVIEWING?

70
minds.
• IF IT IS TRUE, espouse your enthusiasm and allude to your hopes and
send the I AM RANKING YOU NUMBER ONE EMAIL.
° It is to your advantage to tell your number one program that
you are ranking them number one. Do not send this email to
multiple programs. Radiology is a small world and it might
haunt you if you do this to multiple programs.
° It is the best card you can play and the only way for you to
TRY TO convince programs to rank you higher after the
interview. Send this email in January, right before the
ranking meeting. Make it short, concise, clear, and direct. Do
not hedge or beat around the bush.
° Telling a program that you are “ranking them highly,” “near
the top,” or in other similar language will let the program
director know that you are not ranking them number one.
Because if you were ranking them number one, you would
say so, since almost all medical students would say so to get
themselves ranked higher. It might be better to not say
anything than to tell them you are “ranking them highly.”
Program directors have been playing this game for many
years, much longer than you, and know how to read in
between the lines.
For discussion on communicating with programs, please see: Applicant to
Residency Program Translation Guide
• A computer with a mathematical algorithm determines your fate: How the
Matching Algorithm Works
• Submit early – you can change it - don’t wait until the final hours to certify it
the first time.
• The radiology faculty advisor is YOUR advocate, and you should feel free to
discuss your rank list with him or her. She/he will not divulge this to the
ranking committee unless at any point it seems to YOUR detriment not to.
• There is no “one size fits all” answer to this. Refer to your detailed notes, but
trust your gut: You must find the one thing that matters most to you in a
program. Is a significant other/family in the city? Research or IR experience?
Happy residents?
RANKING PROGRAMS

71
(See: “THINGS TO CONSIDER AT THE PROGRAMS WHEN
INTERVIEWING AND RANKING” section)
• Rank all programs that you interviewed at, unless you really hated a particular
place - but consider whether you would rather not do radiology than match
there. Be realistic. Don’t get emotionally committed to any program.
• Rank based on where YOU want to go. The applicant’s rank list has priority
over the programs’ rank lists!
The computer algorithm DOES favor the applicant. Do NOT rank places you
WOULD NOT go to.
° Take the 3 you like best and put them in order of where you
want to live.
° Rank the bottom 3.
° No advice about the middle ranks. They are often the most
difficult to rank.
° Don’t try and work in your interpretation of the likelihood of
matching, you are likely to be wrong and it doesn’t matter. List in
the order you want.
• If you are interested in IR training and applied to both DR and IR
residency (you generally should), then you will have to create a rank list
containing both types of programs.
• Most applicants in this situation would rank the IR programs above the
DR programs, however it is applicant and program specific. For
example, you may rank IR program A #1 and IR program B #2 but
prefer DR program A over IR program C at #3.
• Because IR residency is much more competitive than DR residency,
you are likely to receive more AND better interviews at DR programs
than IR programs. How you rank this is up to you.
• For Radiology, you must rank both your radiology PGY 2 year and your
PGY 1 intern year. You must enter the intern year as a “supplemental list.”
So, if you match at program X, then the computer goes into the
supplemental list you ranked for program X and it tries to place you as
high as it can on that list.
Correspond with your top programs once more before they rank. (See “WHEN
YOU CAN CONTACT A PROGRAM DIRECTLY?” section)
• Students feel that they will not be ranked well unless they tell the
program that they are ranking that program number 1, or at least in
the top 3. This isn’t true – you will be ranked on your merits, although
it helps to know if you are interested.

72
• At the end of the interview season, if you tell a program director that
you are ranking their program “highly,” then they know you are not
ranking them number 1. With experience they have learned that if a
student were ranking them number 1, then he or she would say so.
• So, it is only your “ranking you number 1” email that might have an impact
on how programs rank you.
• Programs rank at all different times, and if you contact them, it
should be before they rank. Find out their last interview day and
email them shortly after this date.
• Conversely, programs might try to change how you rank them by sending
you emails and saying you are ranked “highly.” The only meaningful email
from programs is a “ranked to match” email and this email might be
deceiving. For example, if a program has 10 spots and you are “ranked to
match,” then theoretically you are ranked in their top 10 and will match
there if you rank them number 1. However, people don’t always tell the
truth. Don’t be sure until you open your letter on Match Day.
• It is within Match Rules to tell a program “You are my first choice.”
"Having finished my interviews, I wanted to tell you how impressed I
was with your program. I am ranking you number 1 and would be
honored to join you in 2---. I hope you will keep me strongly in mind."
• Match violations: programs SHOULD NOT ask you how you are ranking
them (nor can you ask them).
• If a program calls and tells you that you are being ranked highly, you
need not answer directly. Have a handy answer ready – something
positive, appreciative, but noncommittal: "Thank you, I am flattered and
thrilled. You will be high on my list, but I haven’t finalized it yet."
• Along the same lines, don’t believe what they say about where they are
placing you on the rank list.
For discussion on communicating with programs, please see: Applicant to
Residency Program Translation Guide
• Relax. The hard part is over.
• You have probably seen areas of the country on interviews you never
knew existed.
• Pay off your credit card bills.
WAITING

73
• Make sure you have done everything you need to graduate and get
excited!
Monday:
• Email from the NRMP at 12 noon EST: “Yes, you matched.” or “No, you did
not match.”
• Contains both PGY 1 and PGY 2-5 matches, or PGY 1-5/6 categorical.
• No information about where you matched.
Supplemental Offer and Acceptance Program (SOAP) – Follow instructions.
• SOAP is the process through which positions offered by
unfilled programs will be accepted by unmatched applicants
during Match Week.
• SOAP replaces the "Scramble" and provides a standardized and
uniform process for obtaining post- match appointments.
• All applications to programs are done via ERAS. Unmatched
candidates select programs via ERAS starting on the Monday.
Programs can contact candidates after reviewing applications.
Candidates do NOT contact programs directly.
• Positions offered and accepted during SOAP establish a binding
commitment enforced by the Match Participation Agreement.
For additional information, view How SOAP Works
Friday Match Day:
• Depends on the medical school:
° Breakfast or lunch.
° Applicants receive the envelopes containing their match,
privately, publicly, in-person, or online.
It’s not the end of the world. Though this is very stressful and not the result you would
have liked, take a deep breath, and start to think about your options:
• Assess your interview season honestly. Are there things that you think you
could have done better? Did you submit all your materials on September
MATCH WEEK!
I DIDN’T MATCH WHAT SHOULD I DO?

74
7? Did you rank >13 programs if you were applying by yourself and even
more if you were couples matching? Did you not rank some of the
programs that you interviewed at?
• What are the SOAP options for this application cycle? Do you think that if
you were to SOAP into a particular program you could potentially be
happy there (both in terms of the program and the geographic location) for
4 years?
• Have a frank discussion with your advisor. Gather their opinions on your
application relative to the degree of competition that you faced in your
particular year (some years are much more competitive than others and if
you were to redo everything exactly the same another year you may have
a different outcome).
• After introspection and gathering this information:
° If you believe that you can do better during the interview
season but also feel that you could be happy at a program in
SOAP, consider entering SOAP.
° If you do feel you did everything you could in the interview
season, there isn’t anything that you would change/ improve
upon, and if you would like to avoid taking a year off,
consider entering SOAP.
° There are websites like APDR, APDS
(https://apds.org/education-careers/open-positions/) which
lists open surgery or radiology positions that are still unfilled
after SOAP. These provide opportunity for candidates to
apply outside the NRMP match and can do so until June of
that year (3 months post-match results) after which if still
unmatched, will have to reapply at the following match cycle.
• Scenario: You do not want to go to any of the programs that are available
in SOAP or you entered SOAP and did not get one of the available
positions. Again, time for some introspection:
° Do you absolutely want to go into radiology or do you think
you would potentially be happy in another specialty? If you
definitely want to pursue radiology, immediately start thinking
about what you can do for the coming academic year that is
radiology-related and put in applications. This may be
research or even something related to product development
or consulting. Regardless, make sure that it’s something
where you should be able to get time to go on interviews
when you reapply. If you are considering another specialty
but would prefer radiology, consider dual applying next

75
season. Find a mentor in that field to help you develop a
reasonably competitive application.
• If you did not include a Step 2 score in your application the first time
around, take and do well on Step 2. This will help to prove to programs
that you are a strong applicant.
• When going through your second interview season for radiology, apply
more broadly to programs, including university and community programs
as well as programs in different geographic areas. Do not turn down any
interview invitations and rank every program where you interview.
° Have a discussion with your medical school to see if you
would be able to extend your time there for another year so
that you can apply as a student still affiliated with your
school. Historically unaffiliated applicants have had some
more difficulty matching. If this is not possible, again, not the
end of the world.
• There are 3 different scenarios to not matching into residency for a radiology
specialty applicant:
1. Matched into preliminary/ transitional year, but NOT
matched into radiology (Partial match): Candidates can enter
SOAP with the list of unmatched radiology programs and try
matching in SOAP. If unsuccessful at SOAP, you can keep
checking the APDR website (Association of Program Directors in
Radiology) (https://www.apdr.org/trainees/residency-
information/residents-seeking-positions) which allows for programs
posting open positions due to residents leaving the program for
relocation related to family reasons, and also unmatched residents
post on the website seeking radiology position. If still unsuccessful,
you can enter the consecutive year NRMP match while being in
intern year with stronger letters of recommendation from the intern
year program.
2. Matched into advanced radiology program, but NOT into
intern year program (Partial match): Candidates can enter SOAP
with the list of unmatched preliminary/ transitional year programs
and try matching in SOAP. If unsuccessful, you can do the same as
above by checking the APDS website (Association of Program
Directors in Surgery) (https://apds.org/education-careers/open-
positions/) which allows posting by the candidate seeking
preliminary surgery positions and also programs with open surgery
residency positions. If still unsuccessful at SOAP, the situation is
different from the above scenario because intern year matching is

76
mandatory to start an advanced radiology residency. So, if
candidate is unable to match into preliminary year by the start of
next academic year which July of that year when they have to start
intern year, you will have to contact the radiology program that you
matched into and in most situations, you will have to give up the
radiology program that you matched the following year as well.
Few programs might allow a month or more grace period to let you
find a preliminary/ transition year position. If that did not work, the
candidates have to enter into the next NRMP cycle for full
rematching process with both intern year and radiology program.
3. Did NOT MATCH INTO BOTH intern year program and
advanced radiology program: there are 2 options which
candidates have in this scenario.
▪ Option A: Try SOAP process and try at least to match into
preliminary/ transitional year (more important than trying to
match in radiology program in this scenario) and post SOAP
trying for the same until June of that year. If unsuccessful,
enter the NRMP match next year while boosting the CV with
more research/ academic activities.
▪ Option B: Try matching into different subspeciality in SOAP
if not willing to waste one more year before next NRMP
match, for example, Radiation oncology etc. (previous years-
nuclear medicine residency which is now merged into
radiology residency), which might be closer one to match
with ERAS application documents which reflect your interest
in radiology. However, the caveat is if the candidate is still
interested in entering radiology residency at later date, this
step complicates it. Once the candidate signs the offer from
a different specialty residency program, they are not eligible
to enter the traditional NRMP match in the subsequent
years. However, the candidate can switch residencies in
second year if any radiology position opens up elsewhere
but with consent and approval from your current enrolled
program. So, candidates might think twice before choosing
this option.
In conclusion, this is not a black and white process.
FINAL ADVICE

77
• Opinions vary and you will hear many different ways of attacking the
residency application process.
• Follow your gut and do what you think is right.
• Be your own advocate - applying to residency is not a passive process.
• Be strong and positive - it IS better on the other side of medical school!
• Read and know a radiology book for medical students at the end of intern
year so that you can hit the ground running.
Best wishes!!
The following online resources are that of the opinions of the authors. These online
resources are not validated or endorsed by AMSER or AUR. The goal is to offer
potentially helpful resources, with an understanding that the information and application
process is ever changing.
1. American Medical Association (AMA) FREIDA
TM
Ability to search residency and fellowship programs that are accredited by the
Accreditation Council for Graduate Medical Education (ACGME).
2. Residency Explorer Tool
TM
Tool
This tool allows one to explore and compare residency programs in 23
specialties as well as compare an individual’s profile to applicants who matched
at each program.
3. Texas STAR (Seeking Transparency in Application to Residency)
Powered by UT (University of Texas) Southwestern Medical Center. This
nationwide survey and online tool, administered by UT Southwestern Medical
School, allows medical school deans, advisors, and fourth-year medical students
access to real application data of recently matched fourth-year medical students.
This database allows students to better target their applications to programs that
they are more likely to receive interviews and ultimately match into.
4. National Resident Matching Program (NRMP®) 2022 Main Residency Match
®
-
This pdf report contains statistical tables and graphs for the Main Residency
Match
®
and lists by state and sponsoring institution every participating program,
the number of positions, the number of positions offered, and the number filled.
ONLINE RESOURCES

78
SOAP
®
data also are presented.
5. APPS OF STEEL - TeamRads.com. Guide to matching into radiology and other
matches from the perspective of Donna Magid, MD, M.Ed, FAUR
6. TheRadRoom - Centralized resource for those interested in radiology and are
applying to diagnostic/interventional radiology residency. Recent launch of a
series known as Program Director Tip of the Day with tips/advice from Program
Directors and Associate Program Directors regarding common questions
applicants have.
Charting Outcomes in the Match, 2022: These reports document how
applicant qualifications affect match success. Ten to twelve measures are
examined in the reports, including the number of contiguous ranks in preferred
specialty, the number of distinct specialties ranked, USMLE® Step 1 and Step 2
CK scores (for U.S. allopathic seniors and IMGs), COMLEX-USA® Level 1 and
Level 2-CE scores (for osteopathic seniors), and the numbers of research
experiences, publications, and work and volunteer experiences.
• Charting Outcomes in the Match for U.S. MD Seniors:
Characteristics of U.S. MD Medical School Seniors Who
Matched to Their Preferred Specialty in the 2022 Main
Residency Match (3
rd
edition) (PDF, 220 pages)
• Charting Outcomes in the Match for U.S. DO Seniors:
Characteristics of U.S. DO Medical School Seniors Who
Matched to Their Preferred Specialty in the 2022 Main Residency
Match (3
rd
edition) (PDF, 222 pages)
• Charting Outcomes in the Match for International Medical
Graduates: Characteristics of International Medical Graduates
Who Matched to Their Preferred Specialty in the 2022 Main
Residency Match (4
th
edition) (PDF, 294 pages)
List of ACGME Accredited DR Residency Programs
List of ACGME Accredited IR Residency Programs
Fellowship and Residency Electronic Interactive Database (FREIDA)
Electronic Residency Application Service (ERAS)
National Resident Matching Program (NRMP)
Doximity Residency Program Ranking
