
Service Evaluation of the Elton John AIDS
Foundation’s Zero HIV Social Impact Bond
intervention in South London:
An investigation into the implementation and sustainability
of activities and system changes designed to bring us closer
to an AIDS free future.
Alec Fraser, Clare Coultas & Alexis Karamanos
Final report March 2022

2
Table of Contents
Acknowledgements ................................................................. 3
About the authors ................................................................... 4
Foreword .......................................................................... 5
Executive Summary ................................................................. 7
Introduction........................................................................ 9
Methodological and theoretical approach .............................................. 11
Qualitative approach ............................................................ 12
Quantitative approach........................................................... 12
Ethics ........................................................................ 13
Theoretical approach............................................................ 14
Zero HIV SIB programme background ................................................. 15
Findings .......................................................................... 16
Evaluating the impact of the Zero HIV programme .................................... 16
Evaluating the processes through which the Zero HIV programme functioned ............. 25
Narrative overview .............................................................. 25
Defining the Zero HIV SIB-financed ‘intervention’ .................................... 27
Secondary Care.................................................................... 30
Opt-out HIV testing in the ED ..................................................... 30
LTFU work in the hospital setting .................................................. 35
Primary Care ...................................................................... 38
Awareness Raising.............................................................. 38
Opt-in HIV testing in Primary Care ................................................. 39
LTFU and HIV Support in Primary Care ............................................. 40
Community Care ................................................................... 42
Sustainability...................................................................... 44
Conclusions ....................................................................... 47
References ....................................................................... 50

3
Acknowledgements
This service evaluation is supported by the National Institute for Health Research (NIHR) Applied
Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS
Foundation Trust. The views expressed are those of the authors and not necessarily those of the NIHR or
the Department of Health and Social Care.
The authors received funding to support this work from the King’s Business School Research Incubator
Fund in October 2020 and an Impact Fund award in February 2022. We are very grateful to the
KBS Research support team for all their help with this service evaluation and their patience as we
experienced delays linked to COVID-19.
We would like to thank all the research participants who kindly agreed to give up their time to be
interviewed throughout this service evaluation and also answered questions informally at times over the
past year or so.
Thank you to Professor Peter Littlejohns of King’s College London for help and guidance in the
establishment of this service evaluation. Thanks to Clare FitzGerald of King’s College London and
Richard Boulton of Kingston & St George’s University of London for help and advice as the project
developed.
Many thanks also to Steve Hindle, Social Impact Bond Performance Manager, Elton John AIDS
Foundation and Neil Stanworth, Director, ATQ for support throughout the project and for commenting on
earlier drafts of this report.
The interpretation of all the data remains that of the authors.
Please cite this report as Fraser, A., Coultas, C., & Karamanos, A. (2022) Service Evaluation
of the Elton John AIDS Foundation’s Zero HIV Social Impact Bond intervention in South London:
An investigation into the implementation and sustainability of activities and system changes
designed to bring us closer to an AIDS free future. Final Report, King’s College London.

4
About the authors
Dr Alec Fraser is a Lecturer in Government & Business at King’s College London (KCL). He is a member
of the Public Services Management and Organisation Group within the King’s Business School. Alec’s
research centres on the use of evidence in policy making and practice across the public sector with a
particular focus on health and social care. He has extensively researched the development of Social
Impact Bonds and Outcomes-Oriented Reforms in public service delivery in the UK and internationally
over recent years. He previously spent five years at the Policy Innovation Research Unit at the London
School of Hygiene and Tropical Medicine. Prior to entering academia, he worked in NHS administration
and management. He has an MA in Public Policy and a PhD in Management - both from KCL.
Dr Clare Coultas is Lecturer in Social Justice in the KCL School of Education, Communication and
Society, and a is postdoctoral researcher in the South London Applied Research Collaboration (ARC),
based at the KCL Institute of Psychiatry, Psychology, and Neuroscience. Grounded in her experiences
of working as a third-sector research, evaluation, and development practitioner in the UK and East and
Central Africa, Clare’s research focuses on developing practice-based evidence on the change potentials
of people, organisations, and institutions using ethnographic, qualitative, and participatory methods.
Clare holds a PhD in Social Psychology from the London School of Economics and Political Science, and
an MSc in International Primary Health Care and BSc in Human Sciences, both from University College
London.
Dr Alexis Karamanos is a Population Health Analyst for the London Borough of Hackney and the City
of London, and a visiting Research Associate in Social Epidemiology and Public Health at King’s College
London. He is interested in the social, economic, and political determinants of human development, and
health inequalities over the life course. Alexis holds an undergraduate degree in Political Science and
Public Administration from the National and Kapodistrian University of Athens, Greece. He also holds
an MSc in Health and Society: Social Epidemiology from University College London (UCL), which was
funded by the Onassis Foundation, and a PhD in Population Health from UCL which was funded by the
UK Economic and Social Research Council (ESRC).

5
Foreword
The Zero HIV Social Impact Bond was the Elton John AIDS Foundation’s response - despite excellent
clinical care within the health system - to the seemingly intractable problem of continued undiagnosed/
late HIV diagnosis in England. When I first started talking back in 2015 with interested people from
Lambeth council, NHS England, and NHS clinical colleagues about the potential of creating the world’s
first ever HIV SIB to expand testing and linkage to care, I was confident that we could make an impact.
But what an impact! Over 460 people have been either newly diagnosed with HIV or reengaged into care
across South London, providing access to lifesaving treatment, preventing onward transmission of HIV,
and avoiding over £90m of costs to the healthcare system.
Our partnership with Terrence Higgins Trust and National Aids Trust in developing the HIV Commission,
so ably chaired by Dame Inga Beale, gave a great opportunity for us to share the learning from the SIB.
The HIV Commission 2020 report emphasised the importance of HIV testing at every opportunity. In
response the government committed to develop the HIV Action Plan, giving us the chance to lay out our
evidence to DHSC and the Action Plan taskforce. The HIV Action Plan, launched by the Dept of Health
last December, committed £20m for the roll out of opt out ED HIV testing in very high areas of HIV
incidence, the first new HIV funding in many years, as well as annual reporting of progress to Parliament.
As this service evaluation shows, we now have the evidence that opt out ED and primary care HIV
testing reaches those members of the community who do not currently come into contact with HIV
testing services anywhere else. In particular the SIB highlighted inequities for rates of diagnosis and
reengagement in care for minority groups and amongst women and older people We were able to
contextualise this data against related health and social care needs, thus informing broader planning
for service delivery by Integrated Care Systems and local authorities. The SIB also highlighted missed

6
opportunities for new HIV diagnoses and the critical need to reengage many patients living with HIV
who are Lost to Follow Up. SIB partners reengaged over 250 people back into treatment, improving their
health and wellbeing, avoiding potentially expensive hospital treatment, and contributing to the HIV
Commission goal of Zero HIV transmissions by 2030.
As you will see, the SIB approach itself brought benefits. Its structure allowed for considerable flexibility
and innovation by implementing partners, matched as it was with the reassurance of upfront payments.
A laser focus on outcomes saw greater collaboration across dierent clinical teams and the creation of
HIV GP Champions energised opt out testing services in primary care. It has been truly heart-warming
to hear this feedback which underscores the importance of collaboration and consensus across
stakeholders.
I would like to thank our partners in the hospitals, primary care and community organisations for their
amazing work; our funding partner The National Lottery Community Fund, our investors from Comic
Relief, Big Issue Invest and Viiv Healthcare; and commissioners in the Public Health teams at Lambeth,
Southwark and Lewisham councils; the team at NHS England and Public Health England (in their
new homes at UKHSA and OHID), the legal team at Freshfields Bruckhaus Deringer for their pro bono
support and Maclaren Consulting for developing our PowerBI management and reporting system.
We are deeply grateful to all those involved in the project and those who have created this evaluation
report. We look forward to a national roll out to continue this vital work.
Anne Aslett
Chief Executive Ocer of the Elton John AIDS Foundation
March 2022

7
Executive Summary
This service evaluation takes a combined qualitative and quantitative methodological approach to
explore an innovative public health intervention with significant public management implications in
South London. The intervention is known as the ‘Elton John AIDS Foundation Zero HIV programme’ (we
term it the Zero HIV SIB programme in this report). The intervention ran in the boroughs of Lambeth,
Southwark, and Lewisham from November 2018 until the end of December 2021. The goals of the
intervention include improving a person living with HIV’s health outcomes by linking them into HIV
treatment either as a new diagnosis or through re-engagement with NHS services (if already diagnosed
but not receiving treatment) before their condition deteriorates, slowing the spread of HIV through
avoiding future transmission and saving the NHS money in future years.
The intervention was financed through a novel Social Impact Bond (SIB) mechanism. A SIB is an
outcomes-based contract, in which a commissioner pays a contractor for certain measurable outcomes.
A key facet of the SIB approach is to encourage multi-agency collaboration across public, private, and
philanthropic partners (Carter et al, 2020). A deeper understanding of these collaborations – how they
work, their strengths and weaknesses – is very important for informing wider commissioning decisions
not only in HIV but across other chronic diseases.
We find that the 3-year Zero HIV SIB programme has been eective in both (1) delivering improved
health outcomes for people living with HIV and (2) improving inter-organisational collaboration and
service collaboration across what has historically been a rather fragmented HIV healthcare ecosystem in
South London.
In terms of the health impacts, key actors expressed confidence that this programme had reached (i)
people living with HIV who were previously undiagnosed and brought them into contact with specialist
NHS services and (ii) people living with HIV who were previously diagnosed but had become ‘lost to
follow-up’ (LTFU) treatment services. However, the absence of robust baseline data for key outcomes
or a commitment to a counterfactual evaluation design means it is not possible to attribute outcomes to
specific interventions.
Data from EJAF show that 124 new HIV diagnoses were identified through ED testing, and 53 LTFU
patients were also identified through participating EDs in South London hospitals. These hospitals also
re-engaged a further 153 LTFU patients separate to ED testing. Primary Care providers identified 26 new
HIV diagnoses through GP testing and also re-engaged 45 LTFU patients. Finally, 46 new diagnoses were
made by community providers and 5 LTFU patients were re-engaged by community providers as part of
the Zero HIV programme.
In terms of the organisational impacts, key actors expressed confidence that this programme
successfully mitigated many of the traditional organisational and financial factors that had led
to fragmented HIV services in South London through (i) improved inter-organisational network
working – both formal and informal in nature through boundary spanning activities and a pervading
‘cosmopolitanism’ (Greenhalgh et al, 2004; Damschroder et al, 2009). In addition to this, informants
perceived the increased use of data and monitoring and the realignment of incentives as positively
promoting collaboration and better outcomes. In terms of financing (ii) the programme very eectively

8
negated many aspects of the existing siloed payments systems for various aspects of HIV services which
actors felt had stymied attempts for providers to implement evidence-informed practice (for instance
in relation to ED and Primary Care testing), or to adapt to practical realities (such as identifying LTFU
patients and providing more flexibility for not-for-profit provider organisation outreach work).
The programme adapted and grew over the three years with new provider organisations recruited
over the lifetime of the programme and new emphases on delivery developed – for example through
the expanded use of GP champions. This adaptability proved to be very beneficial in relation to the
COVID-19 outbreak in early 2020 (see Stanworth, 2022) and presaged a pivot to greater LTFU work.
Community providers welcomed the flexibility that the programme aorded them overall, though issues
were noted by some providers in relation to how SIB-financed work may have been seen to duplicate
existing work commissioned more conventionally.
The role of EJAF was praised by informants. The organisation played a key boundary spanning function
and delivered leadership, support, and encouragement to other organisations. EJAF were crucial
players in the design, financing, and delivery of the programme acting as co-commissioners, financial
intermediaries, project managers, and data analysts. EJAF successfully disrupted many of the existing
inter-organisational, financial, and institutional barriers that historically inhibited more systematic
implementation of testing, LTFU and better joined-up HIV service provision. EJAF were instrumental
in shaping an ‘outer context’ (Damschroder et al, 2009) conducive to improving HIV services in South
London.
Rather than one ‘intervention’ the qualitative data in this report highlight that the actors involved
in commissioning and delivering HIV services through the Zero HIV SIB programme felt they were
delivering a suite of ‘interventions’. Some of these have a strong existing evidence base and have been
recommended in existing guidelines whilst others are more organisational and pragmatic. Some were
new and developed as part of the Zero HIV SIB programme whilst others were already in existence in
some or other settings. A key finding is increased flexibility and local discretion to use funds to tailor
services more closely to the needs of those using services as we have seen in other health focused SIBs
in the UK (Fraser et al, 2018).
A central aim of the Zero HIV SIB programme was to further the evidence for these interventions and
change practice going forward. A criticism of the programme raised by some informants was that more
work could have been done to ‘baseline’ existing practice and prove the attribution of some of these
interventions in order to provide a more robust body of evidence to sustain these going forward once the
SIB financing ended in December 2021. Though beyond the scope of this current service evaluation, it
appears that learning from the programme (particularly in relation to ED testing) may have been used to
inform national and local level policymakers in future HIV policy development.
There are mixed views from informants in relation to the sustainability of the improvements to South
London HIV services delivered through the Zero HIV SIB programme after the SIB-financing is gone.
More research is needed to follow these developments over the coming years.

9
Introduction
This service evaluation takes a combined qualitative and quantitative methodological approach to
explore an innovative public health intervention with significant public management implications in
South London. The intervention is known as the ‘Elton John AIDS Foundation Zero HIV programme’. The
goals of the intervention include improving a person living with HIV’s health outcomes by linking them
into HIV treatment either as a new diagnosis or through re-engagement with NHS services (if already
diagnosed but not receiving treatment) before their condition deteriorates, slowing the spread of HIV
through avoiding future transmission and saving the NHS money in future years. It was developed by
the Elton John AIDS Foundation, in partnership with Lambeth local authority and NHS England, and
received support from the National Lottery Community Fund. The intervention ran in the boroughs of
Lambeth, Southwark, and Lewisham from November 2018 until the end of December 2021.
The intervention was financed through a novel Social Impact Bond (SIB) mechanism. It was the first
SIB in the world to focus on HIV treatment and care. A SIB is an outcomes-based contract, in which a
commissioner pays a contractor for certain measurable outcomes. The outcomes (diagnosing new cases
of HIV and re-engaging patients who dropped out of HIV care) have significant beneficial social impacts as
well as hypothetical cost-savings for the NHS. A key facet of the SIB approach is to encourage multi-agency
collaboration across public, private, and philanthropic partners (Carter et al, 2020). A deeper understanding
of these collaborations – how they work, their strengths and weaknesses – is very important for
informing wider commissioning decisions not only in HIV but across other chronic diseases.
This service evaluation is informed by an Implementation Science approach (Damschroder et al,
2009) to explore the impacts and implications of the Zero HIV programme from the perspectives of
service users, clinical sta, health service managers, local authority commissioners, private sector, and

10
philanthropic stakeholders. The evaluation also explores questions in relation to the sustainability of the
intervention beyond the end of the SIB financing in December 2021.
The overall objective of the evaluation is to learn more about the processes, impacts and sustainability
of the Zero HIV intervention through combined research methods. These principally include semi-
structured interviews with individuals who receive the services through the intervention, those who
deliver the intervention, those who design and oversee the intervention, those who commission the
intervention, and those who have provided finance for the intervention. Alongside interviews, the
evaluation also draws on relevant documentary sources and anonymized descriptive statistical information.
The qualitative element of the evaluation focuses on the following research questions:
1. What do key stakeholders perceive to be the organisational and health impacts of the
Zero HIV intervention?
2. Through what mechanisms, how, and why, does the Zero HIV intervention impact upon the
behaviour, attitudes, and actions of:
(a) Service users?
(b) NHS and non-NHS providers?
(c) NHS and Local Authority commissioners?
(d) Wider stakeholders including those involved in financing, evaluating, and overseeing the Social
Impact Bond element of the intervention?
3. How might these impacts and behaviour changes be sustained:
(a) In South London after the SIB financed programme ends in December 2021?
(b) And/or transferred to other geographical settings?
The quantitative element of the evaluation focuses on the following research questions:
1. Are there any ethnic, sex and age dierences in the likelihood of being diagnosed?
2. Are there any ethnic, sex and age dierences in the likelihood of being re-engaged?
3. Are there any ethnic, sex and age dierences in the likelihood of non-engagement in treatment (e.g.,
found through ED testing “non-contactable,” or even re-attending at ED)?
The current report will provide an overview of the key responses to these research questions. Further
analysis will be performed on the data collected leading to submissions of papers to academic journals.
It is anticipated that the research team will conduct further research in South London in order to explore
qualitative research question 3 (a) above more fully. The current report does not directly evaluate the
impact and eectiveness of the SIB financing mechanism as this is explicitly evaluated by another
research team led by Ecorys and ATQ (see Stanworth, 2020; 2022). However, the report does explore
some of the links of how the financing mechanism impacts upon the delivery of the health interventions.
This report does not explore the cost-eectiveness or health economic impacts of the programme.

11
Methodological and theoretical approach
Qualitative approach
This service evaluation follows a case study approach (Yin, 2009; Eisenhardt, 1989) to explore
the perceptions of key actors in relation to the nature, impacts and sustainability of the Zero HIV
intervention. A qualitative case study approach is appropriate for exploring issues related to policy
implementation (Fraser & Mays, 2020), exploring ‘how’ and ‘why’ questions about phenomena
through detailed contextualised accounts of a case (Yin, 2009). Interviews were conducted until “data
saturation” (Glaser & Strauss, 1967) and were recorded, translated, transcribed, and coded using
NVivo 12. Members of the research team discussed and reviewed the interview data alongside relevant
documentary material to ensure consistency.
We conducted 31 interviews overall, principally through the Summer and Autumn of 2021. Most
interviews took place via MS Teams given the ongoing COVID-19 pandemic. We purposively sampled
informants to a wide selection of relevant viewpoints. Most interviews lasted an hour. We used an
interview schedule that asked informants about their professional background, work history, and asked
them to provide an overview of their understanding of the Zero HIV intervention and the barriers and
facilitators linked to this. We discussed prospective opportunities and challenges faced in the roll-out
and development of the intervention whilst allowing informants the space to express their own narratives
(Fontana and Frey, 2000).
Table 1: Interview informant data
Role Number of
informants
Number of organisations
represented
Community organisation outreach worker (strategic,
operational, and patient-facing responsibilities)
4 4
SIB investor 2 2
GP (HIV champions) 3 3
HIV patient 2 N/A
EJAF (strategic, operational and data management
responsibilities)
4 1
NHS hospital sta (including nurses, doctors, managers,
both HIV and non-HIV specialists – e.g. A&E sta)
9 3
Project evaluator 1 1
Local commissioners (CCG and/or LA) 4 2
National commissioners 2 2
The data were interrogated repeatedly in order to understand key emergent issues drawing on the
principles of ‘constant comparison’ (Glaser, 1965). The analytical approach drew on both inductive
and deductive reasoning (Langley, 1999) – exploring emergent issues alongside insights from wider
implementation science theory (Damschroder et al, 2009). Whilst “recall bias” may be a problem in
relation to retrospective interviews with some stakeholders, retrospective interviews can also have
benefits – such as encouraging informants to critically appraise the original rationale for decisions
relating to policy and practice.

12
Quantitative approach
Data
In this secondary data analysis, we use data from 2,388 individuals aged 15 and over in 29 London
borough councils between August 2018 and December 2021.
Outcome
The outcome of interest includes information for individuals who were known positive (N=1,512) during
the study period. This forms the baseline category of this analysis against which information from other
categories is compared. These categories are formed by those who were newly diagnosed (N=223),
those who were re-reengaged to treatment (N=249) and those who were not being able to be contacted
(N=121). There was missing information on the outcome of interest for 257 individuals.
Demographic variables
Information on sex and age categories (35-49 years was used as the reference category) was used.
UK Health and Security (UKHSA), formerly known as Public Health England, ethnic categorisation
information was also used (White, Black African, Black Caribbean, Black other, Asian, and Mixed).
Information on London borough council residence was collapsed to four categories (Lambeth, Lewisham,
Southwark and Other) since ~80% of the sample was from Lambeth, Lewisham, and Southwark.
Statistical analysis
For descriptive reasons, we first explored the probability of each outcome category by age and
ethnicity. Further, we applied multivariable multinomial logistic regression modelling to identify
characteristics that have a greater probability of being newly diagnosed, re-engaged with treatment
and being non-contactable compared to those who were known positive. Particularly, the ratio of the
probability of being newly diagnosed or re-engaged with treatment or not being able to be contacted
over the probability of being known positive (baseline category) is expressed as relative risk. When a
characteristic/variable has a relative risk ratio (RRR) of one, this means there is neither an increase nor
a decrease in the probability of choosing one of the modelled outcome categories compared with the
baseline category. A RRR greater than one indicates an increased probability of choosing one modelled
outcome category compared with the baseline category. A RRR lower than one indicates a decreased
probability of choosing one modelled outcome category compared with the baseline category. We opted
for a single model, which produces the most accurate representation of the eect of each of the core
demographic (age, sex, Ethnicity and London borough council) characteristics on the probability of being
newly diagnosed or being re-engaged with treatment or being able to be contacted relative to being known
positive. It is worth mentioning that we decided not to adjust for the Index of Multiple Deprivation (IMD-a
measure highlighting area deprivation) since most of our sample comes from economically deprived areas
(more than 70% of the sample comes from the top 30% of area deprivation).
13
Ethics
We submitted our study protocol for review by the Guy’s and St Thomas’ NHS Foundation Trust
Research & Development governance team in March 2020. They recommended our work be defined
as a ‘service evaluation’ and advised that it therefore did not need formal IRAS/NHS ethical approval.
Where appropriate we secured site specific NHS R&D approval for the qualitative elements of the
service evaluation. All participants in the qualitative part of the research received detailed participant
information sheets and were formally asked for consent before taking part.
In addition, we developed a formal data use agreement between KCL and EJAF to ensure robust
governance in relation to the use of quantitative data for this report and subsequent academic outputs.
Theoretical approach
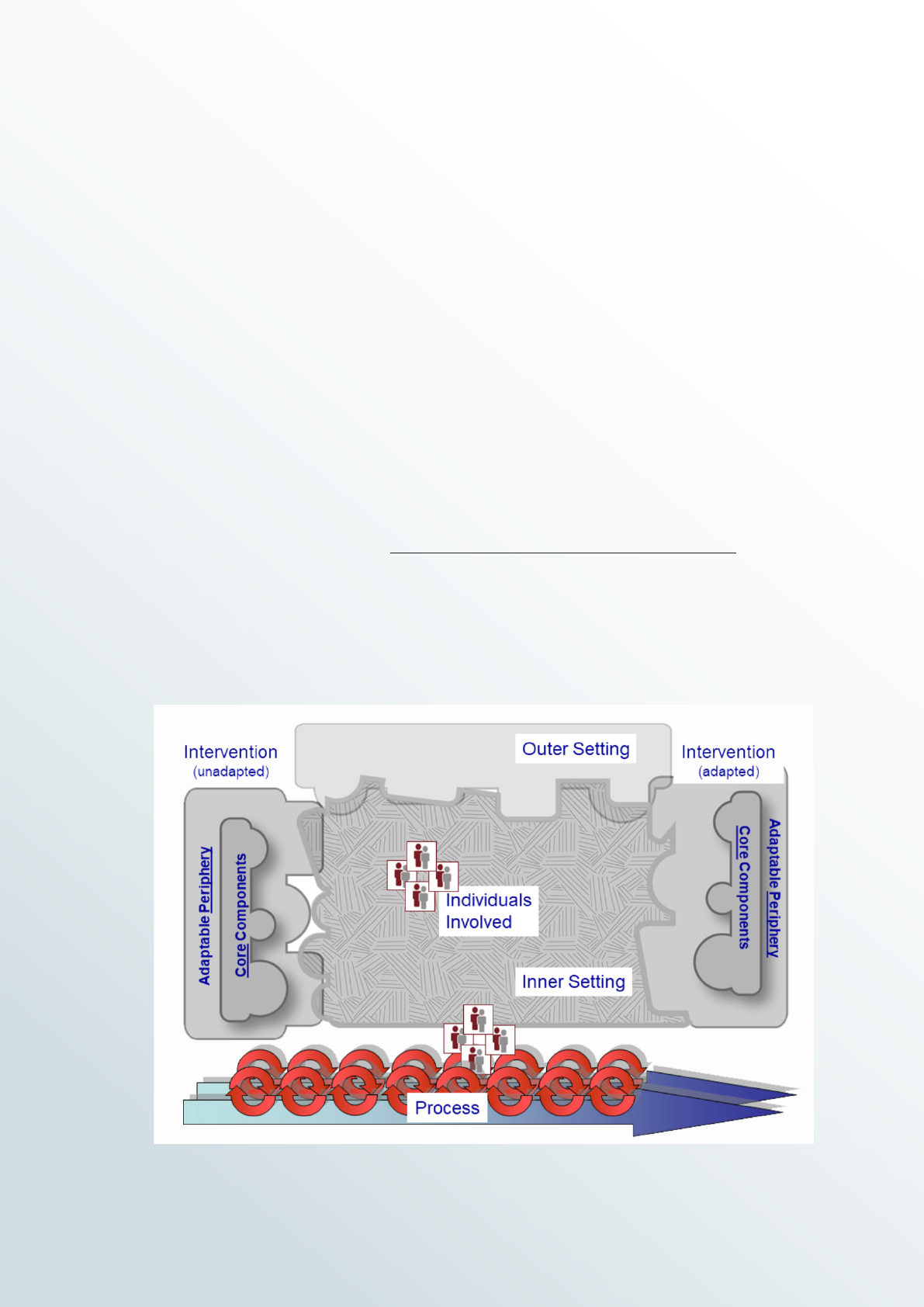
Our study design is influenced by the Consolidated Framework for Implementation Research (CFIR)
framework pioneered by Laura Damschroder and colleagues (Damschroder et al, 2009). The CFIR is
structured around five ‘constructs’. These are (1) intervention characteristics (2) outer setting (3) inner
setting (4) characteristics of individuals (5) implementation processes.
Figure 1: The CFIR

14
The qualitative data generated by the service evaluation interviews were analysed using key components
drawn from the CFIR. This enabled a clear and theoretically informed framework to interrogate:
1. the characteristics of the intervention (or interventions) developed as part of the Zero HIV
programme by dierent actors over time and across dierent settings
2. the wider financial, strategic, and operational context developed to coordinate the intervention(s)
3. the dierent relationships and interactions at the micro-level focused on delivery of the
intervention(s)
4. the importance of key personal characteristics of individuals designing, delivering, or monitoring the
intervention(s)
5. the important processes involved in promoting and/or inhibiting the delivery of the intervention(s).
Future academic outputs will explore these five constructs in greater detail than we do in this current
report – however the analyses included here are driven by key CFIR ideas. It is also worth noting
some important inductive codes not covered by the CFIR. This included definition of the Zero HIV SIB
programme interventions, the impact of COVID-19, HIV stigma, and issues related to post-SIB-financing.

15
Zero HIV SIB programme background
This service evaluation explores important Public Health and Public Management questions. In relation
to Public Health, the service evaluation reflects if and how the Zero HIV intervention reached hard-to-
reach populations with HIV – either those who have never been tested or who have stopped attending
treatment. This work has important implications for health equity. We know that anti-retroviral therapy
(ART) for those with HIV is highly eective enabling individuals to live long and healthy lives. There
are massive benefits to individuals if they can be diagnosed and start to receive treatment, but Public
Health England (PHE) estimates that about 6% of the 105,200 people living with HIV are unaware of
their condition (PHE, 2019). The earlier that diagnosis occurs the better, as over time the undiagnosed
virus may damage the immune system and general health. PHE data show that 43% of those diagnosed
in 2018 were diagnosed late, with late diagnosis being much higher among certain groups (PHE,
2019). Beyond the individual health benefits of early diagnosis and ongoing treatment of HIV there are
significant wider public health benefits as eective treatment reduces the risk that the infected person
can pass on the virus to almost zero. These individual and population level health benefits may also
be expected to have wider financial benefits for the health system by keeping those with HIV healthy
and also reducing the likelihood of further onward transmission of the disease. As Stanworth (2022)
highlights – whilst there is no recent independently validated estimate of the scale of such benefits,
calculations made by the Elton John AIDS Foundation suggest that they amount to an estimated
£220,000 per person, based on £140,000 of cost avoided through treatment, and £80,000 avoided by
reduced onward transmission.
In relation to Public Management, a key interest here is the novel Social Impact Bond (SIB) financing
mechanism. This is the first SIB in the world to focus on HIV treatment and care. SIBs are hugely
interesting from a public policy and management perspective (Fraser et al, 2018) sitting at the vanguard
of policies designed to foster an outcomes-based focus in public service commissioning and delivery
(Edmiston & Nicholls, 2018). A key facet of the SIB approach is to foster multi-agency collaboration
across public, private, and philanthropic partners (Blundell et al, 2019). The Zero HIV programme brings
together the Elton John AIDS Foundation, Lambeth Council, Southwark Council, Lewisham Council, NHS
England, NHS Improvement the National Lottery Community Fund, ViiV Healthcare, Comic Relief, and
Big Issue Invest to work with local NHS Trusts, Primary Care and Community providers to collaboratively
tackle problems related to people living with undiagnosed HIV across Lambeth, Southwark, and
Lewisham. A deeper understanding of these collaborations – how they work, their strengths and
weaknesses – is very important for informing wider commissioning decisions not only in HIV but for
other chronic diseases too.

16
Findings
Evaluating the impact of the Zero HIV programme
We firstly present an overview of the impact of the Zero HIV programme through a series of textboxes
and discuss some of the key quantitative findings before moving on to the qualitative findings of the
service evaluation.
ED TESTING IMPACTS
124 people were diagnosed with HIV and linked to care, and a further 53 people living with HIV
were reengaged into care following ED HIV testing. Of these 55% were Black African, Black
Caribbean or Black Other community members, which when compared with the 22% of new
diagnoses from these communities reported in the Public Health England ‘London HIV Spotlight’
(2018) (Black African, Black Caribbean data only), suggests that ED HIV testing is extremely
good at reaching communities who may not otherwise be tested, either through not using
services where HIV testing is oered, or by avoiding testing through fear of HIV stigma. Late
outcomes (CD4 count <350) were 74% of new diagnoses and 81% of reengagements, suggesting
that ED HIV testing is finding people who are at serious risk of needing extensive treatment and
developing AIDS defining diseases and linking them to care.
ED HIV testing has a health inequalities element, with 50% of all those newly diagnosed living in
areas within the two lowest deciles of the Index of Multiple deprivation see figure 2.
(Data from EJAF)

17
Figure 2: Patient Total by Ethnicity, Index of Multiple Deprivation (IMD) Decile
(where 1 is most deprived 10% of LSOAs) (bins) (groups)
LTFU WORK BY HOSPITALS
A total of 153 people were reengaged through hospital HIV clinic recall work. 71% were from
Black African, Black Caribbean and Black Other communities, which suggests that LTFU work is
particularly helpful in reaching people from this community, who may have left care because of
HIV stigma as well as other life challenges. For the LTFU group as a whole, 53% had a CD4 count
of <350, suggesting that this is a cohort of people who were at risk of serious illness and expensive
utilisation of hospital resources.
(Data from EJAF)
Not known &
Not stated
Other
White &
White other
Black African &
Black Carribean
& Black other
54.0%
57.1%
61.1%
33.3%
66.7%
33.3%
33.3%
28.6%
27.8%
9.5%
21.0
3 4 5 6 7 81 & 2
50.0
18.0
9.0
3.0
2.0
1.0
24.0%
14.0%
8.0%

18
As can be seen in figure 3, the risk of LTFU is highly correlated with where someone lives and using the
Index of Multiple Deprivation suggests that this work is highly eective in engaging those people who are
already experiencing significant health inequalities (data from EJAF).
Figure 3: Index of Multiple Deprivation (IMD) Decile (where 1 is most deprived 10% of LSOAs) (bins)
(groups)
Asian
Other
White &
White other
Black African &
Black Carribean
& Black other
74.0%
72%
10%
20%
10%
7%
29
72%
67%
33%
9
25
67%
40%
40%
3 4 5 7 61 & 2
19.0%
7.0%
68
PRIMARY CARE NEW DIAGNOSES AND LTFU
36 new diagnoses, and 45 reengaged patients were identified through testing and LTFU work done
by the primary care providers involved in the programme.
(Data from EJAF)

19
IMPACT OF COMMUNITY ORGANISATIONS
This intervention led to 46 people being newly diagnosed, and 5 people being reengaged into
care. Providers that targeted Latin American community members were especially successful
contributing 32 new outcomes and one reengagement, suggesting that this is a community that is
particularly underserved through current arrangements.
(Data from EJAF)
Bringing these data together, there are a number of points we can make about the impact of the Zero
HIV programme. Firstly, in terms of the age of people living with HIV identified in the programme we
may say the following. Older participants identified by the programme were more likely to be known
to be HIV positive. Those aged 15-34 years were more than twice as likely to be newly diagnosed as
SIB participants aged 35-49 and 50 years and over. Participants aged 35-49 years were more likely to
be re-engaged to care than participants aged 15-34 years and 50 years and over. There was a higher
probability of not being able to be contacted for participants aged 15-34 years than older participants,
however 95% confidence intervals slightly overlapped (this is probably due to the small sample of SIB
participants who could not be contacted).
20
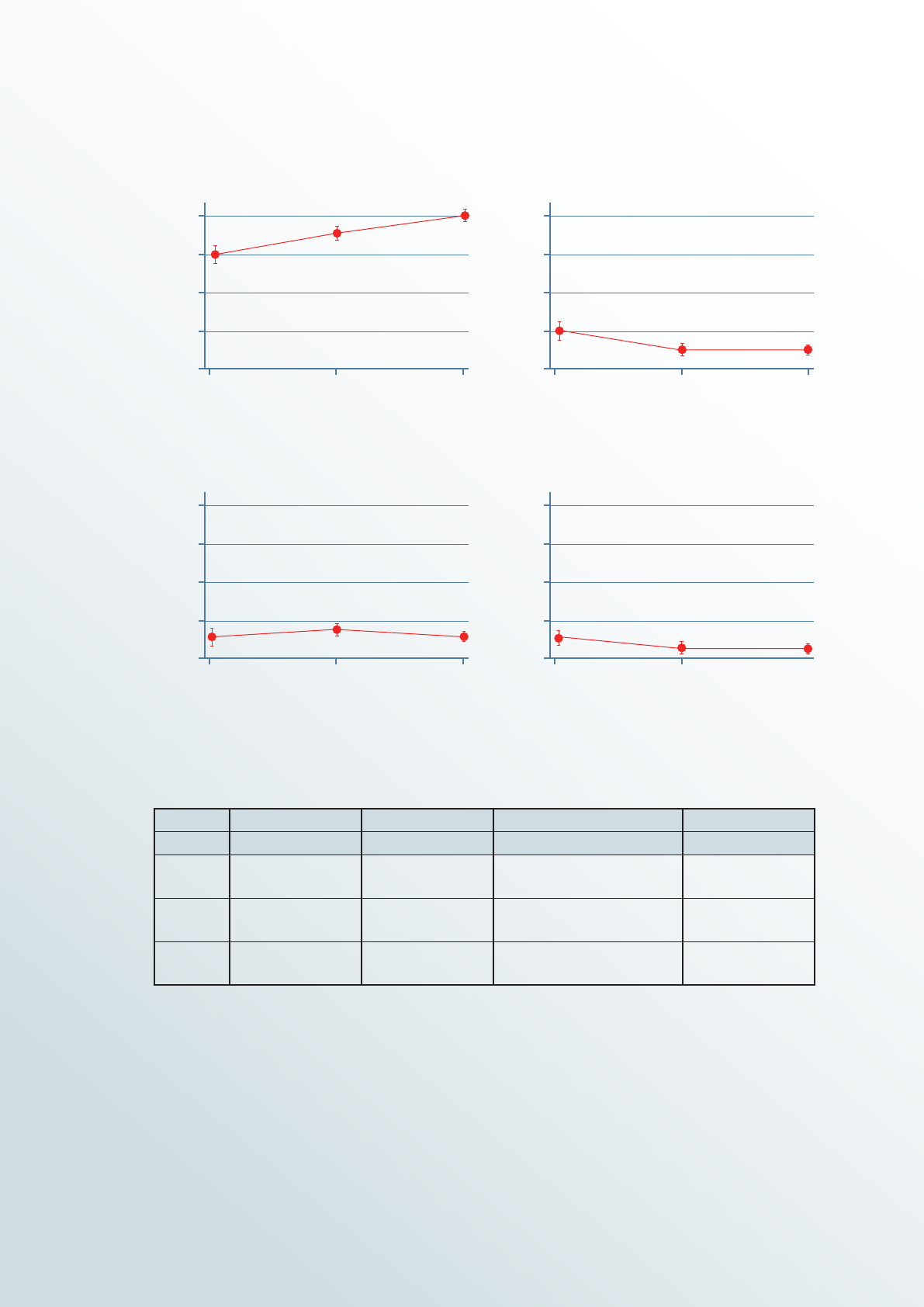
Table 2: Unadjusted predicted probabilities of outcomes by age group
Known positive New diagnosis Re-engagement to care Non-contactable
Pr [95% CI] Pr [95% CI] Pr [95% CI] Pr [95% CI]
15-34
0.61
[0.56, 0.67]
0.20
[0.16, 0.25]
0.10
[0.07, 0.13]
0.09
[0.06, 0.12]
35-49
0.7
[0.67, 0.73]
0.1
[0.07, 0.11]
0.16
[0.13, 0.18]
0.05
[0.03, 0.06]
50+
0.78
[0.75, 0.80]
0.08
[0.07, 0.10]
0.09
[0.07, 0.11]
0.05
[0.04, 0.06]
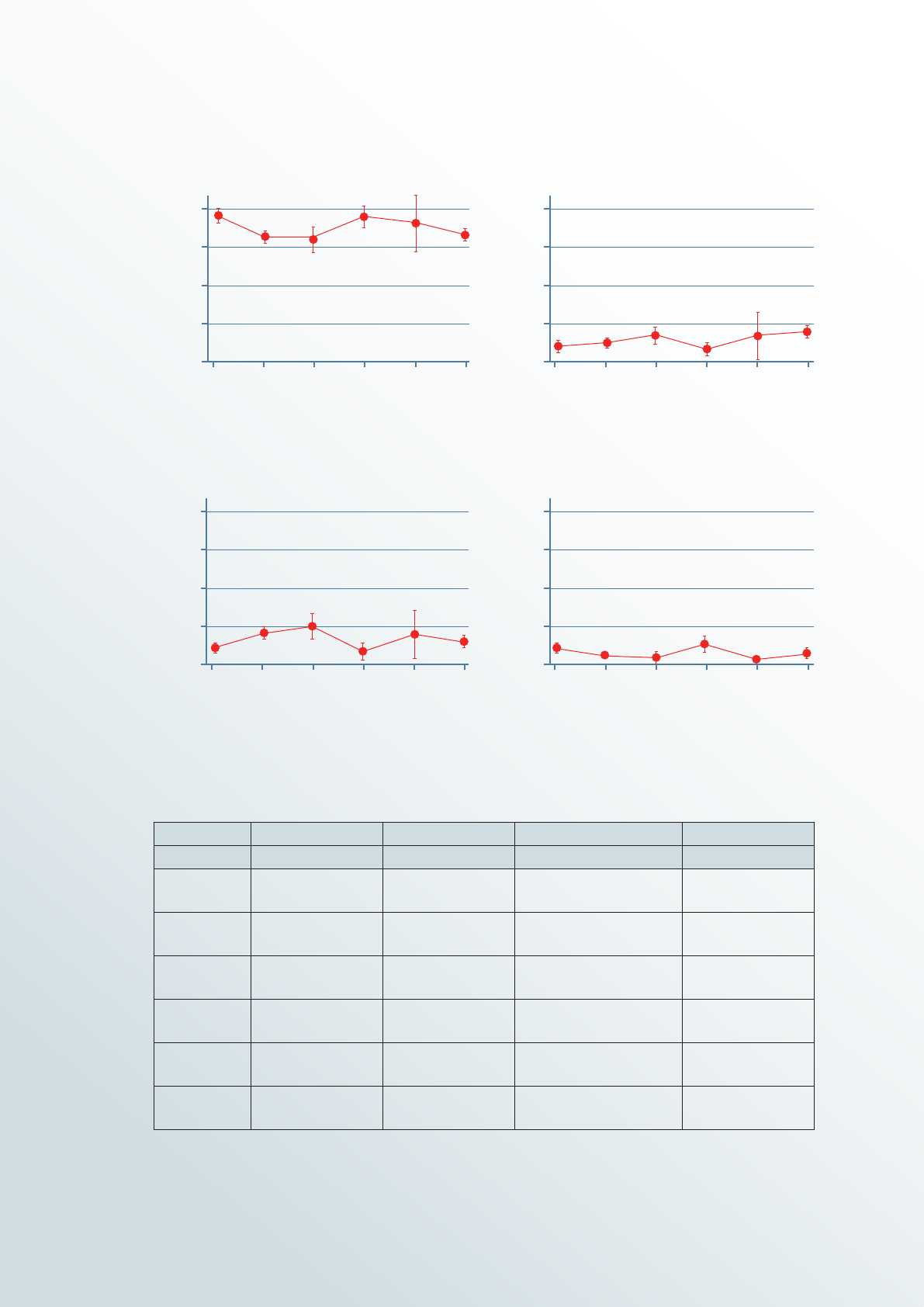
In terms of ethnicity, our data suggest the following. White participants in the programme had a
significantly higher probability of being known to be HIV positive than Black African, Black Caribbean
and Other/Mixed. Black Caribbean and Black African participants had a higher probability of being newly
diagnosed than White participants, nevertheless 95% confidence intervals were overlapping (indicating
uncertainty about the statistical significance of these probability dierences). Black African and Black
Caribbean participants were two and three times as likely to be re-engaged to HIV care as White
participants. Black African and Black Caribbean participants had a lower probability of not being able to
be contacted, however 95% confidence intervals were overlapping slightly.
Figure 4: Unadjusted predicted probabilities of outcomes by age group
15-34
15-34
15-34
15-34
35-49
35-49
35-49
35-49
Age group
Age group
Age group
Age group
50+
50+
50+
50+
Probability of being known positive by age with 95% CIS
Probability of re-engagement by age with 95% CIS
Probability of new diagnosis by age with 95% CIS
Probability of non-contact by age with 95% CIS
80
80 80
80
60
60 60
60
40
40 40
40
20
20 20
20
0
0 0
0
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
21
Table 3: Unadjusted predicted probabilities of outcomes by UKHSA ethnic categorisation.
Known positive New diagnosis Re-engagement to care Non-contactable
Pr [95% CI] Pr [95% CI] Pr [95% CI] Pr [95% CI]
White 0.77
[0.72, 0.81]
0.09
[0.06, 0.12]
0.079
[0.05, 0.11]
0.07
[0.04, 0.10]
Black African 0.67
[0.63, 0.71]
0.12
[0.10, 0.15]
0.17
[0.139, 0.199]
0.04
[0.02, 0.05]
Black
Caribbean
0.63
[0.56, 0.71]
0.13
[0.07, 0.18]
0.22
[0.15, 0.28]
0.03
[0.01, 0.05]
Black other 0.75
[0.68, 0.83]
0.07
[0.02, 0.11]
0.08
[0.04, 0.13]
0.10
[0.05, 0.15]
Asian 0.71
[0.55, 0.87]
0.13
[0.01, 0.25]
0.16
[0.03, 0.29]
9E-08
Other/Mixed 0.68
[0.64, 0.72]
0.15
[0.12, 0.19]
0.10
[0.07, 0.13]
0.06
[0.04, 0.09]
Figure 5: Unadjusted predicted probabilities of outcomes by UKHSA ethnic categorisation.
White
White
White
White
Black African
Black African
Black African
Black African
Black Caribbean
Black Caribbean
Black Caribbean
Black Caribbean
Black other
Black other
Black other
Black other
Asian
Asian
Asian
Asian
Other/mixed
Other/mixed
Other/mixed
Other/mixed
80
80 80
80
60
60 60
60
40
40 40
40
20
20 20
20
0 0
0 0
UKHSA Ethnic Category
UKHSA Ethnic Category
UKHSA Ethnic Category
UKHSA Ethnic Category
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
Probability of being known positive by ethnicity with 95% CIS
Probability of re-engagement by ethnicity with 95% CIS
Probability of new diagnosis by ethnicity with 95% CIS
Probability of non-contact by ethnicity with 95% CIS

22
Table 4: Unadjusted predicted probabilities of outcomes by London borough council.
Known positive New diagnosis Re-engagement to care Non-contactable
Pr [95% CI] Pr [95% CI] Pr [95% CI] Pr [95% CI]
Lambeth
0.79
[0.76,0.82]
0.06
[0.04, 0.08]
0.11
[0.08, 0.13]
0.04
[0.03, 0.06]
Lewisham
0.67
[0.66, 0.74]
0.12
[0.09, 0.15]
0.15
[0.12, 0.19]
0.02
[0.01, 0.04]
Southwark
0.77
[0.74, 0.80]
0.10
[0.08, 0.13]
0.07
[0.05, 0.09]
0.06
[0.04, 0.07]
Other
0.60
[0.55, 0.65]
0.16
[0.13, 0.20]
0.16
[0.12, 0.17]
0.08
[0.05, 0.11]
Lambeth Lambeth
Lambeth Lambeth
Southwark Southwark
Southwark Southwark
Lewisham Lewisham
Lewisham Lewisham
London Borough London Borough
London Borough London Borough
Other Other
Other Other
Probability of being known positive by council with 95% CIS Probability of new diagnosis by council with 95% CIS
Probability of re-engagement by council with 95% CIS Probability of non-contact by council with 95% CIS
Figure 6: Unadjusted predicted probabilities of outcomes by London borough council.
In terms of the geographical distribution of those identified as either new diagnoses or as LTFU patients,
the data suggest that participants in Lewisham and other London borough councils had a significantly
lower probability of being known to be HIV positive than SIB participants in Lambeth and Southwark.
Participants in Lambeth had a significantly lower probability of being newly diagnosed than other borough
councils, and finally, participants in Lewisham and other London borough councils had a significantly
higher probability of being re-engaged to care than SIB participants in Lambeth and Southwark.
80
80 80
80
60
60 60
60
40
40 40
40
20
20 20
20
0
0 0
0
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent
PR (Outcome == Known_Positive)
Percent

23
We also conducted multivariable multinomial logistic regression by demographic characteristics and
can state that after mutual adjustment of demographic characteristics, it was observed that the relative
risk of a female is RRR=.68 for being newly diagnosed vs. being a known positive. In other words, the
expected probability of being newly diagnosed was significantly lower for females (32%). The expected
probability of being newly diagnosed was significantly higher for those aged 15-34 compared to those
aged 35-49 years old. Black Africans were twice and Black Caribbeans almost three times as likely as
White British to be newly diagnosed. Participants in the SIB from other/mixed ethnic background were
twice as likely as White British to be newly diagnosed. Newly diagnosed patients with HIV were more
likely to be found in Lewisham (almost 3 times), Southwark (almost 2 times) and other borough council
(4 times) compared to Lambeth.
After mutual adjustment of demographic characteristics, it was observed that the expected probability
of being re-engaged was 51% higher for females compared to males. The expected probability of being
re-engaged was 44% lower for those aged 50-64 years and 77% for those aged 65 and over compared to
those aged 35-49 years. Black Africans were almost twice and Black Caribbeans more than three times
as likely as White British to be re-engaged. Participants in the Zero HIV programme were more likely to
be re-engaged in Lewisham or another borough council compared to Lambeth. The probability of being
re-engaged is not statistically dierent for Southwark and Lambeth.
After mutual adjustment of demographic characteristics, it was observed that the expected probability
of not being able to be contacted was 71% higher for females. The expected probability of not being
able to be contacted was 53% lower for those aged 35-49 compared to those aged 15-34 years. Black
Africans and Black Caribbeans had a lower probability of not being able to be contacted compared to
White British. However, these dierences were not statistically significant. This is possible due to the
small number of those who could not be contacted. Compared to Lambeth, participants in other borough
councils were more likely to not being able to be contacted. The probability of not being able to be
contacted was similar for participants in Lambeth, Southwark, and Lewisham.

24
Table 5: Multivariable multinomial logistic regression by demographic characteristics (probabilities
expressed as relative risk ratios-an RRR below 1 indicates a lower probability, above 1 indicated a higher
probability).
New Diagnosis Re-engagement to care Non-contactable
RRR [95% CI] RRR [95% CI] RRR [95% CI]
Gender
Male Ref. Ref. Ref.
Female 0.70* [0.49,0.99] 1.51* [1.10,c2.07] 1.71* [1.04,2.84]
Age
15-34 Ref. Ref. Ref.
35-49 0.44*** [0.3.0,0.67] 1.28 [0.80,2.04] 0.47* [0.24,0.93]
50+ 0.349*** [0.23,0.52] 0.67 [0.41,1.07] 0.63 [0.34,1.17]
Ethnicity
White Ref. Ref. Ref.
Black African 1.98** [1.21,3.25] 1.872* [1.152,3.042] 0.532 [0.270,1.050]
Black Caribbean 2.60** [1.37,4.94] 3.295*** [1.843,5.888] 0.359 [0.102,1.264]
Black other 0.90 [0.41,2.02] 0.858 [0.403,1.829] 1.339 [0.619,2.895]
Asian 1.47 [0.46,4.74] 1.494 [0.502,4.445] 0.000 [0.000,0.000]
Other/Mixed 1.97** [1.21,3.2.0] 1.245 [0.744,2.084] 0.897 [0.472,1.702]
Council
Lambeth Ref. Ref. Ref.
Lewisham 2.70*** [1.67,4.36] 1.94** [1.29,2.92] 0.47 [0.22,1.02]
Southwark 1.85* [1.13,3.02] 0.84 [0.53,1.33] 1.04 [0.57,1.91]
Other 4.13*** [2.53,6.77] 2.82*** [1.81,4.37] 1.89* [1.01,3.51]
There are limitations to these data that must be considered. Firstly, the small sample size of those
re-engaged to care and those who decided not-to re-engage does not allow a detailed exploration
of any ethnic, sex and age dierences in the odds of being re-engaged into HIV care by HIV clinics
and GP practices. Secondly, the small number of counts (sample size) does not allow to explore how
the demographics of people disconnected from care & reached through HIV clinic or primary care
audit/recall interventions dier from those found through ED testing or another route. Finally, most
participants lived in more socio-economically deprived neighbourhoods, therefore there was limited
statistical power to explore inequalities in HIV care in SIB at the intersection of socio-economic
disadvantage and demographic characteristics.

25
Evaluating the processes through which
the Zero HIV programme functioned
The qualitative findings of the service evaluation are structured as follows.
› Firstly, we provide a narrative overview of the programme and combine headline descriptive
statistics with a synthesis of key qualitative data.
› Secondly, we define the distinct elements of the Zero HIV ‘intervention’ and reflect on the ways in
which dierent actors define these.
› Thirdly, we explore the dierent intervention elements across their separate healthcare settings in
three subsections – secondary care (hospitals), primary care (GP practices), and the community.
› Fourthly, we present the views of participants in relation to the sustainability of these HIV service
interventions beyond the period of SIB-financing.
Narrative overview
The headline finding from this service evaluation is that the 3-year Zero HIV SIB programme has been
eective in both (1) delivering improved health outcomes for people living with HIV and (2) improving
inter-organisational collaboration and service collaboration across what has historically been a rather
fragmented HIV healthcare ecosystem in South London.
In terms of the health impacts, key actors expressed confidence that this programme had reached (i)
people living with HIV who were previously undiagnosed and brought them into contact with specialist
NHS services and (ii) people living with HIV who were previously diagnosed but had become ‘lost to
follow-up’ (LTFU) treatment services. However, the absence of robust baseline data for key outcomes
or a commitment to a counterfactual evaluation design means it is not possible to attribute outcomes to
specific interventions.
In terms of the organisational impacts, key actors expressed confidence that this programme
successfully mitigated many of the traditional organisational and financial factors that had led
to fragmented HIV services in South London through (i) improved inter-organisational network
working – both formal and informal in nature through boundary spanning activities and a pervading
‘cosmopolitanism’ (Greenhalgh et al, 2004; Damschroder et al, 2009). In addition to this, informants
perceived the increased use of data and monitoring and the realignment of incentives as positively
promoting collaboration and better outcomes. In terms of financing (ii) the programme very eectively
negated many aspects of the existing siloed payments systems for various aspects of HIV services which
actors felt had stymied attempts for providers to implement evidence-informed practice (for instance
in relation to ED and Primary Care testing), or to adapt to practical realities (such as identifying LTFU
patients and providing more flexibility for not-for-profit provider organisation outreach work).

26
The programme adapted and grew over the three years with new provider organisations recruited
over the lifetime of the programme and new emphases on delivery developed – for example through
the expanded use of GP champions. This adaptability proved to be very beneficial in relation to the
COVID-19 outbreak in early 2020 (see Stanworth, 2022) and presaged a pivot to greater LTFU work.
Community providers welcomed the flexibility that the programme aorded them overall, though issues
were noted by some providers in relation to how SIB-financed work may have been seen to duplicate
existing work commissioned more conventionally. This ‘messiness’ of competing contracts, and
perceptions of ‘double-dipping’ was problematic and caused extra labour for some actors and reflects
the complexity of the existing commissioning landscape with resultant conflicts, and the overall lack of
coordination between NHS and not-for-profit service provisions.
The role of EJAF was praised by informants. The organisation played a key boundary spanning function
and delivered leadership, support, and encouragement to other organisations. EJAF were crucial
players in the design, financing, and delivery of the programme acting as co-commissioners, financial
intermediaries, project managers, and data analysts. EJAF successfully disrupted many of the existing
inter-organisational, financial, and institutional barriers that historically inhibited more systematic
implementation of testing, LTFU and better joined-up HIV service provision. EJAF were instrumental
in shaping an ‘outer context’ conducive to improving HIV services in South London. Namely, EJAF
facilitated the establishment of systematic processes that helped enable other organisations and
individuals to focus on identifying and caring for people living with HIV – free from some of the
organisational and financial impediments that had hindered such work previously.
Rather than one ‘intervention’ the qualitative data highlighted that the actors involved in commissioning
and delivering HIV services through the Zero HIV SIB programme felt they were delivering a suite of
‘interventions’. Some of these have a strong existing evidence base and have been recommended in
existing guidelines whilst others are more organisational and pragmatic. Some were new and developed
as part of the Zero HIV SIB programme whilst others were already in existence in some or other settings.
A key finding was increased flexibility and local discretion to use funds to tailor services more closely to

27
the needs of those using services as we have seen in other health focused SIBs in the UK (Fraser et al,
2018).
A key aim of the programme was to further the evidence for these interventions and change practice
going forward. A criticism of the programme raised by some informants was that more work could have
been done to ‘baseline’ existing practice and prove the attribution of some of these interventions in
order to provide a more robust body of evidence to sustain these going forward once the SIB financing
ended in December 2021. Though beyond the scope of this current service evaluation, it appears that
learning from the programme (particularly in relation to ED testing) may have been used to inform
national and local level policymakers in future HIV policy development.
There are mixed views from informants in relation to the sustainability of the improvements to South
London HIV services delivered through the Zero HIV SIB programme after the SIB-financing is gone. The
regional commissioning ecosystem is undergoing a further reconfiguration as the new Integrated Care
System is developed. More research is needed to follow these developments over the coming years.
One interesting question that divided informants to a degree related to the extent and nature of public
versus third sector financing and delivery of HIV services in the future.
Defining the Zero HIV SIB-financed ‘intervention’
Figure 2 presents a useful graphic representation of the dierent interventions which occurred in
dierent settings and locations as delivered by various NHS and non-NHS provider organisations.
Figure 2: Overview graphic of Zero HIV SIB programme interventions (taken from Stanworth, 2022)
Secondary Care
(Hospitals)
Primary Care Community
• Oer ‘opt-out’ tesing and support to those who access services
• Identify those LTFU when they access services
• Proactively contact those identified LTFU by data analysis
• User HIV experts and champions to support and educate
colleagues in how to engage patients
• Oer testing and support in a
variety of community settings
• Target those most vulnerable
and least likely to seek
treatment
Hospital Trusts GP Foundations VCSEs
Accident and emergency
departments
Other surgical wards
GP surgeries
Hospitality venues
Saunas and gyms
Barbers
Places of worship
Healthcare setting
Interventions
Providers
Locations
In the qualitative interviews we asked participants to define and explain the Zero HIV programme in
their own words – whether as a health ‘intervention’ or something else. Most informants emphasised the
multi-modal and multi-locational nature of ‘intervention’:

28
‘There are dierent programmes running in dierent services, so you’ve got the community
organisations, you’ve got things running in Primary Care through the GPs and then through
Secondary Care in hospitals and HIV clinics. So, for example we have the HIV testing
on new patient registration in GP surgeries for example, or testing patients for HIV who
have never had an HIV test as they’re going for other routine bloods, we’ve got community
organisations who are actively going out and doing point of care testing at events or
amongst particularly aected ethnic groups… And then in the hospitals, we’ve got the
introduction of the routine opt out testing, HIV testing in the A&E department, so anyone
who visits and hasn’t ever had an HIV test or not had one in the last twelve months will
have that test added onto their bloods. And then we’ve got the HIV clinics who are setting
up more robust pathways for patient recall and auditing their clinics to nd out who’s not
been seen in the last twelve months and bringing people back into care.’
Hospital nurse 1
This informant went on to highlight the way that the programme combines an experimental element –
i.e., building an evidence base around local eectiveness with a commitment to following established
guidelines:
‘It’s experimental but it’s also, you know, what we’re doing is based on best practice…
that’s outlined by NICE and BHIVA, but the resources have not been sucient for it to
happen. So, I suppose it’s not routine, it hasn’t been routine in the past for HIV testing to
be done in the A&E Departments, but it is clear in NICE guidance that it should be done
in areas of high incidence, which our hospital is in an area of very high incidence of HIV.
And that’s not happening [outside of this programme]. And I think the main reason, well,
in my limited understanding, the main reason it’s not being done is because there’s other
priorities and because there’s not the funding, it’s not been prioritised as a funding, or it’s
not been a priority funding need… there must be a lot of things that are in guidelines and
best practice documents that we all know that’s what we should be doing but actually it’s
not achievable within the budget that we are aorded.’
Hospital nurse 1
For many informants, the programme functioned as a way to encourage greater and more consistent
uptake of existing evidence-informed practices by removing traditional barriers linked to funding,
stang, or competing clinical or organisational priorities. The commissioning manager below
emphasises the ways in which the programme goes beyond initial testing and LTFU work to encompass
greater support post-diagnosis to encourage all patients to enter (or re-enter) NHS care.
‘At its core, it’s HIV testing, and then communication with people who are, identication
and communication with people who have dropped out of care. So, HIV testing, but also,
I guess, what’s slightly dierent with some of the more transactional HIV testing stu
we fund is that, obviously, the outcome paid for is HIV identied and the person enters
care, so people have to take them all the way on that journey. Now, of course, that’s not
the only intervention under the SIB, in the sense that it’s funded more developmental
stu, GP champions, etc., but generally, that’s been about building networks and clinical
infrastructure to support testing across our local, well, what I would say our ICS [Integrated
Care System], but really, it’s Lambeth, Southwark and Lewisham.

29
We haven’t expanded it out to Southeast London yet, but [this is an aim]’
NHS/LA service commissioner
Alongside this greater support for people living with HIV, the programme functions at a regional level
to foster the development of increased clinical skills and networked working alongside deeper inter-
organisational collaboration.
For some of those involved these dierent interventions were new – but not for others:
‘Was there anything novel? So, whilst some of this work had been done in some settings
and wasn’t novel at all, had been doing it for some time, any time you brought it to a new
setting it was novel. So, if you were a GP practice that you’ve never done HIV testing
for any of your patients, it’s novel… And again, in the A&E departments where it was
embedded and it wasn’t particularly novel, but telling another A&E department, who
are at out and not meeting their four-hour waits and falling over and got NHS[England]
breathing down their necks, it’s not only novel, it’s almost beyond comprehension that
you’re now asking them to do something else, which they quite oen don’t perceive to be a
high priority.’
Commissioner 4
This informant captures the complexity and variability of the pre-existing situation and how the
programme sought to encourage greater standardisation across the boroughs involved. Interestingly,
the evaluator of the programme – with extensive experience of other SIBs -noted the uniqueness of this
programme compared with other SIBs in relation to the variation in numbers, types and settings in which
‘interventions’ take place.
In summary, informants positively emphasised the multi-dimensional nature of the programme and how
it encouraged a more standardised uptake of various complementary activities that sought to identify
new and existing people living with HIV through clinical and organisational interventions and practices
across a variety of healthcare and community settings. The programme identified existing obstacles
to the implementation and normalisation of evidence-informed practices and proposed solutions to
overcome these in a more systematic way.

30
Secondary Care
We collected data from NHS sta working predominantly in two dierent Southeast London hospital
settings. In this report we mostly aggregate the findings from both settings. In further academic work
we plan to explore the dierences across these two ‘inner settings’ (Damschroder et al, 2009) in more
detail. Hospital sta emphasised two distinct activities or interventions at the secondary care level. The
first of these is ‘opt-out HIV testing’ which took place predominantly in the Emergency Department (ED)
of each hospital with a view to diagnosing new HIV cases. The second is the identification and active
tracing and communication with people with a known existing HIV diagnosis who had disengaged from
NHS HIV clinical services – or colloquially - ‘lost to follow-up’ (LTFU). In practice, there was a good degree
of cross-over between these two activities, notwithstanding this, we explore them separately below.
Opt-out HIV testing in the ED
The Zero HIV programme set out to institute and regularise HIV testing for all patients who required
blood tests on presentation at the ED department in participating hospitals. This initiative was in line
with existing (British HIV Association) BHIVA and NICE guidance. However, prior to the Zero HIV
programme, it had been hard to implement this locally for a number of reasons including (1) financing
(2) sta reluctance and (3) competing organisational priorities.
Financing ED opt-out HIV testing has long been problematic, falling between the cracks of the three
potential funders – Local Authorities (LA), Clinical Commissioning Groups (CCG) and NHS England
(NHSE)– as articulated by a hospital manager:
‘That’s why, historically, when we’ve done what’s called our provider intentions, when we
set out service developments, we’ve always put that we would like ED tests, HIV testing in
ED, to be funded. And Local Authorities have always pushed back because, within their
commissioning arm, what’s been delegated to them from the government is not anything
to do with preventative sexual health. So, they’re not responsible for that funding element,
whereas our CCG commissioners, they’re also not technically funded for any preventative
care for HIV, which involves testing. You’re only tested, for example, if you came into the
hospital, maybe you were in critical care, and they’ve eliminated, maybe, majority of all
the other tests that could be contributing to your illness, they’ll be like, we should test you
for HIV, we’re going to ask you, have you ever had an HIV test? So, it was then in those
instances that a certain number of patients would then be tested. But within our contract
with CCG commissioners or NHS England commissioners, there is no, sort of, requirement
for them to fund for testing for HIV, either in ED or just as routine. So, NHS England fund
our HIV treatment as part of their specialised services arm, so they would actually fund
treatment once you’ve been diagnosed with HIV [but not testing in the rst place].’
NHS manager 1

31
SIB-financing as part of the Zero HIV programme solved this historical problem by explicitly stepping
in and funding HIV opt-out testing in the ED. The funding model that was negotiated between EJAF for
one of the NHS trusts was structured in such a way that it guaranteed a minimum funding level so that
the hospital would not be out of pocket regardless of the ‘success’ of the new testing regime, and also
incentivised them to reach as many people living with HIV as possible. In this way it removed the barrier
of financing which had prevented opt-out testing in ED to take place hitherto. This might be seen as a
SIB-related flexibility mechanism.
The desire to increase testing was there from HIV specialist sta already – but the EJAF funding enabled
them to move from ‘one-os’ to a more regularised model:
‘So as soon as I came here, I started to try and get HIV testing a little bit improved in
other departments. And ED was the obvious one. But hit a lot of brick walls in terms of
nancing. So, I did manage to persuade people to let me do things on World Aids Day and
HIV testing week, and things like that. And they were just one os. And actually, even
back then, still dealing with quite a bit of prejudice and stigma amongst the sta. A lot of
misconceptions that it would take an awful lot of time, and a lot of concerns about consent
process of testing someone for HIV... And so, a lot of education around various dierent
departments and sta and trying to feedback when there were late diagnoses – not always
being greeted with great response to that. And then just felt like I was coming up against
a brick wall the entire time in terms of funding, so when EJAF came along, it was just
brilliant. And to be honest, we just started very, very promptly because we’d already done
all of that kind of groundwork, and actually the main issue was cost.’
HIV Consultant 1
The theme of sta reluctance to engage and HIV stigma in the quote above was a recurring one noted by
HIV champions – replicated by a nurse below:
‘Throughout my nursing career I’ve always had an interest in HIV. So, where I trained…
it’s a very taboo subject... So, we had a patient in ED at [another London hospital] that
had come in aer a chemsex party, really unwell, and it was just the nurse’s attitude. I
overheard them talking about HIV and it was just the nurse’s attitude, and I was like
“Actually we need to change this”. So, this is why I am now quite passionate about it. So,
my involvement in the ED down in [this hospital] was actually I liaised with, so my link
role as an emergency nurse practitioner was sexual health, so I was liaising with the [HIV]
Clinic and bits and pieces, trying to push it. And from my own experiences, good health
promotion experience as well. The one thing I was quite keen about is actually we need to
get people talking about it and making it an everyday norm and I think that’s why I like it
because actually it’s, the management of HIV has come such a long way and we now treat
it as a, what I would call a chronic condition because of medication, so actually let’s get it
out into the forefront and talk about it and make it an everyday conversation, not a taboo
conversation.’
Hospital nurse 2

32
A strong and consistent finding was the level of personal and professional dedication that the vast
majority of informants had towards people living with HIV and career-long desire to improve HIV services
– however, these commitments from HIV champions were sometimes not taken-up by non-HIV specialist
clinical sta. This is important because the majority of work actually done to deliver opt-out testing was
not carried out by HIV specialist clinicians – but ED nurses. Therefore, a significant implementation
challenge revolved around changing the perceptions, attitudes and working practices of ED nursing sta.
This involved changing the culture and dialogue from asking ‘do you want an HIV test’ to ‘this is an area
of HIV incidence. We test everyone unless you ask us not to’.
Non-specialist HIV nursing sta reported how in the years prior to the Zero HIV programme, opt-out
testing in ED had not been the norm – indeed HIV testing in ED was rare and only tended to occur when
ordered by doctors if clinically relevant. With the introduction of the Zero HIV programme, a programme
of awareness raising had taken place:
‘During handover [Band 7 nurses] will just tell us “OK we’re doing the HIV testing for
all patients. You just have to tell [the patients], ask for permission and that’s it. If they
don’t want, then just not do it” – something like that. It was very quick, really simple. To
be honest not a lot of us were complying to it at the very rst I think weeks, or probably
months, and even now some of us do not do it.’
Hospital nurse 3
The new opt-out testing initiative adds further complexity to the interactions that nurses must have with
patients thereby increasing the time it takes to triage patients. It also emerged that some spaces are
more conducive to these conversations than others:
‘It’s also a very dicult conversation, and they have brought this up, because it’s OK if it’s
triage because you are in a room, in a private room and it’s you and the patient. But it’s
quite dierent say for instance if you were in Majors. When we get a lot of patients, and we

33
don’t have enough cubicles we let them sit on the grey chairs and sometimes they sit beside
each other, and those conversations are quite dicult to ask them if they want HIV testing
when other patients or relatives of patients can hear you. So, I brought this to the matron’s
attention that it’s hard to get the patient’s consent, because in my opinion the consent for
HIV screening needs to be private.’
Hospital nurse 3
It is apparent that ED opt-out HIV testing can be challenging in the inner setting of hospital EDs. In
another hospital involved in the Zero HIV programme, the approach taken was dierent, in that notional
consent for testing was assumed – and this was achieved through extensive publicity about HIV testing
– for instance through leaflets and posters.
The key factors in mitigating these challenges were HIV specialist sta linking into and liaising with ED
sta – in particular the Clinical Nurse Specialist (CNS) role seems crucial:
‘I think there was some resistance from some of the sta in A&E about the testing, but we
learned to work with the people who were really on-board with it and kind of used them as
our channel, but the important thing for me was to try and build a relationship between the
clinic and the sta there, so yeah, I would go to A&E handovers. I did try and go to some
of the doctors’ handovers, which I did a little bit, just at the beginning you really want to
get it into people’s minds. I went to a number of the sta training days for A&E for the sta
nurses and the HCAs, I went and did sessions with the new rotating doctors as well’
Hospital nurse 1
The CNS role is significant in terms of boundary spanning from the HIV-specialist setting to the ED.
Numerous informants spoke of the significance of the regular presence of the CNS during shift handover
and also the feedback in relation to patient outcomes that the CNS provided. This is important as a way
of expanding support for the intervention through highlighting the significance of the intervention and
the value it has for patients and improving care:
‘Eventually I got onto the ED Friday news, so I would start – I would particularly go back
and share case studies – so when we had our rst new diagnosis it couldn’t have been
a better patient case study because it blew people’s minds, that an 85 year old was the
rst lady that was tested… that was so helpful because suddenly people started to go ‘oh
right, OK, this is bigger than the gay community and our drug users’ and, you know, it
really helped, so sharing those case studies, as I went I’d say ‘right we’ve had four new
diagnoses this month’ and share some of the stories and that really helped people to see the
importance of the testing.’
Hospital nurse 1

34
Having the CNS in place and able to aid the opt-out ED HIV testing intervention with support from
HIV specialist colleagues highlights the organisational prioritisation of HIV services linked to the
Zero HIV programme – such prioritisation had previously been lacking. The CNS role was partially
funded by outcomes from the Zero HIV programme. In addition to the clinical champion activities, the
CNS also plays a substantial role in data collection and presentation related to ED diagnoses and has
a clear understanding of the links between new diagnoses and outcomes payments, reiterating the
significance of how the wider financing model/outer context/incentives de-risks the hospital to
innovate the stang model.
In summary, implementing opt-out HIV testing in ED was a complex undertaking. The key sta members
implementing the intervention are not HIV specialists and may display resistance to the intervention
for understandable reasons given their wider work commitments and time pressures – especially in the
early days of implementation. The stigma around HIV complicates the discussions that ED nurses have
with patients and the physical spaces in which these discussions must take place are suboptimal in
many ways. The dierent models in relation to consenting patients found in the dierent sites are worthy
of greater examination in further research.
Notwithstanding these implementation issues, the overall picture is one in which ED opt-out HIV testing
is better established than before the Zero HIV programme in the hospitals in which we conducted
our research and has generated new HIV diagnoses which would have been less likely without
the intervention. Key factors in driving this change are a clear and reliable funding stream for the
intervention and dedicated HIV specialist sta support – from the CNS working in a boundary spanning
role, encouraging ED sta to implement the intervention, and feeding back results, generally raising
awareness, and acting as a clinical champion with other HIV specialist colleagues.
These positive changes are attributed by informants to the Zero HIV programme.

35
LTFU work in the hospital setting
The second significant intervention in the secondary care setting is LTFU work. This work involves
hospital HIV Clinic sta systematically reviewing databases of known HIV patients and reaching out
to those who have stopped attending NHS care, talking to them, and encouraging them to re-engage
with HIV services. The work is dicult as contact details may be out of date and some patients may
reject the outreach attempts. Often these individuals may live in deprived or marginalised settings and
may have profound mistrust of public and wider institutions, be fearful due to their immigration status,
or be concerned that anyone in their community may learn of their HIV status. LTFU work is therefore
time consuming, administratively burdensome, and potentially emotionally challenging. It requires
administrative, clinical, and social skills alongside patience and persistence.
There are many parallels with the opt-out ED HIV testing in terms of the barriers to achieving LTFU
success and the facilitators which the Zero HIV programme put in place. Like the opt-out testing
intervention, there was (1) some confusion and complexity in relation to which commissioning body
ought to finance LTFU work and (2) a lack of organisational prioritisation in terms of doing the LTFU
work. Unlike opt-out testing, sta resistance and HIV stigma are themes that do not emerge as barriers
in relation to LTFU as the team consist of HIV specialists. Neither is there an established evidence base
proving the benefit of LTFU work (in contrast to opt-out ED testing) – it is more of a practice-based
intervention, dependent on relationship-building with often vulnerable populations, and time-consuming
data cleaning activities and analyses. Finally, the boundary spanning role of the CNS emerges as
a significant factor, as does the payment mechanism and somewhat unexpectedly, the COVID-19
pandemic is seen by some informants as something of a facilitator in the successful development of
hospital led LTFU strategies.
The quote below from one of the HIV consultants captures key elements of the story around the existing
barriers and eventual facilitators rather neatly:
‘A lot of [the LTFU] work I’ve always done… because it was quite important. But we were
just overwhelmed by the work that we’ve [already] got, and, even doing the kind of here
and now and things that come to you – so sort of seeking out that extra work is something
that you don’t have as much time for. And I think that was supposed to be mainly
something that community nurses did, but they’re not the people who are best t to do that.
It has to be from the hospital, who decide, who are much more aware of who’s to follow
up and who isn’t. And they’re also completely overwhelmed looking aer all these really
complex patients in acuity. So, it’s been brilliant when EJAF said that they were interested
in the [LTFU work] as well, and once we got the ED testing up and running, and it was not
requiring as much of [the CNS] time anymore – she’s now devoted herself to that, because
there’s quite a backlog. So, the whole idea is that can shi the backlog and then have much
more better ongoing things to re-engage people much earlier in the piece. And she’s done
brilliantly. Really, really brilliantly. It’s not always success stories, we don’t always get hold
of people, but if we do get hold of people, they don’t always want to take treatment, but for
those people who’ve got plans in place – so I feel much more comfortable about it all. And
it has made a huge dierence, having her designated role to do it.’
Hospital Consultant 1
36
Before this work was specifically identified and financed by the Zero HIV programme it suered from a
lack of ‘ownership’. Community nurses received some funding to pursue patients who were LTFU, but
some informants questioned whether these were the best placed actors to do so. At the same time,
clinical sta from the hospital engaged in ad hoc LTFU work but were not able to focus systematically
on this work due to other work commitments. A further key issue expressed by informants related to
problems with the data – i.e., missing data, or poorly categorised data, and that no one ever had the
time to fix such problems. As part of the Zero HIV programme, responsibility for the LTFU work (of
hospital patients) was directed to the CNS, who, in conjunction with other HIV specialist sta was tasked
with tracking down LTFU patients and bringing them back into NHS care.
The outcomes payment approach delivers a significant fee for each new or LTFU patient linked to HIV
care and registered by the hospital in a way that is completely dierent to before. This means that time
spent on LTFU work can become generative as opposed to consumptive in financial terms – in complete
contrast to prior practice. A number of informants also pointed out that this was work which could take
place throughout the periods of lockdowns in response to the COVID-19 pandemic (Stanworth, 2022)
which was highly beneficial for all parties. Once more this highlights the flexibility and adaptability of the
Zero HIV programme.
In summary, the LTFU strand of the Zero HIV programme developed over time to become highly
significant and eective in re-engaging HIV patients. The programme increased the organisational
importance of this work through mandating the practice within the work-role of relevant and capable
hospital sta and incentivising HIV teams to do this work through the outcomes-based financial model. It
was particularly useful and durable during periods of COVID-19 ‘lockdown’.

37
SECONDARY CARE PATIENT EXPERIENCE
BENNIE’S STORY
Bennie has lived in London for many years. A couple of years ago, he was not feeling well – so he
went to his local ED. One of the ED doctors organised for him to have an HIV test in the ED, despite
him having very few HIV risk factors: ‘[The doctor] asked me, have I ever been tested for STDs or
HIV, and I said, no, and they said, did you mind, I said, I don’t, because obviously, I didn’t think
anything of it.’
He was admitted to hospital from the ED and thought nothing more of the HIV test. Two days after
his admission, he was visited on the ward by the HIV team: ‘So, they came in and they said that I
tested positive, and obviously, they gave me all the support and stu.’
Bennie spoke very highly of the support he received from the HIV clinical sta, describing them
as: ‘Very, very supportive. [the nurse] held my hand, and it was, I mean… we are kind of friends
when I go [to the clinic] for my blood test. It’s like family… they told me everything, they explained
everything. I mean, I cannot thank them enough… every time you go [to the clinic] it’s just like, they
don’t look at you like you’ve got disease; they look at you like you just come in and say, hello, good
morning, how are you? The nurses know, and even when they take the blood test, everyone is so
friendly, you just do want to go there, literally’
Bennie is fully supportive of opt-out testing in ED: ‘I think they should do it [test for HIV]
automatically, that should be just a normal, standard thing, because like I said to you, I don’t know
when and how… I mean, I think I know how, but I still, I’m not 100% sure, and if they didn’t do that,
then I was still living and probably been much more ill than I am now, so there should be standard
tests like they shouldn’t ask, they should just do it.’
Bennie had heard of EJAF and had an understanding that they were involved in some way but felt
that the service functioned as a standard NHS one. He was keen that the service continue beyond
2021 and that the NHS fund the service.
He was keen to pass on the following message about education for schoolchildren and for HIV
testing to be increased and normalised for everyone: ‘I think that [schools] should have someone
to actually come in to talk to them about HIV, how you catch it or how not to catch it, just to make
them aware… To avoid it and to help them understand that if you do get it, it’s not the end of the
world, but it’s better for them not to get it.’

38
Primary Care
We collected data from GPs acting as ‘Champions’ for the programme working in three dierent GP
practices in two Southeast London boroughs. Primary Care is dierent from Secondary Care in that
services are less coordinated, meaning that there was quite a bit of variation in the activities that made-
up the intervention. Nevertheless, the intervention at the Primary Care level can be broadly grouped into
three main activities: awareness raising with GPs; opt-in HIV testing; and LTFU work. In this section we
compile the findings from across these dierent settings integrating some discussion on variations and
will explore the dierences between them in more depth through further academic work.
Awareness Raising
Across the interviews the GP Champions discussed how many in Primary Care hold the view that HIV
prevention and care ‘wasn’t something that GPs did’ (GP2), and that HIV is currently not a ‘priority’
in Primary Care, for instance when compared to diabetes, asthma, and COPD. Therefore, the HIV
Champions described an important aspect of their work in terms of ‘trying to encourage GPs to be more
mindful of HIV patients… [and more generally be] a bit more aware of HIV’ (GP1). All interviewees
described the SIB and formation of the HIV Champion role, as crucial for developing HIV prevention and
support in Primary Care, in that the greater autonomy of individual GP practices calls for a more tailored
approach, and therefore also holds space for experimentation. As one HIV Champion describes:
‘[through the SIB] people are almost being paid to think about it [i.e., practice procedures
related to HIV care] … [in GP practices] thinking time is not really valued… if you’re not

39
doing something, signing a prescription or looking at a blood test result every second of the
day or talking to a patient then you’re wasting your time’
GP2.
Examples of innovative thinking towards raising awareness of HIV in Primary Care include the organising
of educational events for GPs, nurses, and GP trainees, that in one borough also included networking
with secondary care HIV specialists, as well as stigma reduction trainings for administrative sta
(identified as an issue by third sector organisations that the HIV Champion spoke to). In one borough,
they have also trialled using the outcomes-based financing of the SIB as a ‘financial carrot’ for
encouraging GPs to engage with the programme, with certain monies from the outcome payments being
sent directly to the individual practice. Competition between practices was also used as an incentive:
‘We had a dashboard, and we would send out this monthly newsletter with the dashboard
attached so that we could compare with other practices but also compare to previous
months and see whether we were up or down… and actually that was really interesting
because people would be like, “your practice is doing well” and that generalised peer
pressure was quite helpful’
GP3.
One interviewee identified the cross-borough HIV Champion monthly meetings (facilitated by EJAF) as
an important space for developing ideas and sharing learnings, and suggested, if anything, that more
time for experimentation and evaluation would have been useful. This innovative thinking can also be
seen in the other two intervention activities.
Opt-in HIV testing in Primary Care
Owing to issues of consent, opt-out HIV testing was found to not be possible in Primary Care settings.
Therefore, eorts were put towards increasing opt-in HIV testing. One approach developed by a GP, and
which was shared and taken-up by practices in other boroughs, was to alert GPs through the electronic
records system that they use, when an attending patient has never been tested for HIV or has not been
tested in the last year. The awareness raising activities (described in the previous section) included
promoting information about these alerts along with skills-building exercises with Primary Care sta on
how to initiate conversations about HIV testing. In one borough, three GP practices trialled sending out a
text message to patients asking if they would like an HIV test, however this ultimately was not considered
a success in that HIV testing did not really increase and because the people who responded were already
quite ‘health aware’. Nevertheless, this was described as an important learning opportunity in that
opportunistic testing with GPs initiating the conversation was concluded to work best in Primary Care.

40
LTFU and HIV Support in Primary Care
As with Secondary Care, lost-to-follow-up work largely involved the time-consuming work of auditing
records and trying to make contact with patients, often from vulnerable groups, who do not always have
consistent phone numbers and addresses. One identified challenge in relation to the SIB, was that it
was not always clear who the payment for LTFU outcomes should go to (i.e., Secondary Care or Primary
Care). In one borough, where relationships were strong with Secondary Care, they described negotiating
this on a case-by-case basis, however this was described as being much more challenging and political
when working relationships with Secondary Care were less strong.
Dierent from Secondary Care, all of the HIV GP Champions identified these LTFU-related activities
(i.e., auditing and contacting patients) as also crucial for ensuring that all patients living with HIV are
receiving the care that they need. As described by one interviewee:
‘I’ve been quite surprised about how … [GP] practices manage HIV…[they] make a new
diagnosis and then... say “Oh well you know you just self-refer to the local clinic?” No
follow-up, no sort of “This is a major life changing diagnosis, how do you feel about that?”
No doctor contacts them’
GP2.
Another GP described this work as being about ensuring that HIV is treated as a chronic disease, and
that it is normalised in Primary Care, but that this change in culture will likely be enormously dicult to
achieve.
The Zero HIV programme work in Primary Care has therefore supported the further development of
integrating HIV prevention and care into GP practise. This has included the building and strengthening of
relationships with HIV services in Secondary Care, along with relationship-building across GP practices,
federations, and boroughs aimed at mobilising GP engagement in, and commitment to HIV prevention
and care. As indicated by the HIV GP Champions, this area of work remains a challenge in Primary Care,
and questions around sustainability are particularly pertinent in regard to the potential loss of financing
for the HIV GP Champion role.

41
PRIMARY CARE PATIENT EXPERIENCE
SUZIE’S STORY
Suzie returned to London having lived away from the capital for a few years and registered as a
new patient at her new local GP surgery. At the end of her new patient check-up the nurse asked
Suzie if she’d take an HIV test: ‘as I was just leaving the surgery [the nurse], really nicely, asked
me would I be prepared to take an HIV test and I thought, well, yeah why not. Now had I been in a
hurry that day, I wouldn’t have taken that test, it would have been one of those things where I would
have said ‘look, do you know what, next time I’m coming in I’ll have that’, but you know that day
never happens does it…’
Suzie had very few HIV risk factors, but, very unexpectedly, the test came back positive. Suzie was
referred to her local hospital to see the HIV specialist team the following week. That week spent
waiting for the appointment was hard. However, once she met the specialist team, led by the local
consultant she felt in safe hands: ‘I’ve got a lot of faith in [the HIV consultant] because you know
when you meet someone and you kind of click and you know that they’re going to go above and
beyond and she’s very much like that.’
Suzie’s HIV was diagnosed before she developed any symptoms. She was put on to treatment and
is able to live a fully functioning life. She is an advocate for Primary Care opt-out HIV testing: ‘you
can’t force people to have it, but if anyone said to me ‘what would you advise me to do’, my advice
will be always to have the test, because in the extremely unlikely event – and it is extremely unlikely
– then you will get treated. So, I can’t see a negative in it at all.’
Suzie suggested a good analogy for the inclusion of HIV testing in new patient appointments might
be the following: ‘it’s like checking a car, taking it in for a service and not checking the brakes isn’t
it, you know, we’re going to check everything but we’re not going to check the brakes. It’s got to be
done, hasn’t it?’
Suzie was not aware of how the service was funded – or the involvement of EJAF or the nature of
the SIB – for her, the experience was one in which the NHS provided an excellent, well integrated
care pathway: ‘A really, really good NHS [service], you know, when the NHS is at its best kind of thing.’
Finally, Suzie stressed: ‘one thing that I think could be changed and there should be more public
awareness of taking this test and put over in such a way ‘look, this is not something you should be
scared of, this is something that you might need’… [furthermore] It will save the government money
in the long run, if they can get everybody on treatment, the cost of HIV treatment will come down’.

42
Community Care
Since the 1980s London has been served by a number of third sector provider organisations that have
been delivering out-reach and wider support services to people living with HIV, or communities of people
with a raised risk of contracting HIV including HIV testing services in non-clinical settings. Dierent
organisations have historically targeted specific population groups such as men who have sex with men
(MSM), immigrant communities from global areas of high HIV prevalence, and others. These community
providers are very important because they are able to reach people living with HIV who may be wary
about engaging with NHS services – for reasons of HIV stigma as well as fears about eligibility for care
due to immigration status, or not realising that HIV care is free. Like NHS HIV specialist sta, those
working for these community provider organisations demonstrate commendable dedication to serving
the needs of people living with HIV.
Historically, these services have been financed in a number of ways – with funds coming from a mixture
of philanthropic, private, and (a range of dierent) public sources. Public sector funding for these
community delivered services has traditionally been structured through short-term contracts rarely
linked to outcomes. The financial viability of such providers in this climate is sometimes perilous.
A key factor informants identified in the Zero HIV programme as manifested in the community setting
was that it served to increase and simplify financing for this outreach work. In addition, the finance
provided through this programme had more flexibility in terms of what it could be used for and when,
and upfront funding was highly valued by providers as it reduced their sense of risk and also increased
their ability to sta and deliver services before outcomes payments arrived:
‘In the charity sector, we’ve not had much experience with [Payment by Results], so it was
always approached with a bit of hesitancy, and I think the agreements that were made with
EJAF about, okay, well, at least you’ll get an upfront payment of X amount, which gave us
a bit more condence to engage with the process, whereas if it were payment by result from
the very start, we would be quite nervous about, because normally, we’re running things on
a shoestring budget a lot of the time.’
Community provider worker 4
‘The contract says you can be [given advanced funding] and that’s to help you set up, buy
the testing kits, train your people how to do your clinical protocols and then basically get
people to pay, facilitate to pay for people, so you can get supplies and pay your sta to go
and test.’
Community provider worker 2
In addition, the pivot to outcomes-oriented payments incentivised some community provider sta in
what were generally reported as positive ways:
‘It’s been a real motivator for [sta] in terms of getting people. I mean, we’ve always been
good at, as a charity, hand-holding people in, making sure they get to care, but having
that extra incentive for the team has been great… The team are fully aware of the payment
structure, and it has motivated them, and it has, as I said before with engaging already

43
positive people, it’s provided those additional conversations to be happening, and I think
overall, it’s been really good for the team.’
Community provider worker 4
This kind of statement was repeated by all community providers we interviewed. This ‘hand-holding’
concept – whereby the dierent providers developed deep and trusted relationships with their newly
diagnosed (or newly re-engaged) clients was particularly important to clients during the period between
their reactive test and their visit to the HIV clinic for confirmatory test and starting treatment. The theme
also recurred across the interviews with dierent provider organisations and was linked to an informal
‘cosmopolitanism’ (Damschroder et al, 2009) whereby personal networks across charity and NHS
providers were harnessed to facilitate the discrete and smooth transfer of care from trusted community
providers to NHS colleagues:
‘My rst client [identied as part of this programme], he didn’t know he had HIV, and I
made friends with somebody from an organisation… it’s basically like a community … in
London and they’re really nice and I made friends with them and they said ‘oh I know this
person who contacted me asking for how can I get [tested for] HIV…’ and they connected
me with this person and then I took them to Guy’s,[Hospital] well, so my friend from this
community advisory board was going to take them to Dean Street and I was like ‘no, no,
no, wait a minute’ and then I contacted *‘David’ at Guy’s, so the consultant, and I was like
‘’David [I have this patient, can I bring him to you?]’ and then he was like ‘yeah, of course’
and then I just cancelled the appointment at Dean Street… took the guy to Guy’s, he was
positive, and then that’s how I leave them with treatment, we went for a coee aer, we get
on very well,[and keep in touch aer the diagnosis]’
Community provider worker 1
*Name changed to respect anonymity
This cosmopolitanism is linked to long-standing relationships between non-NHS and NHS HIV workers
but there is also a sense in which EJAF furthers this through regular meetings and data sharing as part
of the wider ‘outer-setting’ and policy conditions linked to the programme. Beyond this, the community
providers engaged in cosmopolitan activities by definition – delivering testing in a wide range of
community settings such as clubs, bars, barber shops, shopping centres and more. COVID-19 and the
resultant restrictions placed on social interaction impacted on the feasibility of such tactics (Stanworth,
2022). This led to community organisations targeting known people living with HIV who had disengaged
from NHS care, or new arrivals to London from outside if the UK with an existing HIV diagnosis who
were yet to access NHS care. This generally points to the high level of flexibility built into the Zero HIV
programme at the community level. It was highly adaptable and pragmatic.
Whilst the general picture here is positive – in terms of the Zero HIV programme enabling these
community organisations to successfully provide targeted out-reach to often vulnerable or marginalised
people and support them to secure NHS care, there were problematic issues highlighted by community
informants. Mostly these were linked to the ways that the SIB contract interacted with existing London
HIV prevention programme work leading to possible perceptions of ‘double-dipping’ that had to be
navigated, and also that the level of HIV positivity in the community meant that the cost of work needed
to achieve an outcome might not be recouped through the outcome payment.

44
In summary, the Zero HIV programme was welcomed by community providers as it released funds to
enable them to provide services in flexible, adaptable ways. The programme encouraged cosmopolitan
working practices across non-NHS and NHS organisations and actors and delivered welcome central
guidance and support – often from EJAF. The PbR model and level of outcomes payments were seen as
positive innovations.
Sustainability
It will come as little surprise, having read thus far, that there was a unanimous desire for many aspects of
the Zero HIV programme to continue beyond 2021. Opt-out testing in the hospital setting – particularly
ED - was seen as a major priority, and many respondents were keen that the work piloted in the ED
departments involved in the programme be spread to other local EDs also. Likewise, there was support
for further opt-in testing in primary care, and a desire for communities of practice and opinion leadership
activities such as the HIV GP champion programme to be sustained. In addition, HIV specialist clinicians
were particularly keen for the LTFU work to continue beyond 2021. The picture in relation to community
testing and LTFU work was slightly more contested. Whilst all informants recognised the value of
community outreach activities provided by the not-for-profit sector, there was a concomitant belief that
such work would continue to be funded in various ways going ahead.
There was a mixed set of opinions in relation to the necessity and desirability of the SIB-specific
elements of the Zero HIV programme model and whether and to what extent these might be integral
to the success (and subsequent sustainability) of the dierent interventions developed as part of the
programme. SIB-specific elements included the (1) utility/nature of the outcomes payment model, (2)
the level at which the outcomes payments themselves were set, and (3) the performance management
and coordinating role played by EJAF. Some informants felt these aspects would be helpful to maintain
and improve service levels after 2021 (e.g., one of the HIV GP Champions questioned whether the time/
space for sharing ideas and learnings related to HIV prevention and care in Primary Care would even be
possible without the facilitating role played by EJAF), whilst others did not.
A further issue that divided informants related to the extent to which the services developed and
financed as part of the Zero HIV programme should subsequently be funded through the public sector
(e.g., standard NHS budget lines), or whether non-public sector financing (e.g., SIB, investors etc.)
as part of the financing mix might bring additional (financial and non-financial) benefits. The on-going
role of EJAF also emerged as an issue in some interviews with some informants suggesting a continued
presence and role could be valuable.
‘In terms of what should happen, I think those things should be funded by the government.
I think the kind of economic modelling that we did – and the problem is that these things
outlive political cycles – but the economic modelling that we did really is so compelling to
say do this now, don’t wait for the problem later, that I think it’s what they should do. And
I also think that there are opportunities not just in ED but also in Primary Care for – and I
think with a fair wind because of COVID-19 this is more likely now – for a much greater
push on early testing and early diagnostics for a whole range of things to then proactively

45
see what’s circulating in society and in the system and what’s the best way to address it.
So, I don’t know whether that will happen. I think it might, but I think it should. I think
there should be a much better sense proactively of doing those things. In terms of the SIB
more generally and community involvement and so on, my own view is that I think they’re
incredibly eective mechanisms at focusing and galvanising people round a specic aim,
but I don’t think that they’re the right mechanism long term for a lot of things, because I
think there’s a real risk that they create all kinds of perverse incentives and they give you
a very tunnel vision, which is useful in the rst instance but can mean that you miss the
bigger picture in the long term.’
EJAF participant 4
‘What EJAF has done is take the space and the bandwidth they’ve got, to go this is
something that you need to be doing but you’re not doing, and we’re giving you a
framework to do it in, and we’re going to do the business support and the back end and
we’re going to do all the organising and part of that is the money for the resourcing, and
we’re going to show you that it can be done and how you can do it, and so, from my point
of view, that’s what that’s brought.’
National NHS organisation informant
This latter point is demonstrated by EJAF’s use of the evidence to inform policy and commissioning
across national, regional, and local levels, culminating in the commitment in the government’s HIV
Action Plan to commit £20m to ED HIV testing in very high areas of HIV incidence.
A division in relation to informant views sometimes emerged between front-line HIV clinicians and
those in commissioning roles. As might be expected, HIV specialists were very keen for HIV services
developed as part of the programme to be sustained and were confident that the evidence generated
by the programme supported this. Those commissioning services sometimes took a slightly dierent
line, questioning the strength of the evidence generated by the programme particularly in relation to
questions of attribution and a lack of detailed health economics data related to the dierent elements
of the programme.
‘I think that’s the takeaway, and I’d say that whilst we hoped that, I suppose, we hoped
that the SIB would get us there, I think that we’re still at least all talking to each other
and working towards that goal. I think it’s challenging to make the nancial case without
that evidence, and it may be that we don’t get everything that we want now in terms
of agreement, but at least if we’re looking to evidence, looking to continue to build the
evidence base, then that will help us to secure future funding as well, as a system.’
Commissioner 2
These issues surface both the strengths and the weaknesses of the SIB as a mechanism to promote
sustainable inter-organisational change in public sector service commissioning. The status quo ante
mitigated against reliable and sustainable resources for the HIV services because of siloed funding
streams. The SIB funding model developed as part of this programme counters the problem of siloed
funding in the short term but not the long term.

46
‘That’s the really key piece of this, I think, is that there are savings implied, but the savings
are so dispersed across a system that it’s hard for anyone to take responsibility for the
upfront costs, because they don’t know if they’re going to get the gains of the savings,
because they don’t know if the savings will actually go to them or it’ll go King’s College
Hospital or if it’ll go somewhere in Oxford because the person will have moved by then,
you know? And it’s very interesting, because the NHS to an outsider might seem like, well,
it will just accrue to the NHS, but the NHS is segmented and there’s so many dierent
buckets of funding that that’s not… Even though the savings will accrue somewhere across
the whole system, no specic stakeholder gets that.’
EJAF manager 1
The SIB cut through the existing complex and contrary bureaucratic structures and provided the
resources (financial, managerial, and clinical) to deliver improvements in HIV service provision.
However, the lack of a robust impact evaluation or baseline work means that the standard of evidence of
eectiveness may be below that needed by commissioners to justify the continuance of such services. In
addition, the level of funding aorded by the SIB model (and informal de-risking of some organisations –
such as NHS trusts) may make the reproduction of the same or similar services ex post dicult.
‘I think working with EJAF has been, it’s been helpful in that they have a huge amount of
enthusiasm for this, they want it to work, they push, push, push to make that happen, and
we do tend to, a little bit, in the NHS and in councils, get a bit bogged down in process and
all the rest of it. So, in a way, they released us from a little bit of that by really pushing. The
contrary to that is that we do have lots of processes and stu that we have to do because
that’s the way it’s set up, which was equally a frustration on their part, because why does
everything take so long and why do you have to bang on about all these other things. And
so, that’s always a little bit of a challenge, balancing those two things o… [For] example,
it’s the data collection stu where we wanted baselines. We were really keen to understand
what our baseline was of who was coming through, what those numbers were and that
issue around what the marginal case base would be versus, rather than just everybody, they
were just like, well, just count everybody. So, that’s a good example where we’re like, well,
if we’re going to fund this, we need to know what it costs over and above what we were
already doing.’
Commissioner 4
The SIB model is eective in reframing the existing inauspicious inter-organisational and health
funding context and super-charging innovation and experimentation – however, the extent to which
the inter-organisational context and funding channels may be substantively and sustainably made
more auspicious by the SIB experiment remains an open question which we can only answer over the
longer term. In this particular case, the timing of the end of the SIB financing may be helpful in terms
of generating sustainable change as it is concurrent with a wider NHS reconfiguration aimed at better
integration, collaboration and aggregation of commissioning and service provision – though the extent to
which any new structures will deliver firm change was questioned by some informants.
In summary, most informants expressed a desire that most aspects of the Zero HIV programme would
be sustained after the SIB funding ended in 2021. However, many informants feared that a reversion to
pre-SIB funding regimes represented a risk to this occurring. This is an important question for further
research to explore.

47
Conclusions
In this concluding section we return to our original research questions and seek to respond to each of
these in the light of our findings.
1. What do key stakeholders perceive to be the organisational and health impacts of the Zero HIV
intervention?
2. Through what mechanisms, how, and why, does the Zero HIV intervention impact upon the
behaviour, attitudes, and actions of:
(a) Service users?
(b) NHS and non-NHS providers?
(c) NHS and Local Authority commissioners?
(d) Wider stakeholders including those involved in financing, evaluating, and overseeing the Social
Impact Bond element of the intervention?
3. How might these impacts and behaviour changes be sustained:
(a) In South London after the SIB financed programme ends in December 2021?
(b) And/or transferred to other geographical settings?
In relation to the first research question, we found extensive qualitative evidence that services
users alongside clinical, managerial, and other NHS and non-NHS stakeholders viewed the Zero
HIV programme as delivering significant and highly desirable organisational and health impacts. In
organisational terms, the programme was very eective in challenging and removing many of the existing
barriers to HIV testing and LTFU work. As highlighted in this report many such barriers are related to
funding silos and conflicting incentives across primary and secondary care as well as in the community.

48
The Zero HIV programme was very eective in identifying these barriers and devising innovative
solutions to these – encouraging flexibility and adaptability through the COVID-19 pandemic.
Furthermore, the programme encouraged greater inter-organisational collaboration and increased
sharing of ideas through a more cosmopolitan approach within and across the organisations involved.
In terms of the health impacts, stakeholders were likewise confident that the programme was reaching
new HIV patients and very eectively engaging with them and enrolling them on to HIV treatment. The
programme also made valuable strides in systematising LTFU outreach work and re-engaging patients
who had disengaged from care. The descriptive statistics and wider quantitative analyses presented
earlier give a sense of the scale and scope of this work.
Turning to the second question, there are a number of significant mechanisms through which the
programme impacted upon behaviour, attitudes, and actions of the various stakeholders. From the
perspective of both service users we interviewed, it was apparent that they very much valued the
normalisation of HIV testing and the care and dedication demonstrated by those who deliver their
ongoing care. The oer of a rapid HIV test, early diagnosis and excellent all-round care from NHS
specialist HIV clinical teams was highly valued by both patients we interviewed. Timely access to the
right medication alongside good overall emotional support from NHS clinicians has transformed the lives
of these individuals.
For the provider organisations including NHS hospitals, GP surgeries and non-NHS organisations
such as local charities providing HIV outreach, testing and support, the Zero HIV programme enabled
them to reach a wider selection of people living with HIV than previously. This is linked to changes in
what Damschroder et al. (2009) term as the ‘outer setting’ – or the inter-organisational space which
influences change at the individual provider level. Key here was increased cosmopolitanism and
cross-organisational exchanges prompted by the programme. EJAF were identified as valued external
change agents who met regularly with all provider organisations and worked with them where needed
to help them achieve their outcomes. This fostered a positive culture in which measurement and
evaluative practice were used productively. The programme encouraged increased and more accurate
measurement and reporting of both new diagnoses and LTFU across all providers.
This measurement regime was stimulated by the need to evidence performance in order to access the
increased and better targeted funding for provider organisations that came with the programme. The
shift to an outcomes-based approach to financing HIV services was reported to have been significant
for some of the provider organisations. The increased emphasis on HIV testing and LTFU work in
provider organisations alongside the increased and more generous funding stream in turn increased the
visibility and salience of HIV within each provider organisation, thereby achieving greater organisational
prominence and management interest and protecting stang levels and organisational focus. This in
turn enabled the establishment of an organisational ‘inner-setting’ (Damschroder et al., 2009) in which
the passion and dedication of sta to identify and help those living with HIV was allowed to flourish
(rather than be stymied by lack of resources or misaligned priorities) across the provider organisations.
This service evaluation found the NHS and Local Authority commissioners involved in the programme
welcomed the programme and valued the increased and better targeted funding for HIV diagnosis and
LTFU. They also welcomed the work done by EJAF as external change agents and that learning from
the programme has value in guiding their decisions in relation to how to manage HIV services in the

49
longer term. We found that other stakeholders involved in the programme – such as SIB investors were
generally quite removed from issues around implementation of the organisational and clinical changes
prompted by the programme. We expect their roles will be discussed in greater detail by the Ecorys/ATQ
research team in their third and final report.
We now turn to questions of sustainability. The timing of this report is rather unfortunate falling as it does
between the end of the SIB-financed programme (December 2021) and the establishment of the new
financial year (April 2022) and consequent HIV strategic plans for South London linked to the new ICS.
A number of informants speculated that elements of the programme may well continue into the future
– for instance, ED HIV testing and the local GP champion programme if funds can be secured for these.
Questions remain however about whether standard (i.e., non-SIB) funding may have the same impacts
as that of the SIB. Can the gains around cosmopolitanism, coordination, collaboration, and high-quality
measurement be sustained in South London? Only time and further research will tell.
Our final research question, about the transferability of the findings from the programme is also dicult
to answer at this time. Much will depend on national government and regional NHS decisions. However
EJAF have provided evidence from the SIB programme to the HIV Commission, the APPG HIV Testing
Inquiry, the APPG Impact of HIV on BAME Inquiry, and the HIV Action Plan working group, which led
to the HIV Action Plan 2021 introducing £20m funding for ED HIV testing in very high areas of HIV
incidence – so EJAF certainly hope this programme can influence the agenda at a national level – but
once more, time and further research are required to answer the question properly.
In relation to the quantitative questions we explored, we found evidence that the programme managed
to reach marginalised groups of people who perhaps would not normally come into contact with HIV
testing services elsewhere - thus suggesting the programme may have the potential to address health
inequalities in a positive manner.
We conclude this report with a note on the need for further research and the possible avenues this
might take.
In terms of HIV service provision in South London, further mixed methods research into the sustainability
of the testing and LTFU work pioneered as part of this programme would be valuable – both from
an implementation and improvement science sustainability perspective, as well as to inform wider
understandings around the longer-term impacts of policy innovations such as SIBs and outcome-
oriented approaches to the commissioning of public services.
In addition, it would be very helpful to have detailed independent research into the health economic
impacts of the dierent aspects of the programme conducted. This would enable local and national
commissioners to gain an accurate understanding of the health economics and wider costs implications
of the programme facilitating future policy decisions to be better informed by evidence.

50
References
Blundell, J., Rosenbach, F., Hameed, T., &
FitzGerald, C. (2019). Are we rallying together?
Collaboration and Public Sector Reform,
Government Outcomes Lab, University of Oxford,
Blavatnik School of Government.
Carter, Eleanor (2020): More than marketised?
Exploring the governance and accountability
mechanisms at play in Social Impact Bonds.
Journal of Economic Policy Reform. 24(1), 78-94.
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh,
S. R., Alexander, J. A., & Lowery, J. C. (2009).
Fostering implementation of health services
research findings into practice: a consolidated
framework for advancing implementation science.
Implementation science, 4(1), 1-15.
Edmiston, D., & Nicholls, A. (2018). Social Impact
Bonds: The role of private capital in outcome-
based commissioning.Journal of Social
Policy,47(1), 57-76.
Eisenhardt, K. M. (1989). Building theories from
case study research. Academy of management
review, 14(4), 532-550.
Fontana, A., & Frey, J. H. (2000). The interview:
From structured questions to negotiated text.
Handbook of qualitative research, 2(6), 645-672.
Fraser, A., Tan, S., Kruithof, K., Sim, M., Disley,
E., Giacomantonio, C., Lagarde, M., & Mays,
N. (2018). Evaluation of the social impact
bond Trailblazers in health and social care final
report. Policy Innovation Research Unit: https://
researchonline.lshtm.ac.uk/id/eprint/4650174/1/
SIB%20Trailblazers%20Evaluation%20final%20
report.pdf
Fraser, A., & Mays, N. (2020) ‘Case Studies’ in
Pope, C., & Mays, N. (eds) Qualitative Research in
Healthcare 4th Edition. Wiley, London
Glaser, B. G. (1965). The constant comparative
method of qualitative analysis. Social problems,
12(4), 436-445.
Glaser, B. G., & Strauss A., L., (1967). The discovery
of grounded theory: strategies for qualitative
research. New York
Greenhalgh T, Robert G, Macfarlane F, Bate P,
Kyriakidou O. (2004) Diusion of innovations
in service organizations: systematic review and
recommendations. Milbank Quarterly, 82:581-
629.
Langley, A. (1999). Strategies for theorizing from
process data. Academy of Management Review,
24(4), 691–710.
Public Health England (2018) HIV Southeast Annual
Data Spotlight: https://www.gov.uk/government/
publications/hiv-south-east-annual-data-spotlight
Public Health England (2019) Trends in HIV testing,
new diagnoses and people receiving HIV-related
care in the UK: data to end December 2019
Health Protection Report Volume 14 Number
20: https://assets.publishing.service.gov.uk/
government/uploads/system/uploads/attachment_
data/file/959330/hpr2020_hiv19.pdf
Stanworth, N. (2020) The Zero HIV Social Impact
Bond: Commissioning Better Outcomes Fund
Evaluation: In depth review (1). https://www.
tnlcommunityfund.org.uk/media/insights/
documents/EJAF-Zero-HIV-in-depth-review_
FINAL.pdf
Stanworth, N. (2022) The Zero HIV Social Impact
Bond: Commissioning Better Outcomes Fund
Evaluation: In depth review (2). The impact
of the Zero HIV COVID-19 pandemic: https://
www.tnlcommunityfund.org.uk/media/insights/
documents/Zero-HIV-Social-Impact-Bond-2.
pdf?mtime=20220224150943&focal=none
Yin, R. K. (2009). Case study research: Design and
methods (Vol. 5). Sage.

