
Philip R. Lee Institute for Health Policy Studies
The Future of Oregon’s
Nursing Workforce:
Analysis and
Recommendations
Final Report
October 18, 2022
Timothy Bates, Emily Shen, & Joanne Spetz, University of California, San Francisco
Jana Bitton & Rick Allgeyer, Oregon Center for Nursing
Acknowledgements:
This report benefitted from the support and guidance of Marc Overbeck, Director of the Primary Care
Office, and Neelam Gupta, Director of Clinical Supports, Integration, and Workforce, at the Oregon
Health Authority.
We appreciate the input of the project’s Advisory Group, chartered by the Oregon Health Care
Workforce Committee: Patricia Barfield (Oregon Health & Science University), Susan Burke
(PeaceHealth), Matthew Calzia (Oregon Nurses Association), April Diaz (Marquis Companies), Andi
Easton (Oregon Association of Hospitals and Health Systems), Ruby Jason (Oregon State Board of
Nursing), Paula Love (Avamere), Becky McCay (Oregon Health & Sciences University), Desi McCue
(Providence Health and Services), Jane Morrow (Central Oregon Community College Nursing
Program), Jane Palmieri (Portland Community College Nursing Program), Cathy Reynolds (Legacy
Health), Tina Ronczyk (PeaceHealth), Melody Routley (Kaiser Permanente), Casey Shillam (University
of Portland), and Jackie F. Webb (Oregon Health & Science University).
The Oregon Health Care Workforce Committee provided support and comments throughout our
research. We are particularly appreciative of Troy Larkin (Providence Health and Services), as well as
Chair Laura McKeane (AllCare Coordinated Care Organization), Vice-Chair Paul Gorman (Oregon
Health & Sciences University), and Immediate Past Chair Curt Stilp (George Fox University), for their
engagement in the Advisory Group and frequent feedback.
Representative Rachel Prusak sponsored the legislation that made this report possible. Her support
and feedback are greatly appreciated.

Future of Oregon’s Nursing Workforce
2
Table of Contents
List of Tables .............................................................................................................................................................4
List of Figures ...........................................................................................................................................................5
Project Purpose ........................................................................................................................................................7
Nursing Practice in Oregon and the Nation ...........................................................................................................8
What is Nursing? ........................................................................................................................................................8
Nurse License Types and Specialties ........................................................................................................................8
Licensing and Regulation of Nurses ........................................................................................................................ 10
The Role of the Oregon State Board of Nursing ..................................................................................................... 12
Emergency Authorization Licensure 2020-2022 ........................................................................... 13
Perceptions of OSBN among key informants ................................................................................ 14
Solutions to OSBN Licensing Delays ............................................................................................ 15
Overview of Oregon’s Nursing Workforce .......................................................................................................... 15
Size and Demographics .......................................................................................................................................... 15
Number of Nursing Professionals in Oregon ................................................................................. 15
Age Distribution of Oregon Nurses ................................................................................................ 16
Gender of Oregon nurses .............................................................................................................. 17
Racial and ethnic diversity of Oregon nurses ................................................................................ 17
Languages spoken by Oregon nurses .......................................................................................... 18
Education and Training of nurses in Oregon ........................................................................................................... 19
Quality of Oregon’s nursing education programs .......................................................................... 23
Highest Educational Attainment of Oregon RNs ........................................................................... 25
Inter-state migration of nurses ................................................................................................................................. 29
International recruitment and immigration ............................................................................................................... 30
Patterns of Nurse Employment ................................................................................................................................ 31
Compensation of nurses .......................................................................................................................................... 31
Current Challenges for the Nursing Workforce .................................................................................................. 36
The national context ................................................................................................................................................ 36
Nursing shortages .................................................................................................................................................... 37
Ramifications of nursing shortages on organization operations and new graduate onboarding .. 38
Nurse vacancies ............................................................................................................................ 38
Retention of Nurses in Oregon ...................................................................................................... 39

Future of Oregon’s Nursing Workforce
3
Nurse workloads ...................................................................................................................................................... 42
The importance of nurse workload ................................................................................................ 42
Nurse workload in Oregon ............................................................................................................. 43
Responses to deal with increased workload ................................................................................. 44
Regulatory approaches to manage nurse workloads .................................................................... 44
Oregon’s 2015 Nurse Staffing Law ............................................................................................... 46
Nurse burnout .......................................................................................................................................................... 48
National estimates of nurse burnout .............................................................................................. 48
Factors contributing to nurse burnout ............................................................................................ 48
Effect of Nurse Burnout on Patient and Organizational Outcomes ............................................... 49
Evidence for mitigating burnout ..................................................................................................... 49
Oregon Center for Nursing’s Survey on Nurse Burnout ................................................................ 50
Nursing education capacity in Oregon..................................................................................................................... 58
Faculty shortages .......................................................................................................................... 58
Lack of Clinical Placements ........................................................................................................... 59
Transition into Practice for New Nurse Graduates .................................................................................................. 60
Strategies to address transition-to-practice challenges ................................................................ 61
Challenges with the LPN and CNA workforce ......................................................................................................... 63
Solutions Implemented and Considered in Oregon ........................................................................................... 64
Oregon Wellness Program ............................................................................................................ 64
Temporary Licensure ..................................................................................................................... 65
Nurse Intern Licensure .................................................................................................................. 65
Nurse Licensure Compact ............................................................................................................. 65
Conclusions and Recommendations .................................................................................................................. 68
Conclusions ............................................................................................................................................................. 68
Recommendations ................................................................................................................................................... 69

Future of Oregon’s Nursing Workforce
4
List of Tables
Table 1. License types and current numbers, 2022. ............................................................................. 13
Table 2. Applications and licenses issued, Jan. - Aug. 2022. ............................................................... 14
Table 3. Numbers of licensed and certified nurses in Oregon. ............................................................. 16
Table 4. Racial/ethnic distribution of Oregon nurses by license type. ................................................... 18
Table 5. Languages spoken by license type. ....................................................................................... 18
Table 6. Programs offered by Oregon's RN and LPN education programs. ......................................... 20
Table 7. Total student enrollment in practical nursing programs. ......................................................... 22
Table 8. Highest educational attainment of Oregon RNs, 2014-2020. .................................................. 25
Table 9. Enrollment and graduation by race/ethnicity in Oregon's RN programs over time. ................. 26
Table 10. Race/ethnicity of practical nursing students.......................................................................... 26
Table 11. Age of practical nursing students and graduates. ................................................................. 27
Table 12. Detailed description of employment settings used in the NSSRN, 2018. .............................. 34
Table 13. Median hourly wage by region and occupation, 2022. .......................................................... 35
Table 14. Hospital vacancies in Oregon and other states, 2019. .......................................................... 38
Table 15. Hospital full-time equivalent employment per 1000 adjusted patient days, 2019. ................. 43
Table 16. Nurse Well-Being Mental Health Survey respondents. ......................................................... 51

Future of Oregon’s Nursing Workforce
5
List of Figures
Figure 1. Age cohort by license type. ................................................................................................... 16
Figure 2. Age distribution for Oregon registered nurses, 2012 vs. 2020. .............................................. 17
Figure 3. Gender distribution of Oregon nurses by license type. .......................................................... 17
Figure 4. Locations of Oregon's RN and LPN education programs. ..................................................... 19
Figure 5. Total enrollment in Oregon's RN programs. .......................................................................... 21
Figure 6. New enrollments in Oregon's RN programs. ......................................................................... 21
Figure 7. Numbers of qualified applicants to Oregon RN education programs. .................................... 22
Figure 8. Registered nurse graduates over time. ................................................................................. 23
Figure 10. NCLEX-RN first time pass rate, Oregon vs. U.S.................................................................. 23
Figure 11. Oregon's NCLEX-RN first time pass rate by program type. ................................................. 24
Figure 12. Graduates by age group in Oregon's RN programs............................................................. 27
Figure 9. Graduations from practical nursing programs. ....................................................................... 28
Figure 13. Number of RN licenses approved by year of licensure. ....................................................... 29
Figure 14. Percent of RNs practicing in Oregon by method of licensure. ............................................. 30
Figure 15. Practice settings of Oregon RNs. ........................................................................................ 31
Figure 16. Median income from all nursing employment by full-time/part-time status, Oregon vs. U.S.,
2018. ............................................................................................................................................ 32
Figure 17. Nursing practitioner median income from all nursing employment by full-time/part-time
status, Oregon vs. U.S., 2018. ...................................................................................................... 32
Figure 18. Full-time median income from all nursing employment, by highest level of education,
Oregon, 2018................................................................................................................................ 33
Figure 19. Full-time median income from all nursing employment, by nursing experience, Oregon, 2018.
..................................................................................................................................................... 33
Figure 20. Annual median income from all nursing employment earned by full-time RNs, by
employment setting, 2018. ............................................................................................................ 34
Figure 21. Percentage of RNs employed who were also employed in nursing one year before, Oregon
vs United States, 2018. ................................................................................................................. 40
Figure 22. Change in Nursing Employment Location from Prior Year, Oregon vs United States, 2018. 40
Figure 23. Change in nursing position and employer from prior year, Oregon vs. U.S., 2018............... 41
Figure 24. Change in nursing employment status from prior year, Oregon vs. U.S., 2018. .................. 41
Figure 25. Age of RN Well-Being Mental Health Survey respondents. ................................................. 51
Figure 26. Work settings of RN Well-Being Mental Health Survey respondents. .................................. 52
Figure 27. Years of experience of RN Well-Being Mental Health Survey respondents ......................... 52
Figure 28. Feelings regularly experienced at work. .............................................................................. 53
Figure 29. Top five workplace stressors. .............................................................................................. 53

Future of Oregon’s Nursing Workforce
6
Figure 30. Symptoms experienced recently by respondents. ............................................................... 54
Figure 31. Do nurses receive adequate emotional support at work? .................................................... 55
Figure 32. Do nurses receive adequate emotional support at home? ................................................... 55
Figure 33. Changes in work environment nurses say they need. ......................................................... 56
Figure 34. Changes in work environment nurses say they want. .......................................................... 56
Figure 35. Number of faculty at Oregon’s RN programs. ...................................................................... 59
Figure 36. Known nurse residency programs in Oregon. ..................................................................... 63

Future of Oregon’s Nursing Workforce
7
Project Purpose
The Oregon Health Care Workforce Committee was directed by the Oregon Legislature (HB 4003) to
conduct a study of Oregon’s nursing workforce to identify and describe challenges in addressing
staffing shortages in nursing. This study is intended to provide information to inform the legislature and
Oregon Health Authority (OHA) in their efforts to address critical concerns about nursing workforce
shortages. The study considered all levels of care, including, but not limited to, hospitals, long-term
care facilities, community health centers, home health, public health, and schools.
The specific topics which interested the legislature and committee included:
• size and characteristics of the Oregon nursing workforce;
• administrative capacity of the Oregon State Board of Nursing (OSBN) to process licenses and
renewals, monitor disciplinary actions, and track the workforce, and related regulatory issues, such
as reciprocity with other states and the Nurse Licensure Compact (Compact);
• training capacity in Oregon, including availability of clinical placements;
• transition of newly graduated nurses into practice, including the workload impact to incumbent nurses
of onboarding newly graduated nurses;
• compensation of nurses, including both wages and benefits, across employment settings and nurse
experience;
• workload of nurses, including variation across settings, the use of unlicensed assistive personnel,
and the impact of skill mix;
• nurse burnout, retention, and vacancies across employment settings, age groups, and experience
levels;
• concerns about current and potential nursing shortages;
• inter-state migration of nurses;
• international recruitment and immigration; and
• the impact of the COVID-19 pandemic on the nursing workforce.
The cultural responsiveness of the nursing workforce is a foundational concern of the legislature and
Health Care Workforce Committee. In this context, cultural responsiveness describes the capacity of
the nursing workforce and of individual nurses to respond to the issues of diverse communities. The
cultural responsiveness of the workforce and of individual nurses aims to assure competent language
access and incorporation of diverse cultural approaches, strengths, perspectives, experiences, frames
of reference, values, norms and performance styles of clients and communities to make services and
programs more welcoming, accessible, appropriate and effective for all intended recipients. The domain
of cultural responsiveness was interwoven with each of the specific topics to ensure this foundational
domain was considered in every aspect of this work.
Our research team undertook a number of activities for this study. We began with reviews of the
national literature on nurse staffing, burnout, workloads, and the impact of COVID-19. We also
examined the literature on nurse transition-to-practice and education. We analyzed license and

Future of Oregon’s Nursing Workforce
8
education data from OSBN, licensing survey data from the Health Care Reporting Program, and nurse
well-being survey data from the Oregon Center for Nursing (OCN). We also analyzed data from the
U.S. American Community Survey, the U.S. Bureau of Labor Statistics, the 2018 National Sample
Survey of Registered Nurses, the Oregon Employment Department, and the American Hospital
Association. Finally, we conducted interviews with leadership from OSBN, the Oregon Nurses
Association (ONA), the Oregon Association of Hospitals and Health Systems, the Oregon Health Care
Association, and the Northwest Organization of Nurse Leaders. We interviewed hospital chief nursing
officers and clinical education leaders from rural and urban hospitals, experts in long-term care and
ambulatory care, deans and directors of registered nurse (RN) and licensed practical nurse (LPN)
education programs, and staff nurses.
Nursing Practice in Oregon and the Nation
What is Nursing?
Nursing is the largest health profession in the world and in the United States, with more than 4.2 million
RNs,
1
640,000 employed LPNs,
2
and 1.3 million employed certified nursing assistants (CNAs).
3
Nursing practice involves providing holistic care that includes monitoring patients and assessing their
situation and status, administering treatments and medications, supporting basic needs such as
toileting and feeding, providing education to patients and their families, and collaborating with
interprofessional teams.
Nursing practice spans many care domains across the life span, including disease prevention, health
education, treatment, supporting people living with disabilities, care coordination, and end-of-life care.
Nurses work closely with patients and the public, bringing a scientific understanding of care processes
that gives them what the Institute of Medicine described as “a unique ability to act as partners with
other health professionals and to lead in the improvement and redesign of the health care system and
its many practice environments.”
4
Nurse License Types and Specialties
There are three distinct categories of nursing care providers in the United States, and within these there
are specialties and advanced providers.
Certified nursing assistants (CNA) provide basic care under the direction of licensed nurses. They
support activities of daily living such as bathing, dressing, mobilization, toileting, and eating. Federal
standards for certification require 75 hours of state-approved training, and many states have greater
training requirements. The most common employment settings of CNAs are nursing homes, home
health agencies, and hospitals.
1
American Association of Colleges of Nursing. (2022). Nursing Fact Sheet. https://www.aacnnursing.org/news-Information/fact-
sheets/nursing-fact-sheet.
2
U.S. Bureau of Labor Statistics. (2022). May 2021 National Occupational Employment and Wage Estimates.
https://www.bls.gov/oes/current/oes_nat.htm
.
3
U.S. Bureau of Labor Statistics. (2022). May 2021 National Occupational Employment and Wage Estimates.
https://www.bls.gov/oes/current/oes_nat.htm
.
4
Institute of Medicine. (2011). The Future of Nursing: Leading Change, Advancing Health. Washington, DC: The National Academies Press.

Future of Oregon’s Nursing Workforce
9
Licensed practical nurses (LPNs), called licensed vocational nurses in California and Texas, are
licensed professionals who provide basic nursing care including monitoring vital signs, administering
medications, and performing other tasks such as dressing changes and basic management of
intravenous lines. LPNs complete 12 to 18 months of education at a community college or
vocational/technical school and pass a national certification exam (the NCLEX-PN). The most common
employment settings of LPNs are home health, nursing homes, physician offices, and hospitals.
Registered nurses (RNs) provide essential nursing services including patient assessment and
monitoring, administering treatments and medications, educating patients and family members, and
coordinating care. According to ORS 678.010 (8)(a), the practice of nursing in Oregon means
“diagnosing and treating human responses to actual or potential health problems through services such
as identification thereof, health teaching, health counseling and providing care supportive to or
restorative of life and well-being and including the performance of additional services requiring
education and training that are recognized by the nursing profession as proper to be performed by
nurses licensed under ORS 678.010 (Definitions for ORS 678.010 to 678.410) to 678.410 (Fees) and
that are recognized by rules of the board.” Registered nurses complete an education program at a
community college, diploma school of nursing, or university, and pass a national licensing exam
(NCLEX-RN). Some schools offer programs specifically designed for LPNs to easily move into RN-level
education and licensure. RNs are the most numerous of the nursing occupations and many people use
the term “nurses” to refer specifically to RNs. The most common employment setting of RNs is
hospitals, but RNs can be found in every setting where health care and public health services are
provided.
Many RNs work in health care specialties, including critical care, public health, home health,
emergency and urgent care, occupational health, oncology, mental health, palliative care, and
perioperative care. Many of these specialties have their own certifications associated with some
combination of formal education, on-the-job experience, and examination. Some RNs obtain master’s
degrees to support their knowledge in these specialties, as well as in nursing administration, education,
and leadership.
Advanced practice registered nurses (APRNs) are RNs who have completed a master’s degree in
nursing (MSN) or doctor of nursing practice (DNP) in one of four categories:
• Nurse practitioners (NPs) are the most numerous of the APRNs and can specialize in primary care,
specialty care, acute care, and/or psychiatric-mental health care. They take health histories and
provide complete physical examinations, interpret laboratory results and other tests, diagnose and
treat common acute and chronic problems, and provide counseling and education. They refer
patients to other health care professionals when needed.
• Nurse midwives (NMs) provide reproductive and primary care, including management of low-risk
labor and delivery and neonatal care. If they are nationally certified, they are called certified nurse
midwives (CNMs).
• Nurse anesthetists (NAs) administer anesthesia including during surgery, obstetrical procedures,
and for pain management. They provide more than 65 percent of all anesthetics to patients in the
U.S.
4
If they are nationally certified, they are called certified registered nurse anesthetists (CRNAs).

Future of Oregon’s Nursing Workforce
10
• Clinical nurse specialists (CNSs) are trained in a specialty area and practice in a variety of fields
and specialties including adult health, community health, geriatrics, school health, psychiatric-mental
health, and women’s health.
Licensing and Regulation of Nurses
Occupational licensure is the legal structure through which governments establish the qualifications
required to work in a profession. Only individuals with licenses are allowed to work in that occupation.
The intention of occupational licensure is to protect consumers by ensuring that professionals and
tradespeople are qualified for the services they provide.
5
For most occupations, licensure is regulated
by state governments.
6
The U.S. Bureau of Labor Statistics reports 21.3 percent of the civilian labor
force held an occupational license in 2021.
7
Another component of occupational regulation is scope-of-practice regulation. This type of regulation
specifies the types of services and tasks that people in a licensed occupation are allowed to perform.
Scope-of-practice regulations are common among health care occupations and, like licensing
regulations, are generally considered to be the purview of states.
8
There are no federal standards or requirements for nurses to practice. States are expected to define
what constitutes competent and safe practice for nurses who treat their residents. Therefore, it is the
responsibility of each state to set the regulations for nurses and nursing practice.
Nurse regulation in Oregon
In Oregon, regulations related to nurse licensure and practice are defined in the Oregon Nurse Practice
Act, which contains both laws set by the legislature [Oregon Revised Statutes, Chapter 678.010-
678.445] and rules established by the Oregon State Board of Nursing (OSBN) [Oregon Administrative
Rules, Chapter 851].
The Nurse Practice Act sets standards for all aspects of nursing including:
• rules of practice and procedure;
• agency fees;
• nurse certification and licensing;
• scope-of-practice for nursing at all levels (CNAs, LPNs, RNs, and APRNs); and
• approval and standards for nursing education programs.
As is the case in most states, Oregon’s legislature has established broad requirements for nursing
regulation, and the details of regulation are left to the OSBN to determine. This structure supports the
5
Kleiner, M. M., & Vorotnikov, E. (2017). Analyzing occupational licensing among the states. Journal of Regulatory Economics, 52(2), 132-
158.
6
Kleiner, M. M., Marier, A., Park, K. W., & Wing, C. (2016). Relaxing occupational licensing requirements: Analyzing wages and prices for a
medical service. The Journal of Law and Economics, 59(2), 261-291.
7
U.S. Bureau of Labor Statistics. (2022). Statistics from Current Population Survey: Certification and licensing status of the civilian
noninstitutional population 16 years and over by employment status, 2021 annual averages. https://www.bls.gov/cps/cpsaat49.htm
.
8
Gilman, D. J., & Fairman, J. (2014). Antitrust and the future of nursing: Federal competition policy and the scope of practice. Health Matrix,
24, 143.

Future of Oregon’s Nursing Workforce
11
evolution of policies to meet current needs and address emergent issues because it is easier to amend
regulations than laws.
Licensure and certification in Oregon
Nurse licensing requirements in Oregon are similar to those of other states and generally aligned with
the national Nurse Licensure Compact, which is a set of regulatory recommendations developed by the
National Council of State Boards of Nursing (NCSBN). The only substantive difference between
Oregon’s requirements and the Compact requirements is that Oregon allows people who have a prior
felony conviction to apply for licensure as an RN or LPN whereas the Compact does not. The OSBN
reviews prior arrests and convictions and makes determinations on an individual basis.
9
Oregon’s standards for CNAs differ from federal minimum training requirements. The federal standard
is 75 hours of training, of which 16 must be clinical. Oregon requires 155 hours of training. However, a
CNA who is certified by another state can apply to be a CNA in Oregon without completing additional
training even if the other state’s requirements are less than 155 hours. Oregon also has multiple levels
of certification for nursing assistants: CNA 1, CNA2, and certified medication assistant (CMA). To
become a CNA2, a CNA1 must have 75 hours of work experience as a CNA1 or a combination of work
and clinical training that adds to 75 hours, complete additional training in an OSBN-approved program,
and pass that program’s competency evaluation (Oregon Administrative Rules 851-062-0052). To
quality for CMA certification, a CNA can complete an OSBN-approved medication aide training program
and pass an examination. A student in a licensed nursing education program also can qualify as a
CMA, as can military corpsmen or medics and graduations of medication aide programs in other states.
Scope of practice in Oregon
RNs’ scope of practice does not vary substantially across states and Oregon’s scope of practice for
RNs is aligned with nationally accepted standards. In contrast, there is notable variation in LPN scope
of practice across states. Oregon’s scope-of-practice regulations for LPNs provide general guidance
that they must practice in alignment with their training and skills, which affords their employers with
flexibility in the assignment of tasks to LPNs. For example, Oregon regulations allow LPNs to
administer intravenous therapy, at the discretion of their employer, whereas LPNs are not allowed to do
this in California.
NPs and NMs in Oregon have full practice authority, which means they can practice independently to
the fullest extent of their knowledge and training. Oregon’s NPs and NMs are not required to be
supervised by or collaborate with a physician at any time.
10,11
Many other states require that NPs
and/or NMs practice under physician oversight; Oregon is viewed as a leader in allowing their APRNs
to have full practice authority as recommended by the Institute of Medicine.
4
9
For more information, see https://www.oregon.gov/osbn/pages/criminal-history.aspx
10
Spetz, J. (2018). California’s Nurse Practitioners: How Scope of Practice Laws Impact Care. Oakland, CA: California Health Care
Foundation. Revised 2019, July.
11
Kwong, C., Brooks, M., Dau, K. Q., & Spetz, J. (2019). California’s Midwives: How Scope of Practice Laws Impact Care. Oakland, CA:
California Health Care Foundation.

Future of Oregon’s Nursing Workforce
12
CNAs in Oregon have a scope of practice that is quite expansive and aligned with the majority of
states. Some states place more restrictions on CNAs. In Oregon, a CNA1 provides care as directed in
an individual’s plan of care, which is developed by a licensed nurse. The CNA1 may carry out tasks
associated with infection control and prevention, transporting people to a wheelchair or other
specialized chair, using lifts and other client handling devices, turning oxygen on and off, assisting with
eating and elimination, including administering enemas, assisting with personal care such as
shampooing, and a variety of tasks associated with technical skills such as changing a suction canister.
The CNA2 may perform the same functions as a CNA1 and can help clients navigate the acute care
system, obtain throat swabs and urine specimens, assist with human milk pumping and handling, add
fluid to established tube feedings, change tube feeding bags, use adaptive equipment such as braces
and splints, and perform a wider range of tasks that require technical skills.
All CNAs may administer over-the-counter suppositories, topical barrier skin creams/ointments, and
treatments for lice, but they are not allowed to administer any other medications. CNAs can administer
oral, eye, ear, nasal, rectal, and vaginal medications under the direction of a licensed nurse. CNAs also
may administer medications delivered by nebulizers and can administer PRN (as needed) medications.
The Role of the Oregon State Board of Nursing
OSBN’s mission is to protect the public by regulating nursing education, licensure, and practice. OSBN
is responsible for:
• interpreting the Nurse Practice Act;
• conducting rule-making activities for Nurse Practice Act statutes, including public engagement, rule-
writing, and rule implementation;
• evaluating and approve nursing education and nursing assistant training programs;
• issuing licenses and renewals;
• investigating complaints and take disciplinary action against licensees who violate the Nurse Practice
Act;
• maintaining the nursing assistant registry and administer competency evaluations for nursing
assistants; and
• providing testimony to the legislature and other organizations as needed.
12
OSBN is governed by a nine-person board representing a variety of geographic locations and
consisting of two public members, one nurse educator, one nurse administrator, two direct-care non-
supervisory nurses, one licensed practical nurse, one certified nursing assistant, and one nurse
practitioner. As a state agency, OSBN board meetings are open to the public and include public
comment, except in cases of disciplinary hearings and executive session.
As of September 2022, OSBN reported overseeing licenses for more than 113,000 individuals (see
Table 1).
12
Oregon State Board of Nursing. (2022). What We Do. https://www.oregon.gov/osbn/Pages/about-us.aspx.

Future of Oregon’s Nursing Workforce
13
The licensing process at OSBN requires several steps in which staff must directly verify components of
the application, such as transcripts and criminal record checks. According to OSBN, applications can
get delayed whenever a process isn’t automated or is reliant on staff or applicant intervention. Nurse
license applications can be delayed when applicants delay requesting documents required to verify
information such as school transcripts or out-of-state licensing verification, or applicants fail to obtain
fingerprints for background checks in a timely manner. Sometimes, if an applicant abandons the
application without notifying OSBN, the application retains a “Still in Progress” status, requiring staff
follow-up. Also, staff absences or turnover can delay the licensing process.
Table 1. License types and current numbers, 2022.
License Type
Number of
Licensees
Registered Nurses 80,123
Licensed Practical Nurses 6,128
Nurse Practitioners 6,687
Clinical Nurse Specialists 143
Certified Registered Nurse Anesthetists 720
Nurse Emeritus 31
Certified Nursing Assistants 18,979
Certified Medication Aides 850
TOTAL LICENSES 113,661
Source: OSBN Presentation to House Interim Committee on Health Care, Sept. 2022
Emergency Authorization Licensure 2020-2022
The COVID-19 pandemic caused major disruption in the licensing process in Oregon and the entire
country. When Governor Kate Brown issued Executive Order 20-03, which declared an emergency due
to the COVID-19 pandemic, OSBN created a new licensure, “Emergency Authorization Licenses” (EAL,
under OAR 851-001-0145), which allowed health employers to rapidly hire nurses, especially travel
nurses, to respond to increased demand for services. OSBN issued more than 13,000 EALs for out-of-
state nurses to work in Oregon during the pandemic.
Because the EAL was created in response to the Emergency Declaration, the EAL was set to expire
when the Emergency Declaration was rescinded by the Governor on April 1, 2022. OSBN extended
EALs for 90 days to allow nurses to apply for an Oregon license. This caused an increased demand for
Oregon licenses in February and March 2022 for nurses who wished to continue practice after the EAL
expired. The increased demand for licensure led to delays in the processing of applications. After
OSBN extended the EALs, the rush of applications slowed, as seen in Table 2.
Future of Oregon’s Nursing Workforce
14
Table 2. Applications and licenses issued, Jan. - Aug. 2022.
Jan
2022
Feb
2022
March
2022
April
2022
May
2022
June
2022
July
2022
Aug
2022
Total
RN Applications
Received
1,353
1,443 2,738 2,000 1,990 1,836 1,520 1,485 14,365
RN Applications
Issued
778 783 999 1,256 1,169 1,895 1,960 1,472 10,312
CNA
Applications
Received
418 559 649 432 506 652 642 641 4,499
CNA
Applications
Issued
258 356 366 201 208 331 341 259 2,320
Source: OSBN Presentation to House Committee on Health Care, Sept. 2022
Perceptions of OSBN among key informants
Some of those interviewed perceived the processing of nursing license endorsements in Oregon takes
longer than in other states. One interviewee compared the OSBN to the nursing board in Washington
state, giving an example that in Washington, even at the height of the pandemic, the state nursing
board was processing endorsement applications within seven days while the interviewee believed it
took three months or longer to begin processing the application in Oregon. One interviewee described
the entire process taking anywhere from six months to a year to complete. Another stated that
employers have had to delay new employee start dates because OSBN could not process license
applications in a timely manner, and temporary licenses that cover a period of 90 days would often
expire before applications were processed. The OSBN reported in an interview that their time to
process a new application has been reduced from three months to 38 days, and their goal is to process
applications in within two weeks. They also noted that some delays in licensing are due to applicants’
not submitting complete files; OSBN measures its productivity based on when the application is
reviewed from completeness and validity. If the file is complete and valid, licensure occurs almost
immediately.
Some interviewees referenced a “lack of trust” between health care employers and OSBN. The lack of
transparency in the licensing process and the lack of communication between applicants and OSBN
was cited by multiple interviewees as an ongoing source of frustration for both applicants and
employers. Some of those interviewed noted that OSBN does not have any representation from the
long-term care sector, which may lead to decisions that affect organizations and nurses in long-term
care not considering those interests adequately. Some of those interviewed perceive that OSBN lacks
the resources to provide needed technical assistance to both applicants and employers. However,
OSBN reported in our interview that they have enough staff to clear the backlog of applications and
return to normal processing times soon.

Future of Oregon’s Nursing Workforce
15
Solutions to OSBN Licensing Delays
OSBN’s benchmark to processing license applications is between 10 and 14 days. Because of the
increase demand for licenses during the pandemic, the time to process an application is currently about
38 days, down from about 90 days earlier in 2022.
To further reduce the time to process licenses, verification requirements would need to be revisited,
such as criminal background checks, competency verification through testing requirements, and
disciplinary actions taken on nurse licenses from other states.
Overview of Oregon’s Nursing Workforce
Size and Demographics
Number of Nursing Professionals in Oregon
During 2020, almost 90,000 nursing professionals held a license to practice in the state of Oregon. Of
these, an estimated 70,000 are considered currently practicing in Oregon. RNs and CNAs are the most
numerous licensed professions with 59,778 and 18,640 licensees, respectively.
In Oregon, nursing professionals renew their licenses every two years, and a demographic/workforce
survey is conducted during renewal to gather date of birth, race/ethnicity, language spoken, gender,
educational attainment, employment status, practice characteristics. The survey collected race/ethnicity
using federal Office of Management and Budget standards, although a 2022 revision of the survey
incorporates Oregon’s REALD categories. Because of the timing of the survey, little is known about the
employment setting of newly licensed nursing professionals who obtain their first licenses and do not
take the workforce survey. To understand the total supply of nursing professionals in Oregon and take
into consideration newly licensed professionals, OCN developed a method to estimate the number of
practicing licensees. The employment rate of licensees completing the survey is applied to the newly
licensed individuals (and those who did not complete the survey) to estimate the number of practicing
individuals shown below. As can be seen in Table 3, in 2020, approximately 87 percent of CNAs, 83
percent of LPNs, 75 percent of RNs, and 78 percent of APRNs were practicing in their profession. A
survey conducted by the NCSBN reported that 76.6 percent of RNs and 76.5 percent of LPNs
nationwide were employed in nursing in 2020.
13
13
Smiley, R. A., Ruttinger, C., Oliveira, C. M., Hudson, L. R., Allgeyer, R., Reneau, K. A., Silvestre, J. H., & Alexander, M. (2021). The 2020
National Nursing Workforce Survey. Journal of Nursing Regulation, 12(1), S1-S96.

Future of Oregon’s Nursing Workforce
16
Table 3. Numbers of licensed and certified nurses in Oregon.
Certified Nursing
Assistants (CNA)
Licensed Practical
Nurses (LPN)
Registered
Nurses (RN)
Advanced Practice
Registered Nurses (APRN)
Licensed 18,640 5,644 59,778 5,574
Practicing 16,200 4,680 44,900 4,330
Percent
Practicing
86.9% 82.9% 75.1% 77.7%
Source: OHA, Public Use Nursing Workforce Data File, 2020
Age Distribution of Oregon Nurses
Oregon nurses tend to be younger than in other states. The median age of an RN in Oregon is 51
years,
14
as compared to a median age of 52 for RNs nationwide.
13
The national sample shows the
largest cohort of RNs is over the age of 55. As seen in Figure 1, the largest age cohorts for CNAs,
LPNs, and RNs are 25-34 and 35-44, while the largest age cohorts for NPs are 35-44 and 45-55.
This trend of a younger nursing workforce has been developing for many years. In 2012, for example,
the largest age cohort of nurses was those between 55 and 60 years old (see Figure 2). Eight years
later, the largest age cohort is now between the ages of 30 and 35.
Figure 1. Age cohort by license type.
Source: OHA, Public Use Nursing Workforce Data File, 2020
14
Oregon Health Authority. (2020). Public Use Nursing Workforce Data File.
-4,000
1,000
6,000
11,000
16,000
<25 25-34 35-44 45-55 55-64 65+
CNA LPN RN NP

Future of Oregon’s Nursing Workforce
17
Figure 2. Age distribution for Oregon registered nurses, 2012 vs. 2020.
Source: OHA Public Use Nursing Workforce Data File, 2012 and 2020
Gender of Oregon nurses
Currently, about 14 percent of licensed RNs in Oregon are male; nationally 9.4 percent of licensed RNs
are male.
13
Generally, the percent of male RNs and APRNs has grown over time. There are no data
with which the gender distribution of CNAs can be tracked over time.
Figure 3. Gender distribution of Oregon nurses by license type.
Source: OHA, Public Use Nursing Workforce Data File, 2020
Racial and ethnic diversity of Oregon nurses
Racial/ethnic minority groups are under-represented in Oregon’s nursing workforce compared to the
racial/ethnic makeup of the state’s population, although this representation is improving. In 2020, about
77 percent of licensed RNs identified as white, while 74 percent of the population of Oregonians
identified as white (see Table 4). In 2016, more than 88 percent of licensed RNs identified as white.
0
200
400
600
800
1,000
1,200
1,400
1,600
1,800
2,000
20 25 30 35 40 45 50 55 60 65 70 75 80 85 91
No. Licensed RNs
2020
2012
11,787
4,138
42,727
3,546
2,032
568
6,278
513
0
10,000
20,000
30,000
40,000
50,000
CNA LPN RN NP
Male
Female

Future of Oregon’s Nursing Workforce
18
Hispanics are the most under-represented population, with only 3.9 percent of RNs identifying as
Hispanic, while almost 14 percent of the state’s population is Hispanic. Asians and Native
Hawaiians/Pacific Islanders are slightly over-represented (4.0% vs. 3.6%, 0.4% vs. 0.3%, respectively).
CNAs have the most diversity, particularly among Black/African American and Hispanic/Latinx
populations.
Table 4. Racial/ethnic distribution of Oregon nurses by license type.
Race/Ethnicity/Gender CNA LPN RN NP State Pop.
American Indian/Alaska Native 0.9% 0.7% 0.5% 0.3% 1.9%
Asian 5.9% 4.1% 4.1% 3.7% 5.0%
Black/African American 5.9% 4.1% 1.4% 1.8% 2.3%
Hispanic/Latinx 14.7% 7.8% 3.9% 3.7% 14.0%
Native Hawaiian/Pacific Islander 1.0% 0.6% 0.4% 0.3% 0.5%
White (Not Hispanic) 57.0% 68.3% 76.8% 79.3% 74.1%
Multi-Racial 3.5% 3.6% 2.5% 2.1% 4.2%
Other Race 0.5% 0.4% 0.4% 0.5% n/a
Source: OHA Public Use Nursing Workforce Data File, 2020; US Census, 2021. Note: Some nurses do not provide race/ethnicity data and
thus columns may not add to 100%.
Languages spoken by Oregon nurses
Most of Oregon’s nursing workforce speak only English (see Table 5). Spanish is the second most
common language spoken by Oregon nurses, with 6.8 percent of RNs speak Spanish. Spanish was the
most common language spoken, other than English, for CNAs (13.7%), LPNs (7.4%), and NPs (14.4%)
as well. Tagalog and Russian were spoken by about 1.3 percent and 0.8 percent, respectively, by RNs
practicing in Oregon.
Table 5. Languages spoken by license type.
Language spoken
CNA
LPN
RN
NP
English Only 71.5% 82.6% 84.6% 77.4%
American Sign Language 0.5% 0.4% 0.2% 0.0%
Cantonese 0.2% 0.1% 0.2% 0.2%
Korean 0.2% 0.2% 0.3% 0.4%
Mandarin 0.2% 0.2% 0.2% 0.5%
Romanian 0.7% 0.5% 0.5% 0.2%
Russian 1.3% 1.1% 0.8% 0.6%
Spanish 13.7% 7.4% 6.8% 14.4%
Tagalog 3.0% 2.0% 1.3% 0.7%
Vietnamese 0.7% 0.4% 0.7% 0.5%
Source: OHA Public Use Nursing Workforce Data File, 2020. Note: Only languages spoken by at least 100 nurses across license type are
included, thus columns may not add to 100%.

Future of Oregon’s Nursing Workforce
19
Education and Training of nurses in Oregon
Figure 4 maps Oregon’s RN and LPN education programs. Table 6 lists the schools that offer licensed
nurse education and indicates the programs they offer.
Oregon has eight LPN and 17 RN ADN programs offered at community colleges, and six bachelors of
science in nursing (BSN) programs offered at universities. OHSU School of Nursing, the only publicly
funded BSN-level program in Oregon, has five campuses across the state. Three universities have
Accelerated BSN programs where students with other bachelor’s degrees can earn a BSN in a
shortened amount of time. Four universities offer graduate-level education. Only OHSU and the
University of Portland offer DNP or a Doctor of Philosophy (PhD) degrees in nursing.
Figure 4. Locations of Oregon's RN and LPN education programs.
Source: Oregon Center for Nursing, 2022
Five schools offer a pathway for students with an ADN to earn a BSN (RN-to-BSN). OHSU has
partnered with 11 community colleges to form the Oregon Consortium of Nursing Education (OCNE).
These schools use a shared curriculum taught on all campuses, which allows students to take the
same core nursing courses in the first two years of nursing school, regardless of where they attend.
Upon completion, students can then complete the ADN program or continue to a BSN program through
OHSU either in person or online. According to the OCNE website, 6,045 students graduated from the
OCNE curriculum since its inception in 2001 and, as of winter 2021, 1,210 ADN graduates completed
their BSN at OHSU.

Future of Oregon’s Nursing Workforce
20
Table 6. Programs offered by Oregon's RN and LPN education programs.
Source: Oregon Center for Nursing, 2022
Licensed Nurse Program Enrollments and Graduations
The number of registered nursing education programs in Oregon has not changed for more than a
decade. However, the number of students enrolled in programs continues to climb, particularly for BSN
programs. As seen in Figure 5, Oregon enrolls more than twice the number of BSN students as ADN
students. Since 2014, BSN programs have increased enrollment by 42 percent while ADN programs
have decreased enrollment by 15 percent. Data on CNA training program enrollments and graduations
are not available.
Student interest in nursing school remains strong in Oregon. New enrollments in BSN programs have
been growing at a high rate, particularly since 2017 (see Figure 6). Part of the increase in BSN new
enrollments can be attributed to two factors: a new BSN program opening in the Portland area (Warner
Pacific University), and an increase in new student enrollment for another program (University of
Portland School of Nursing) in 2018.

Future of Oregon’s Nursing Workforce
21
Figure 5. Total enrollment in Oregon's RN programs.
Source: OSBN, Nursing Program Annual Report, 2012-2021
Figure 6. New enrollments in Oregon's RN programs.
Source: OSBN, Nursing Program Annual Report, 2012-2021.
Note: The OSBN Nursing Program Annual Report did not collect data for new enrollments in 2020, but resumed this data collection in 2021.
Since there are only eight schools offering LPN courses, and the number of schools has not changed
markedly since 2012, LPN graduates tend to be a small cohort. As seen in Table 7, Oregon’s practical
nursing programs received about 780 applications per year and about 70 percent of applicants were
admitted. About 500 LPN students are enrolled in programs in total.
1,393
1,416
1,454
1,412
1,245
1,238
1,230
1,223
1,313
1,233
1,939
2,015
1,965
2,083
2,043
2,167
2,150
2,350
2,673
2,797
0
500
1000
1500
2000
2500
3000
2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
ADN Programs BSN Programs
746
799
795
771
664
635
673
659
712
847
848
897
898
867
840
1,083
1,166
1,209
0
200
400
600
800
1000
1200
1400
2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
ADN Programs BSN Programs

Future of Oregon’s Nursing Workforce
22
Table 7. Total student enrollment in practical nursing programs.
2012
2014
2016
2018
2020
Enrolled
540
442
501
510
443
Admitted
569
548
538
528
509
Applications
Received
854
791
749
768
627
Acceptance Rate
67%
69%
72%
69%
70%
Source: OSBN, Nursing Program Annual Report, 2012 and 2020
Applications to Oregon’s nursing programs have been declining since a peak in the 2017-2018 school
year (Figure 7). The decrease in applications has been most noticeable in ADN programs. From 2018
to 2021, applications to BSN programs decreased by 12 percent, while applications to ADN programs
decreased by 22 percent.
Figure 7. Numbers of qualified applicants to Oregon RN education programs.
Source: OSBN, Nursing Program Annual Report, 2017-2021
Oregon has a growing number of RN graduates, particularly in BSN level education. As seen in Figure
8, the number of BSN graduates has almost quadrupled in the past 20 years. In contrast, ADN
graduates have remained at a stable level since 2005.
2852
3129
2721
2512
2410
4762
5178
5050
4578
4558
0
1000
2000
3000
4000
5000
6000
2016-2017 2017-2018 2018-2019 2019-2020 2020-2021
ADN Programs BSN Programs

Future of Oregon’s Nursing Workforce
23
Figure 8. Registered nurse graduates over time.
Source: OSBN Annual Surveys of Nursing Education Programs, 2022
Quality of Oregon’s nursing education programs
Oregon’s nursing education programs are exceptionally successful in ensuring their graduates pass
national board examinations and thus qualify for licensure. As seen in Figure 34, the percentage of
graduates who pass the NCLEX-RN the first time they take it is notably higher in Oregon than the
nation. Pass rates have declined somewhat over the past few years; decreases in 2020 and 2021 are
often attributed to the pandemic, which disrupted both nursing education and the examination process.
Figure 9. NCLEX-RN first time pass rate, Oregon vs. U.S.
Source: NCSBN, NCLEX Examination Statistics, 2017-2021
307
412
465
600
595
779
805
747
791
990
1164
387
497
568
594
622
605
591
613
583
565
619
694
909
1033
1194
1217
1384
1396
1360
1374
1555
1783
0
200
400
600
800
1000
1200
1400
1600
1800
2000
2001 2003 2005 2007 2009 2011 2013 2015 2017 2019 2021
BSN graduates ADN graduates Total graduates
89.5%
92.9%
91.5%
90.1%
86.2%
87.1%
88.3%
88.2%
86.6%
82.5%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
2017 2018 2019 2020 2021
Oregon
United States

Future of Oregon’s Nursing Workforce
24
First-time NCLEX-RN pass rates are similar for ADN and BSN program, as seen in Figure 35. Key
informants generally held the view that nursing education at the ADN provides a solid foundation for
entering nursing, Although, they also generally expressed a belief that ADN-educated nurses are more
“task oriented,” have less developed clinical reasoning skills, and are less confident in their clinical
judgement. It was emphasized by many interviewees that ADN-educated nurses are critical to the
nursing workforce in rural and frontier areas of Oregon.
Figure 10. Oregon's NCLEX-RN first time pass rate by program type.
Source: NCSBN, NCLEX Examination Statistics, 2017-2021
Several interviewees emphasized that ADN nursing education is overly focused on the provision of
acute care and recommended curricula incorporate a greater level of exposure to population health and
community-based care models. In contrast, key informants generally expressed the view that nursing
education at the BSN level was doing a good job of preparing new nurses for roles outside of acute
care, including in roles related to population health and community-based care – in particular care for
vulnerable populations. Several key informants noted that BSN programs are in the process of
transitioning away from a focus on specialty care areas and toward the “four spheres of care” model:
prevention/promotion of health and wellbeing, chronic disease care, regenerative (critical/trauma) care,
and hospice/palliative care.
In general, key informants felt pre-license nursing education at both degree levels should place a
greater emphasis on conceptual models and take less of a task-based approach. Curricula need to
emphasize foundational concepts to prepare students to be able to cope with care situations they have
not encountered before. There was also a perception among key informants that pre-license nursing
students are too infrequently exposed to care settings outside of acute care, and in particular they are
critically underexposed to long-term care. One key informant commented that the lack of clinical
exposure to long-term care, and the lack of emphasis on aging and geriatrics, simply reinforces a bias
against working in long-term care settings. Some organizations recognize this challenge. The Oregon
Health Care Association recently received approval to train all community nurses to become certified
geriatric nurses, and is working on developing mentorship opportunities and a support program to
improve recruitment of nurses to long-term care settings.
89.5%
93.2%
90.0%
90.9%
85.8%
89.5%
92.7%
92.8%
89.5%
86.4%
80%
82%
84%
86%
88%
90%
92%
94%
96%
98%
100%
2017 2018 2019 2020 2021
ADN Programs BSN Programs

Future of Oregon’s Nursing Workforce
25
Highest Educational Attainment of Oregon RNs
In the past two decades, national and state campaigns have emphasized the importance of higher
education for nurses. This message has resulted in an increase in the number nurses whose highest
educational level is a BSN or higher degree, and slight decline in the number of nurses with an ADN.
As seen in Table 8, the percentage of nurses with the highest level of education being a master’s
degree or higher has remained stable since 2014.
Table 8. Highest educational attainment of Oregon RNs, 2014-2020.
2014
2016
2018
2020
Less than ADN 5% 5% 5% 3%
ADN 43% 41% 37% 34%
BSN 45% 48% 51% 54%
Master’s or Higher 6% 6% 7% 7%
Source: OHA, Public Use Nursing Workforce Data Files, 2014 - 2020
Demographics of Oregon’s Licensed Nursing Students
A diverse, representative workforce contributes to better health outcomes, satisfaction with health care,
and access to care.
15
However, there continue to be gaps between the representation of Black, Native
American, Hispanic/Latinx, and some Asian subgroups in health care occupations as compared with
the general population.
16
Development of a diverse nursing workforce begins with cultivating students
from diverse backgrounds to enter nursing education programs. The success of this endeavor is
dependent on the capacity of the K-12 education system to support the success of diverse students; a
full exploration of this within Oregon’s elementary and secondary schools was outside the scope of our
study. Nonetheless, attention must be paid to the pipeline of students through the educational system
before they matriculate to nursing education.
Recent graduates from Oregon RN programs are more diverse than nurses in the workforce. For
example, graduates from BSN programs only report about 67 percent white, and ADN graduates report
64 percent white, compared to 77 percent white in the general RN population. While the diversity
among ADN and BSN graduates are similar, more graduates from ADN programs report their race as
“Other/Unknown,” and more BSN graduates report their ethnicity as Asian.
For both enrollments and graduations, and for students in both ADN and BSN programs, the number of
students from Native American, Asian, Pacific Islander, and Black/African American backgrounds were
mostly unchanged from 2012 to present (Table 9). Year over year, however, the number of nursing
students from Hispanic backgrounds continues to grow. This is good news given the disparity between
the number of nurses who identify as Hispanic (3.9%) compared to the general population (14%).
15
US Department of Health and Human Services Advisory Committee on Minority Health. (2011). Reflecting America’s Population:
Diversifying a Competent Health Care Workforce for the 21st Century. Washington, DC: HHS, Office of Minority Health.
16
Taylor, K. J., Ford, L., Allen, E. H., Mitchell, F., Eldridge, M., & Caraveo, C. A. (2022). Improving and Expanding Programs to Support a
Diverse Health Care Workforce: Recommendations for Policy and Practice. Washington, DC: The Urban Institute.

Future of Oregon’s Nursing Workforce
26
Table 9. Enrollment and graduation by race/ethnicity in Oregon's RN programs over time.
ADN Students
BSN Students
Enrolled Graduated Enrolled Graduated
2012
2018
2020
2012
2018
2020
2012
2018
2020
2012
2018
2020
Hispanic 4% 6% 11% 4% 5% 10% 7% 12% 14% 5% 10% 12%
Native American 2% 1% 2% 1% 1% 2% 1% 1% 0% 2% 2% 0%
Asian 4% 3% 5% 4% 2% 4% 7% 11% 13% 7% 8% 8%
Pacific Islander 2% 1% 2% 1% 1% 2% 1% 1% 2% 2% 1% 2%
Black 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1%
White 73% 68% 68% 81% 68% 63% 77% 67% 61% 74% 69% 67%
More Than One
Race
0%
2%
3%
0%
2%
4%
0%
6%
7%
0%
6%
6%
Unknown
16%
18%
9%
7%
20%
13%
6%
3%
2%
9%
3%
3%
Source: OSBN, Nursing Program Annual Report, 2013, 2019, 2021
The racial/ethnic composition of LPN students is more diverse than that of all licensed LPNs.
Enrollment and graduate percentages for LPN students from almost all racial backgrounds grew
noticeably between 2012 and 2020, except for students from Native American or Pacific Islander
backgrounds (see Table 10). While the percentage of LPN students who identify as Native American
remained unchanged over eight years, students who identified as being from Pacific Islander
backgrounds decreased for both enrollments and graduations to less than one percent of LPN students
in Oregon. While the data suggest that practical nursing programs are becoming more diverse, some of
this change could be due to reporting issues, including a marked decrease in the percent of the
students reporting an unknown racial/ethnic identity since 2012.
Table 10. Race/ethnicity of practical nursing students.
Newly Enrolled Graduates
2012 2020 2012 2020
Hispanic 6% 7% 3% 9%
Native American 1% 1% 2% 2%
Asian 4% 7% 3% 8%
Pacific Islander 3% 0% 4% 0%
Black 1% 10% 1% 12%
White 61% 54% 62% 52%
More Than One Race 0% 3% 0% 3%
Unknown 24% 17% 25% 14%
Source: OSBN, Nursing Program Annual Report, 2012 and 2020

Future of Oregon’s Nursing Workforce
27
Most RN graduates are between the ages of 21 and 40 years, as seen in Figure 12. Following national
trends, nurses who graduate from BSN programs are younger than ADN graduates, with more than half
between the ages of 21 and 25. ADN programs have almost 60 percent of their graduates falling
between the ages of 26 and 40.
Figure 11. Graduates by age group in Oregon's RN programs.
Source: OSBN Nursing Program Annual Report, 2019
Students enrolled and graduating from LPN programs tend to be in their 20s. The age distribution of
LPN graduates continued this trend with 50 percent of 2012 graduates and 58 percent of 2018
graduates age 30 years‐of‐age or younger. Very few practical nursing students and graduates were
over the age of 50. Comparable data on age of LPN students was not collected in 2020.
Table 11. Age of practical nursing students and graduates.
Newly Enrolled
Graduates
2012 2018 2012 2018
>20 10% 3% 1% 2%
21-25 27% 32% 26% 29%
26-30 25% 25% 22% 28%
31-40 23% 26% 22% 28%
41-50 13% 11% 15% 12%
51-60 2% 3% 5% 3%
>60 0% 0% 1% 0%
Source: OSBN Nursing Program Annual Report, 2012 and 2020
1.8%
24.6%
28.4%
31.1%
12.0%
2.0%
0.2%
0.0%
53.3%
21.7%
19.5%
4.9%
0.6%
0.0%
0.0%
10.0%
20.0%
30.0%
40.0%
50.0%
60.0%
≤20 21-25 26-30 31-40 41-50 51-60 >60
ADN Programs BSN Programs

Future of Oregon’s Nursing Workforce
28
Licensed Practical Nurse Program Graduations
LPN graduations averaged 393 per year between 2012 and 2020. As presented in Figure 9, there was
a decrease in LPN graduations between 2012 and 2016, followed by an increase between 2016 and
2018. Since 2018, there has been a decrease in LPN graduations.
Figure 12. Graduations from practical nursing programs.
Source: OSBN Annual Surveys of Nursing Education Programs, 2012-2020
534
425
411
367
329
352
400
389
331
0
100
200
300
400
500
600
2012 2013 2014 2015 2016 2017 2018 2019 2020

Future of Oregon’s Nursing Workforce
29
Inter-state migration of nurses
There are two pathways to nurse licensure conducted by OSBN. One is referred to as “licensed via
examination,” which describes RNs who were educated and passed the NCLEX in Oregon. The second
pathway applies to licensed RNs who are practicing in another state. In this process, called “licensed
via endorsement,” OSBN staff verify the applicant has an unencumbered license in another state, has
the required education, and has passed the NCLEX examination. Once these requirements are met,
the applicant can receive an Oregon’s nursing license.
The proportion of RNs licensed via endorsement increased to 60 percent of the workforce for RNs
licensed since 2010 (Figure 13). It appears that the marked growth increase began around this time,
although the reason for this is not known. The rate of growth in the number of licenses obtained via
endorsement shows little sign of abating.
Figure 13. Number of RN licenses approved by year of licensure.
Source: OHA, Public Use Nursing Workforce Data File, 2020
A survey of Oregon nurses licensed by endorsement suggested that about 30 percent of endorsing
nurses were currently practicing in Oregon and another 11 percent lived in Oregon while practicing in
another state, namely California, Idaho, and Washington.
17
Thus, about 40 percent of endorsing RNs
were available to practice in Oregon based on their state of residence. More recent data from the OHA
indicate that 35 percent of RNs licensed by endorsement were practicing in Oregon (Figure 14).
17
Oregon Center for Nursing, Survey of Endorsing Nurses, November 2017.
4064
1462
0
500
1000
1500
2000
2500
3000
3500
4000
4500
1980
1981
1982
1983
1984
1985
1986
1987
1988
1989
1990
1991
1992
1993
1994
1995
1996
1997
1998
1999
2000
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
Endorsement
Examination

Future of Oregon’s Nursing Workforce
30
Figure 14. Percent of RNs practicing in Oregon by method of licensure.
Source: OHA, Public Use Nursing Workforce Data File, 2020
Studies by OCN have shown the nurses who obtain their license by endorsement and practice within
the state generally practice in Oregon’s small, rural communities, often in non-hospital settings. A
decrease in the number of nurses migrating from other states and practicing in Oregon would likely
impact small counties the most.
International recruitment and immigration
There is very little data about international recruitment and immigration of foreign-educated nurses.
According to the OHA Nursing Public Use File from 2020, 50 LPNs and 1,385 RNs identified
themselves as foreign educated, accounting for less than one percent of LPNs and only 2.3 percent of
RNs.
Foreign-educated nurses must complete an established re-entry program before they can be licensed
to work in Oregon. Oregon has two re-entry programs recognized by OSBN. One of these programs,
the Immigrant Nurse Credential (INC), is designed to help foreign-educated nurses pass the
requirements to become a registered nurse in Oregon.
There is no data about how many foreign-educated nurses have immigrated to Oregon. Between 2018
and 2020, the INC program graduated 30 participants, and currently have about 19 foreign-educated
nurses on a waitlist for the next cohort of the program.
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
Endorsement Examination
Practicing in OR
Not Practicing in OR
Future of Oregon’s Nursing Workforce
31
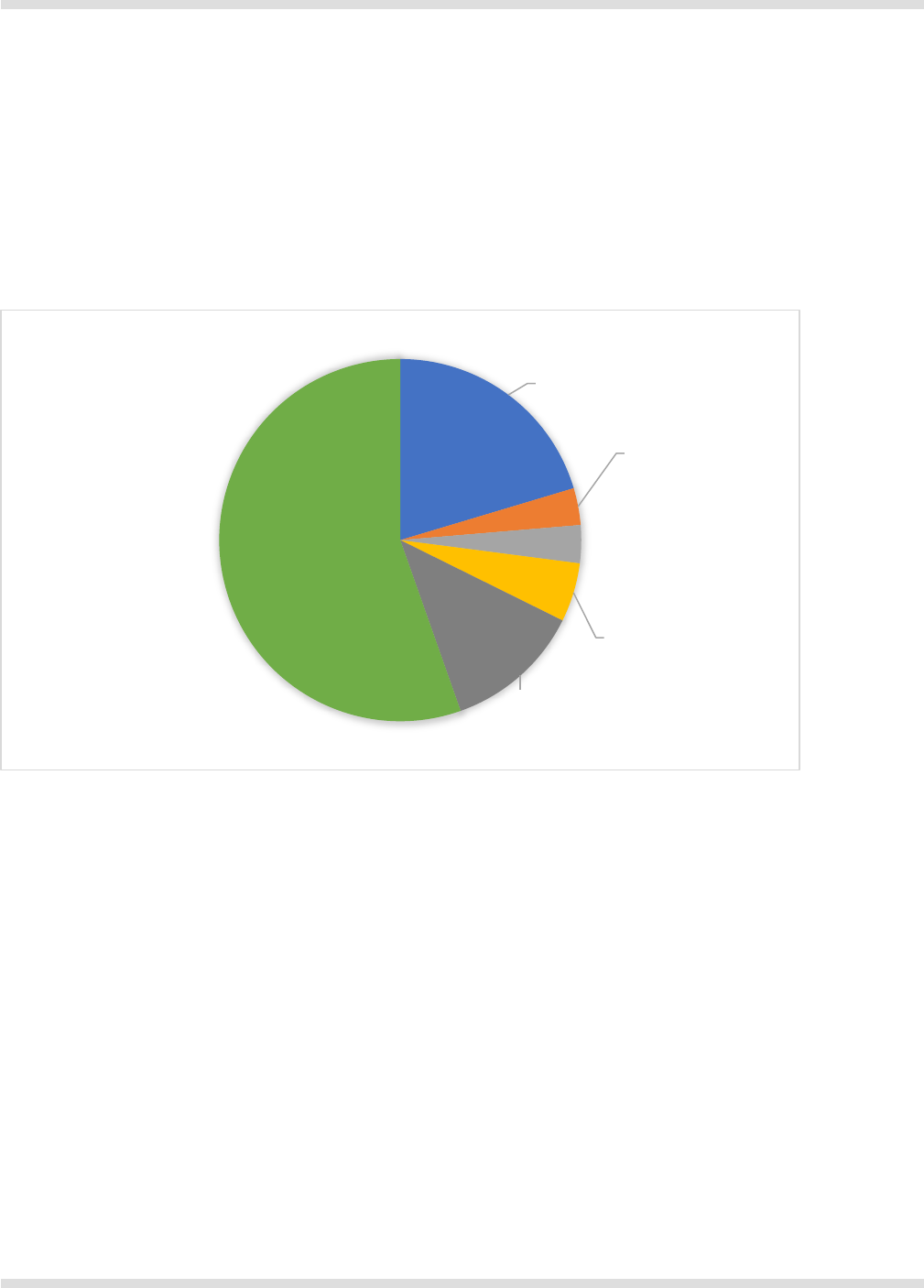
Patterns of Nurse Employment
As seen in Figure 15, the majority of Oregon’s licensed RNs practice in a hospital setting. In 2020, 55
percent of RNs worked in hospitals, which is the most common setting. Office/clinic settings was the
second most common setting, but only 12 percent of RNs reported practicing in this setting. National
data show similar findings. According to the Bureau of Labor Statistics, about 60 percent of RNs
worked in a hospital during 2020. The “Other Practice Setting” category includes nurses in public
health, K-12 education, policy, education, and regulation.
Figure 15. Practice settings of Oregon RNs.
Source: OHA, Public Use Nursing Workforce Data File, 2020
Compensation of nurses
Most of the data presented in this section are derived from the 2018 National Sample Survey
Registered Nurses (NSSRN). These data allow for analysis of the differences in RN compensation
associated with employment status, highest level of education, years of experience, and practice
setting. Figure 16 compares the 2018 median annual income for all nursing employment earned by
nurses employed in Oregon with the national average, for both full-time and part-time employment. The
median annual income for Oregon nurses who worked full-time was $14,000 (or 19%) greater than the
national average. Among those who reported part-time employment, the median annual income for
Oregon nurses was $23,000 (or 55%) greater than the national average.
Other Practice
Setting
20%
Ambulatory
Surgical Center
3%
Skilled Nursing
Facility/Long Term
Care
4%
Home
Health/Hospice
5%
Office/Clinic
12%
Hospital
56%

Future of Oregon’s Nursing Workforce
32
Figure 16. Median income from all nursing employment by full-time/part-time status, Oregon vs.
U.S., 2018.
Source: NSSRN, 2018
Note: U.S. median excludes Oregon. Data includes all nurses regardless of employment setting or advanced practice status.
Figure 17 replicates the comparison shown in Figure 16, but the data are limited to those employed as
a NP. In 2018, the median annual income earned by full-time NPs in Oregon was $12,000 (or 11%)
greater than the national average. Among those employed part-time, the difference in median annual
income was much smaller: part-time NPs in Oregon earned just $3,800 (or 6%) more.
Figure 17. Nursing practitioner median income from all nursing employment by full-time/part-
time status, Oregon vs. U.S., 2018.
Source: NSSRN, 2018
Note: U.S. median excludes Oregon.
Figure 18 compares the 2018 median annual income from all nursing employment earned by full-time
nurses in Oregon, based on their highest level of education in any field. These data show additional
education correlates with higher earnings. Nurses with a bachelor’s degree earned, on average, $9,000
$89,000
$65,000
$75,000
$42,000
$0
$20,000
$40,000
$60,000
$80,000
$100,000
Full-time Part-time
Oregon United States
$118,000
$70,000
$106,000
$66,200
$0
$50,000
$100,000
$150,000
Full-time Part-time
Oregon United States

Future of Oregon’s Nursing Workforce
33
(or 11%) more than nurses with an associate degree. The data indicate a smaller increase in earnings,
comparing those with a bachelor’s degree to those with a master’s degree. The largest increase in
earnings was associated with possession of a doctoral degree. Annual median earnings for nurses with
a doctoral degree earned was $25,000 to $39,000 more than nurses holding less advanced degrees.
Figure 18. Full-time median income from all nursing employment, by highest level of education,
Oregon, 2018.
Source: NSSRN, 2018
Note: These data describe highest level of education in any field, and include all nurses regardless of employment setting or advanced
practice status.
Figure 19 compares the 2018 annual median income from all nursing employment earned by full-time
nurses in Oregon, based on their years of nursing experience. These data demonstrate earnings
generally increase with more years of nursing experience, up to a point, after which earnings level off.
The biggest relative increases in earnings occur in the first 10 years of nursing employment. Annual
earnings for full-time nurses with 6 to 10 years of experience were, on average, $9,000 (or 12%) more
than nurses with five or fewer years of nursing experience.
Figure 19. Full-time median income from all nursing employment, by nursing experience,
Oregon, 2018.
Source: NSSRN, 2018
Note: These data include all nurses regardless of employment setting or advanced practice status.
$81,000
$90,000
$95,000
$120,000
$0
$50,000
$100,000
$150,000
Associate degree Bachelor's degree Master's degree Doctorate
$76,000
$87,000
$90,000
$94,000
$97,000
$102,000 $102,000
$100,000 $100,000
$0
$20,000
$40,000
$60,000
$80,000
$100,000
$120,000
Less than
6 years
6 - 10
years
11 - 15
years
16 - 20
years
21 - 25
years
26 - 30
years
31 - 35
years
36 - 40
years
More
than 40
years

Future of Oregon’s Nursing Workforce
34
Figure 20 compares the 2018 annual median income from all nursing employment earned by full-time
nurses in Oregon, based on their employment setting. Nurses’ employment settings have been grouped
into four categories: Hospitals, other (non-hospital) inpatient settings, clinics and other ambulatory care
settings, and then all other employment settings. Table 12 details the different employment settings that
the 2018 NSSRN have been grouped together into these four broad categories. On average, earnings
for nurses employed in a hospital setting were higher by comparison with all other settings. This
earnings difference ranged from $5,000 to $13,000 annually.
Figure 20. Annual median income from all nursing employment earned by full-time RNs, by
employment setting, 2018.
Source: NSSRN, 2018
Note: These data include all nurses regardless of advanced practice status.
Table 12. Detailed description of employment settings used in the NSSRN, 2018.
Category
Detailed Employment Settings
Hospital
Critical Access Hospital, Inpatient Unit, Emergency Department, Hospital
Ancillary Unit, Hospital Nursing Home Unit, Hospital Administration
Other Inpatient
Non-hospital Nursing Home Unit, Rehabilitation Facility/Long-term Care,
Inpatient Mental Health, Correctional Facility
Clinic/Ambulatory
Nurse-managed Health Center, Private Medical Practice, Public Clinic
(FQHC, Tribal, Rural), School Health Service, Outpatient Mental
Health/Substance Abuse, Ambulatory Surgery Center (free-standing)
Other Setting
Home Health, Occupational Health/Employee Health Service,
Public/Community Health Agency (non-clinic), Other Government Agency,
Outpatient Dialysis Center, Academic Institution, Case
Management/Disease Management/Insurance Company, Call Center
$93,000
$80,000
$82,000
$88,000
$0
$20,000
$40,000
$60,000
$80,000
$100,000
Hospital Other inpatient Clinic/Ambulatory Other setting
Future of Oregon’s Nursing Workforce
35
Table 13 compares the 2022 estimated median hourly wage earned by RNs, NPs, LPNs, and nursing
assistants across different geographic regions of Oregon. These data highlight the substantial
difference in earnings by type of nursing practice. On average, NPs earned approximately $14 per hour
more than RNs, RNs earned approximately $19 per hour more than LPNs, and LPNs earned
approximately $11 per hour more than nursing assistants. Table 13 also indicates the highest paid
nurses, across all three occupations, were employed in the Portland Metro area, and the regional wage
differential was greatest among NPs. The estimated hourly wage difference between the highest paid
NPs (Portland Metro) and lowest paid NPs (Southwestern Oregon and Eastern Oregon) was
approximately $4.39 per hour (or an estimated $9,131 annually for full-time employment). The
difference between the highest paid RNs (Portland Metro) and lowest paid RNs (Rogue Valley and
Eastern Oregon) was $3.42 per hour (or an estimated $7,114 annually for full-time employment). The
difference between the highest paid LPNs (Portland Metro) and lowest paid LPNs (Southwestern
Oregon and Eastern Oregon) was $1.46 per hour (or an estimated $3,037 annually for full-time
employment). The difference between the highest paid nursing assistants (Portland Metro) and lowest
paid nursing assistants (Eastern Oregon) was $1.20 per hour (or an estimated $2,496 annually for full-
time employment).
Table 13. Median hourly wage by region and occupation, 2022.
Region
Registered
Nurse
Nurse
Practitioner
Licensed
Practical/Vocational
Nurse
Nursing
Assistant
Oregon $49.52 $63.60 $30.00 $19.20
East Cascades $49.15 $62.81 $29.58 $18.75
Eastern Oregon $47.17 $60.32 $29.26 $18.30
Lane $49.20 $63.85 $29.45 $19.01
Mid-Valley $48.83 $63.93 $29.98 $19.03
Northwest Oregon $47.90 $63.28 $29.29 $19.04
Portland Metro $50.59 $64.66 $30.72 $19.50
Clackamas $49.98 $64.66 $30.46 $19.18
Rogue Valley $47.17 $63.69 $29.31 $19.01
Southwestern
Oregon
$48.49 $60.27 $29.26 $18.62
Source: Oregon Employment Department, 2022 Oregon Wage Information, June 17, 2022

Future of Oregon’s Nursing Workforce
36
Current Challenges for the Nursing Workforce
The national context
During the COVID-19 pandemic, there were severe disruptions in health care delivery and employment.
Data prior to the pandemic suggested the nation was graduating enough new nurses to replace retiring
nurses, although there was some debate about whether a small shortage or surplus of nurses might
arise in the future.
18
There was consensus about notable differences across regions of the U.S.
19
and
even within states.
20
Prior research has found rural regions and safety-net employers are more likely to
report shortages of nurses than other regions and employers.
21,22
Prior to the pandemic, western states
had lower RN supply than other regions of the country,
19
but the relatively low supply might have
reflected lower demand for nurses due to healthier populations and more efficient health care systems.
When shortages of RNs were reported, they were often for specialty fields such as emergency,
intensive care, labor/delivery, and peri-operative care.
23
Several studies have examined changes in the nursing labor market after the COVID-19 pandemic
reached the U.S. in early 2020. National studies of health care employment have reported some
transient and persistent changes. All health care industry sectors experienced decreases in
employment in the second quarter of 2020.
24
Turnover of health care workers was notably higher from
April through December 2020 than it had been prior to the pandemic.
25
Between mid-2020 and mid-
2021, employment returned to pre-pandemic levels except for skilled nursing facilities, which have
faced a persistent decrease in employment.
24
In addition, turnover rates returned to pre-pandemic
levels in 2021, except for in skilled nursing facilities which have had rising turnover rates.
25
As for all health care workers, nursing also experienced transient and persistent changes. Specifically
nursing employment decreased in all health care sectors starting in the second quarter of 2020 and
then gradually recovered to near-pandemic levels by late 2021, except for in nursing homes where
there has been a continuous decline in nursing employment.
26
When the data are disaggregated to look
at RNs, LPNs, and CNAs separately, they reveal that employment has fully recovered for RNs, but LPN
and CNA employment has remained below pre-pandemic levels. Analysis of turnover data finds that
turnover increased for all nursing categories in the first nine months of the pandemic and recovered for
18
Spetz, J. (2015). Too many, too few, or just right? Making sense of conflicting RN supply and demand forecasts. Nursing Economics, 33(3),
176-179.
19
Auerbach, D. I., & Staiger, D. O. (2017). How fast will the registered nurse workforce grow through 2030? Projections in nine regions of the
country. Nursing Outlook, 65(1), 116-122.
20
Spetz, J. (2018). Forecasts of the Registered Nurse Workforce in the Central Coast Region of California. Oakland, CA: HealthImpact.
21
Spetz, J. & Quan, A. (2021). Innovation Landscape — Solving Shortages: How Technology Can Help Meet California’s Immediate Health
Workforce Needs. Oakland, CA: California Health Care Foundation.
22
Seago, J. A., Ash, M., Spetz, J., Coffman, J., & Grumbach, K. (2001). Hospital registered nurse shortages: environmental, patient, and
institutional predictors. Health Services Research, 36(5), 831.
23
Chu, L. & Spetz, J. (2020). Survey of Nurse Employers in California, Fall/Winter 2018-19. San Francisco, CA: Healthforce Center at UCSF.
April 2020
24
Cantor, J., Whaley, C., Simon, K., & Nguyen, T. (2022). US Health Care Workforce Changes During the First and Second Years of the
COVID-19 Pandemic. JAMA Health Forum, 3(2): e215217.
25
Frogner, B. K., & Dill, J. S. (2022). Tracking turnover among health care workers during the COVID-19 pandemic: a cross-sectional study.
JAMA Health Forum, 3 (4): e220371.
26
Buerhaus, P. I., Staiger, D. O., Auerbach, D. I., Yates, M. C., & Donelan, K. (2022). Nurse Employment During The First Fifteen Months Of
The COVID-19 Pandemic: Study examines nurse employment trends during first fifteen months of the COVID-19 pandemic. Health Affairs,
41(1), 79-85.

Future of Oregon’s Nursing Workforce
37
RNs and CNAs. However, turnover for LPNs continued to increase through the first nine months of
2021.
25
The unemployment rate for RNs was somewhat above pre-pandemic levels in the second
quarter of 2021, notably higher for CNAs, and no different for LPNs.
26
Together, declining employment
numbers and stable unemployment rates for LPNs suggest many LPNs left the labor market and are no
longer working or seeking work in the profession.
Nursing shortages
Nursing shortages arise when employers are unable to hire nurses at prevailing wages to achieve the
level of employment they desire. Economic theory indicates this imbalance in labor supply and demand
should be short-lived, with wages rapidly adjusting to attract a greater supply of labor. However,
recurrent shortages of RNs have been reported for decades.
27
Researchers have proposed a few
reasons this might be the case, including slow wage increases due to constrained employer budgets,
delays in producing new nurses due to education and licensure requirements, and market power held
by large employers, particularly in small markets where there may be only a few employers.
28,29
There is no objective measure of whether a labor shortage exists. Rising vacancy rates can suggest a
shortage, but vacancies also could rise when there is a transient or sudden change in demand such as
when a new hospital building is constructed or there is a particularly bad flu season. Vacancies also
could be posted, but employers might not be actively seeking to fill the vacant positions. Data on the
average length of time required to fill a vacant position can be illuminating, but are rarely collected.
Finally, surveys of employers can provide some indication of the presence of shortages, although
survey responses may be biased. Research on these different indicators of nursing shortages generally
find them to be highly correlated with each other.
27
Debates about whether a statewide labor shortage exists and how severe it is overlook other important
dimensions of labor shortages, particularly for nursing. Geographic maldistribution, imbalances in the
skills and experience desired by employers and the labor supply available, and concerns about quality
of care require at least as much attention as general shortages.
Key informants interviewed expressed mixed views in characterizing concerns about nursing workforce
shortages prior to the pandemic. Some reported no concerns, others described nursing workforce
shortage as manageable, while a few emphasized their health care systems had been under stress
from the lack of available nursing staff for years prior to the pandemic. However, the experience of the
COVID-19 pandemic was uniformly characterized by key informants as having created demand for
nursing staff that could not be met by the available supply, even with the emergency actions taken by
the state to allow out-of-state nurses to practice in Oregon. Interviewees confirmed a shortage of
nurses of all types (RNs, LPNs, and nursing assistants) continues to be an issue for health care
systems across the state. One interviewee, who represented a large health care system in rural
Oregon, emphasized health care workforce shortages are not limited to nursing, but encompass a
broad range of occupations, both patient care-facing, technical, and ancillary support staff.
27
Grumbach, K., Ash, M., Seago, J. A., Spetz, J., & Coffman, J. (2001). Measuring shortages of hospital nurses: How do you know a hospital
with a nursing shortage when you see one?. Medical Care Research and Review, 58(4), 387-403.
28
Yett, D. E. (1975). An economic analysis of the nurse shortage (Vol. 1). Lexington, MA: Lexington Books.
29
Buerhaus, P. I. (1991). Dynamic shortages of registered nurses. Nursing Economics, 9(5), 317-328.

Future of Oregon’s Nursing Workforce
38
The causes of the shortage of nursing staff are difficult to precisely determine. Several interviewees
acknowledged having lost staff nurses as a result of COVID-19 vaccine mandates; others referenced
employers that were more accommodative of vaccine exemptions and expressed the view that a
willingness to accommodate may have helped retain staff and even attract new employees. However, it
is likely a much more important factor driving the current shortage of nursing staff affecting health care
systems across the state is simply the impact of the pandemic itself. There is reason to believe the
negative experience of having been a direct care nurse through the pandemic, especially one who was
employed in an acute care setting, is contributing to nurses opting for early retirement, to seek
opportunities to work as a traveler nurse and dramatically reduce the number of hours worked, to shift
care settings away from acute care or away from patient care, or simply leave the health care workforce
entirely.
Ramifications of nursing shortages on organization operations and new graduate onboarding
Interviewees provided multiple examples of ramifications stemming from an ongoing shortage of
nursing and health care facility staff. Several key informants emphasized daily operations at their
hospitals have been severely challenged: patient diversions are increasing; holding patients in the
emergency department for longer than needed while waiting for a bed or opportunity to transfer is
increasingly common; taking beds offline is more common, as is flexing the number of beds depending
on the availability of staff on a given shift. It is important to underscore that staff shortages are not
isolated to nursing. For some health care systems, they entail a wide range of occupations in direct
patient care, in laboratory and technical positions, and in critical support positions (e.g. housekeeping,
food service). Many of the interviewees acknowledged the burden of being consistently short-staffed is
negatively affecting staff morale.
In addition to their impact on patient care and staff morale, key informants noted nurse staffing
shortfalls have limited the capacity of health care systems to provide clinical placements for nursing
students. A factor contributing to this is a lack of nurses available to precept students because they are
needed to cover shifts in other areas. The effect of having limited access to clinical rotations means
new graduate nurses are entering the workforce with less confidence in their clinical skills and
reasoning, but employers need to them to fill positions left open by a lack of experienced nurses,
including areas of clinical specialty care. Several interviewees expressed concern that specialty care
units may become over-saturated with inexperienced nurses, which in turn contributes to staffing
challenges.
Nurse vacancies
Data from the American Hospital Association’s Annual Survey of Hospitals provided information about
hospital vacancy rates in 2019 for Oregon and other states. As seen in Table 14, on average, Oregon
hospitals reported lower vacancy rates for RNs and nursing aides than other states but slightly higher
vacancy rates for LPNs. Note that the vast majority of hospitals in Oregon and more than half of
hospitals in other states reported no LPN vacancies; thus, the average vacancy rates represent the
situation in only a few hospitals.
Table 14. Hospital vacancies in Oregon and other states, 2019.

Future of Oregon’s Nursing Workforce
39
RNs –
Oregon
RNs –
Other states
LPNs –
Oregon
LPNs –
Other states
Aides –
Oregon
Aides –
Other states
Average 8.3% 9.8% 10.3% 10.1% 8.0% 11.8%
25th percentile 3.0% 2.9% 0.0% 0.0% 0.0% 0.0%
50th percentile 6.3% 7.4% 0.0% 0.0% 1.8% 7.3%
75th percentile 11.1% 13.0% 0.0% 10.0% 12.2% 16.1%
Source: American Hospital Association, 2019
Note: Rates computed as number of vacancies divided by number of FTEs. Some vacancies might be for part-time positions and thus these
calculated vacancy rates are likely to be higher than the actual vacancy rate.
According to the Oregon Employment Department 2021 Job Vacancy Survey, across the entire state,
RNs had the seventh most open positions (2,099) among 432 different occupations. Seventy-six
percent of those openings were full-time positions and 76 percent were considered “difficult to fill” by
employers. Approximately 40 percent of those open RN positions had been vacant for 60 days or more
at the time of the survey. At the regional level, RN was in the top ten occupations with the most total
vacancies and largest share of vacancies considered “difficult to fill” in five of the nine different regions
for which vacancy data were reported.
This same survey reported nursing assistants had the sixth most open positions (2,540) across the
state. Seventy-seven percent of those openings were full-time positions and 87 percent were
considered “difficult to fill” by employers. Thirty percent of those open nursing assistant positions had
been vacant for 60 days or more at the time of the survey. At the regional level, nursing assistant was
in the top ten occupations with the most total vacancies and largest share of vacancies considered
“difficult to fill” in seven of the nine different regions for which vacancy data were reported.
At the state level, LPN was not among the occupations with either the most total vacancies, nor
vacancies considered “difficult to fill”. However, LPNs were among the top ten occupations, in terms of
the most vacancies, in the Mid-Valley region (Linn, Marion, Polk, and Yamhill counties), although not
among the occupations with the most vacancies considered “difficult to fill”.
Vacancies and difficulty recruiting nurses varies across employment settings. Key informants reported
that, in some regions, hospitals have sought to fill RN vacancies by hiring LPNs, which led to more LPN
vacancies in long-term care settings. Similarly, some employers may have increased their demand for
CNAs to relieve RN and LPN workload, which may have led to more difficulty recruiting CNAs in other
settings.
Retention of Nurses in Oregon
Data from the 2018 NSSRN describing changes in nurses’ employment status are presented below.
Although employment conditions have likely changed in dramatic ways in the past two years, these
data provide some context for understanding nursing workforce retention in Oregon prior to the
experience of the pandemic. Figure 21 indicates that Oregon had a much higher retention rate of
nursing employment than the national average. Approximately 97 percent of RNs who reported being
employed in nursing, also reported they had been employed in nursing in the prior year. This is 11
percentage points greater than the U.S. average.

Future of Oregon’s Nursing Workforce
40
Figure 21. Percentage of RNs employed who were also employed in nursing one year before,
Oregon vs United States, 2018.
Source: NSSRN, 2018
Note: U.S. data excludes Oregon. Data include all nurses regardless of employment setting or advanced practice status.
Figure 22 shows that 96 percent of the RNs who reported being employed in nursing, in the state of
Oregon, also reported they had been employed in nursing in Oregon in the prior year. Approximately
four percent of Oregon’s RNs were employed in nursing in a different state in the prior year. These
proportions are comparable to national averages.
Figure 22. Change in Nursing Employment Location from Prior Year, Oregon vs United States,
2018.
Source: NSSRN, 2018
Note: U.S. data excludes Oregon. Data include all nurses who reported employment in both current and prior year, regardless of employment
setting or advanced practice status.
Figure 23 shows that nursing employers in Oregon had a comparable retention rate of their RN
workforce to the national average. Approximately 90 percent of RNs in Oregon were employed with the
96.8%
83.6%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Oregon United States
96.2%
97.0%
3.8%
3.0%
0%
20%
40%
60%
80%
100%
Oregon United States
Employed in same state Employed in different state

Future of Oregon’s Nursing Workforce
41
same employer compared to the prior year (85% in the same nursing position); the U.S. average was
approximately 89 percent.
Figure 23. Change in nursing position and employer from prior year, Oregon vs. U.S., 2018.
Source: NSSRN, 2018
Note: U.S. data excludes Oregon. Data include all nurses who reported employment in both current and prior year, regardless of employment
setting or advanced practice status.
Figure 24 compares changes in employment status among Oregon’s RN workforce with the rest of the
U.S. These data indicate that Oregon had a higher than average share of RNs working part-time in
nursing. Approximately 26 percent of Oregon’s RNs reported part-time nursing employment in both the
survey year and the year prior; across all other states, an average of 16 percent of RNs reported part-
time nursing employment in both years. The data in Figure 24 also show most RNs in Oregon and
across the U.S. maintained their nursing employment status, whether staying in full-time or part-time
positions. Approximately eight percent of RNs in Oregon, and an average of seven percent of RNs
across all other states, reported a change in their full-time or part-time nursing employment status.
Figure 24. Change in nursing employment status from prior year, Oregon vs. U.S., 2018.
Source: NSSRN, 2018
Note: U.S. data excludes Oregon. Data include all nurses who reported employment in both current and prior year, regardless of employment
setting or advanced practice status.
84.6%
82.5%
5.5%
6.2%
9.9%
11.2%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Oregon United States
Different position w/ different
employer
Different position w/ same employer
Same position & employer
65.7%
77.1%
2.5%
2.3%
5.2%
4.6%
26.6%
16.0%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Oregon United States
Part-time to Part-time
Part-time to Full-time
Full-time to Part-time
Full-time to Full-time

Future of Oregon’s Nursing Workforce
42
Nurse workloads
The importance of nurse workload
Across care settings, higher nurse-to-patient ratios are associated with better patient outcomes.
Multiple systematic literature reviews have reported positive relationships between RN staffing and
patient outcomes.
30,31
Patients on units that have periods of “understaffing” relative to what patient
acuity requires have higher risk of negative outcomes.
32,33,34,35,36
However, no study points to a single
“optimal” staffing model. Rigorous studies have found there are diminishing returns to increased nurse
staffing, and some studies suggest adding more nurses may be detrimental after some point.
37,38
The lack of consensus about ideal nurse staffing is likely due to there being other nursing-related
factors that affect patient outcomes. First, individual nurse productivity varies based on their
experience, education, and other unmeasured attributes; this variability has been linked to patient
outcomes.
39
Second, the work environment in which nurses practice can influence patient outcomes.
Positive nurse work environments have positive effects on patient outcomes and satisfaction,
40
although there is some ambiguity regarding the strength of the relationship.
41
For example, research on
organizational safety culture has not found consistent significant relationships with patient safety and
quality of care.
42
Some research suggests that investments in nurse work environment and workload might save money
for health care organizations. Higher staffing is associated with fewer patient complications, and fewer
30
Kane, R. L., Shamliyan, T. A., Mueller, C., Duval, S., & Wilt, T. J. (2007). The association of registered nurse staffing levels and patient
outcomes: systematic review and meta-analysis. Medical Care, 1195-1204.
31
Blume, K. S., Dietermann, K., Kirchner‐Heklau, U., Winter, V., Fleischer, S., Kreidl, L. M., Meyer, G., & Schreyögg, J. (2021). Staffing levels
and nursing‐sensitive patient outcomes: Umbrella review and qualitative study. Health Services Research, 56(5), 885-907.
32
Needleman, J., Buerhaus, P., Pankratz, V. S., Leibson, C. L., Stevens, S. R., & Harris, M. (2011). Nurse staffing and inpatient hospital
mortality. New England Journal of Medicine, 364(11), 1037-1045.
33
Shang, J., Needleman, J., Liu, J., Larson, E., & Stone, P. W. (2019). Nurse Staffing and Healthcare Associated Infection, Unit-level
Analysis. The Journal of Nursing Administration, 49(5), 260.
34
Rochefort, C. M., Beauchamp, M. E., Audet, L. A., Abrahamowicz, M., & Bourgault, P. (2020). Associations of 4 nurse staffing practices with
hospital mortality. Medical Care, 58(10), 912.
35
Griffiths, P., Maruotti, A., Saucedo, A. R., Redfern, O. C., Ball, J. E., Briggs, J., Dall'Ora, C., Schmidt, P. E. & Smith, G. B. (2019). Nurse
staffing, nursing assistants and hospital mortality: retrospective longitudinal cohort study. BMJ Quality & Safety, 28(8), 609-617.
36
Needleman, J., Liu, J., Shang, J., Larson, E. L., & Stone, P. W. (2020). Association of registered nurse and nursing support staffing with
inpatient hospital mortality. BMJ Quality & Safety, 29(1), 10-18.
37
Yakusheva, O., Bang, J. T., Hughes, R. G., Bobay, K. L., Costa, L., & Weiss, M. E. (2022). Nonlinear association of nurse staffing and
readmissions uncovered in machine learning analysis. Health Services Research, 57(2), 311-321.
38
Blegen, M. A., Goode, C. J., & Reed, L. (1998). Nurse staffing and patient outcomes. Nursing Research, 47(1), 43-50.
39
Yakusheva, et al., 2019, Medical Care
40
Lake, E. T., Sanders, J., Duan, R., Riman, K. A., Schoenauer, K. M., & Chen, Y. (2019). A meta-analysis of the associations between the
nurse work environment in hospitals and 4 sets of outcomes. Medical Care, 57(5), 353.
41
Lee, S. E., & Scott, L. D. (2018). Hospital nurses’ work environment characteristics and patient safety outcomes: A literature review.
Western Journal of Nursing Research, 40(1), 121-145.
42
Lee, S. E., Scott, L. D., Dahinten, V. S., Vincent, C., Lopez, K. D., & Park, C. G. (2019). Safety culture, patient safety, and quality of care
outcomes: a literature review. Western Journal of Nursing Research, 41(2), 279-304.

Future of Oregon’s Nursing Workforce
43
patient complications may produce lower net costs.
43,44,45
Moreover, it was suggested in interviews that
shortages of support staff result in RNs being less able to practice using all of the knowledge and skills
they possess.
Nurse workload in Oregon
The American Hospital Association Annual Survey of Hospitals provides data on full-time equivalent
employment of RNs, LPNs, and aides. We divided these figures by the number of adjusted patient days
to obtain a standardized measure of nurse staffing. As seen in Table 15, average RN staffing in Oregon
is higher than in other states, but average LPN and aide staffing are lower. Median RN and aide staffing
are higher in Oregon than other states, and median LPN staffing is lower. Note that these comparisons
do not account for the possibility that hospitalized patients in Oregon are more acutely ill than the
national average, and thus Oregon’s patient care needs may warrant higher staffing levels.
In interviews, key informants held mixed views about the workload of nurses prior to the COVID-19
pandemic. Some described it as having been balanced and generally manageable, but others reported
unfilled nursing positions were already causing workload stress. The pandemic changed conditions for
nurses dramatically, particularly for those working in acute care settings. The intensity of patients’ care
needs was much greater and there weren’t enough nurses to meet those needs, despite shifting nurses
from other units to deal with the influx of COVID-related admissions. Moreover, hospitals needed to
open new units to accommodate the influx of patients, adding volume to the intensity of the workload.
Table 15. Hospital full-time equivalent employment per 1000 adjusted patient days, 2019.
RNs –
Oregon
RNs –
Other states
LPNs –
Oregon
LPNs –
Other states
Aides –
Oregon
Aides –
Other states
Average 5.21 4.74 0.21 0.62 1.41 1.74
25th percentile 3.83 1.99 <0.01 0.08 0.66 0.64
50th percentile 4.90 3.45 0.05 0.21 1.09 1.06
75th percentile 5.82 4.88 0.14 0.47 1.67 1.59
Source: American Hospital Association, 2019
Note: Adjusted patient days are adjusted to account for ancillary and ambulatory services
43
Needleman, J., Buerhaus, P. I., Stewart, M., Zelevinsky, K., & Mattke, S. (2006). Nurse staffing in hospitals: is there a business case for
quality?. Health Affairs, 25(1), 204-211.
44
Martsolf, G. R., Auerbach, D., Benevent, R., Stocks, C., Jiang, J., Pearson, M. L., ... & Gibson, T. B. (2014). Examining the value of inpatient
nurse staffing: an assessment of quality and patient care costs. Medical Care, 982-988.
45
Lasater, K. B., Aiken, L. H., Sloane, D. M., French, R., Martin, B., Reneau, K., Alexander, M. & McHugh, M. D. (2021). Chronic hospital
nurse understaffing meets COVID-19: an observational study. BMJ Quality & Safety, 30(8), 639-647.

Future of Oregon’s Nursing Workforce
44
During the pandemic, hospitals had to rely on unprecedented numbers of traveler nurses who were
often unfamiliar with many operational aspects of the units in which they were working. At the same
time, some hospital leaders indicated they had traveler RNs who had previously been employed by the
same hospital or another hospital in the same system. When traveling nurses are new to an
organization, it creates an additional burden for hospital-employed staff to have to train and support
traveler nurses. Over the past two years, the sheer volume of travelers contributed to a sense of
instability. Beyond the intensity of providing patient care, nurses with families experienced challenges
outside of work related to school closures and childcare-related needs. Some hospitals reported their
staff nurses leaving positions to work as travelers, taking advantage of the opportunity to make
considerably more money. This added to the workload of nurses who remained on staff. Finally, key
informants emphasized that nursing workload continues to be an issue, given the “crisis level” shortage
of available nursing to staff to fill open positions. In addition, they emphasized that the shortage is not
confined to RNs, in some parts of Oregon there is acute shortage of nursing assistants.
46
Responses to deal with increased workload
Key informants provided several examples of hospital efforts to manage the increased workload of
nurses. One interviewee described placing an experienced nurse in every unit of the hospital, free of
patient assignments, so that experienced nurses can focus on supporting other nurses on the unit. The
experienced nurse reviews nursing care plans, helps prioritize patients, consults on patients with
complex care needs, and makes sure nurses get their breaks. Another interviewee referenced taking a
new approach to admissions and discharges, where specialized teams were created to handle all of
these functions in order to free up nursing staff to focus only on providing direct care to patients.
Hospitals set up external COVID-19 testing sites to reduce the burden placed on emergency
departments, which have been a primary site for patients who wanted COVID-19 testing. Finally, one
interviewee reported their health care system had implemented a pilot program for “virtual nurses” who
can be available to support multiple units remotely. This program was described as a way to not only
reduce workload and address staff shortages but also retain experienced nurses at the end of their
career (i.e., nurses who no longer want to practice bedside care and may be ready to retire).
Regulatory approaches to manage nurse workloads
There are four general approaches states have taken to regulate nurse staffing.
The most common regulatory approach, taken by seven states including Oregon, is the requirement
that hospitals have nurse staffing committees composed of representatives of management and staff
that develop nurse staffing plans. This is the regulatory approach recommended by the American
Nurses Association. There has been limited research on the impact of this type of regulation. A study of
Texas’s regulation found increases in nurse staffing, but these were smaller than national trend.
47
A
46
Oregon Public Broadcasting. (2022). Severely short on nurses, Central Oregon hospital system quietly declares crisis.
https://www.opb.org/article/2022/07/27/central-oregon-st-charles-hospital-system-declares-crisis-amid-nurse-shortage/
47
Jones, T., Heui Bae, S., Murry, N., & Hamilton, P. (2015). Texas nurse staffing trends before and after mandated nurse staffing committees.
Policy, Politics, & Nursing Practice, 16(3-4), 79-96.

Future of Oregon’s Nursing Workforce
45
study in New Jersey reported the regulations improved nurse staffing.
48
Finally, a recent national study
found no overall effect on RN or aide staffing and a negative effect on LPN staffing.
49
Oregon’s nurse
staffing law has not been objectively evaluated to assess its effects on nurse staffing, workload, and
satisfaction or on patient outcomes.
The second most common staffing-related regulatory approach is requiring public reporting of nurse
staffing levels; this was in five states in 2019. A national study found no overall effect of this type of
regulation on RN or aide staffing, and a positive effect on LPN staffing.
49
California is the only state to adopt the general approach of fixed minimum staffing ratios. California’s
regulations resulted in higher levels of licensed nurse staffing,
50
particularly for safety-net hospitals,
51
but reductions in staffing of nursing assistants.
52,53,54
The regulations have been associated with greater
RN job satisfaction,
54,55
fewer occupational injuries,
56
increased RN wages,
57,58,59
and slower growth in
uncompensated care services.
60
There is no evidence that the ratios had a causal effect on patient
outcomes.
61,62,63,64
A recent literature review concluded: “All studies that reported on nurse outcomes
demonstrated an improvement associated with the implementation of mandated minimum nurse-to-
patient ratio, but findings related to patient outcomes were inconclusive.”
65
48
de Cordova, P. B., Rogowski, J., Riman, K. A., & McHugh, M. D. (2019). Effects of public reporting legislation of nurse staffing: A trend
analysis. Policy, Politics, & Nursing Practice, 20(2), 92-104.
49
Han, X., Pittman, P., & Barnow, B. (2021). Alternative Approaches to Ensuring Adequate Nurse Staffing: The Effect of State Legislation on
Hospital Nurse Staffing. Medical Care, 59(5), 463-470.
50
Munnich, 2014, Health Economics; Serratt, 2013, J of Nursing Admin; Spetz et al., 2013, Medical Care Research and Review
51
McHugh, M. D., Carthon M. B., Sloane, D. M., Wu, E., Kelly, L., & Aiken, L. H. (2012). Impact of nurse staffing mandates on safety‐net
hospitals: Lessons from California. The Milbank Quarterly, 90(1), 160-186.
52
Burnes Bolton, L., Aydin, C. E., Donaldson, N., Storer Brown, D., Sandhu, M., Fridman, M., & Udin Aronow, H. (2007). Mandated nurse
staffing ratios in California: a comparison of staffing and nursing-sensitive outcomes pre-and postregulation. Policy, Politics, & Nursing
Practice, 8(4), 238-250.
53
Chapman, S. A., Spetz, J., Seago, J. A., Kaiser, J., Dower, C., & Herrera, C. (2009). How have mandated nurse staffing ratios affected
hospitals? Perspectives from California hospital leaders. Journal of Healthcare Management, 54(5).
54
Aiken, L. H., Sloane, D. M., Cimiotti, J. P., Clarke, S. P., Flynn, L., Seago, J. A., Spetz, J., & Smith, H. L. (2010). Implications of the
California nurse staffing mandate for other states. Health Services Research, 45(4), 904-921.
55
Spetz, J. (2008). Nurse Satisfaction and the Implementation of Minimum Nurse Staffing Regulations. Policy, Politics, & Nursing Practice.
2008, 9(1), 15-21.
56
Leigh, J. P., Markis, C. A., Iosif, A. M., & Romano, P. S. (2015). California’s nurse-to-patient ratio law and occupational injury. International
Archives of Occupational and Environmental Health, 88(4), 477-484.
57
Mark, B., Harless, D.W., & Spetz, J. (2009). California's minimum-nurse-staffing legislation and nurses' wages. Health Affairs, 28(2), 326-34.
58
Munnich, E. L. (2014). The labor market effects of California's minimum nurse staffing law. Health Economics, 23(8), 935-950.
59
Harless, D. W. (2019). Reassessing the labor market effects of California's minimum nurse staffing regulations. Health Economics, 28(10),
1226-1231.
60
Reiter, K. L., Harless, D. W., Pink, G. H., Spetz, J., & Mark, B. (2011). The effect of minimum nurse staffing legislation on uncompensated
care provided by California hospitals. Medical Care Research and Review, 68(3), 332-351.
61
Mark, B. A., Harless, D. W., Spetz, J., Reiter, K. L., & Pink, G. H. (2013). California's minimum nurse staffing legislation: results from a
natural experiment. Health Services Research, 48(2), 435-454.
62
Spetz, J., Harless, D. W., Herrera, C. N., & Mark, B. A. (2013). Using minimum nurse staffing regulations to measure the relationship
between nursing and hospital quality of care. Medical Care Research and Review, 70(4), 380-399.
63
Cook, A., Gaynor, M., Stephens Jr, M., & Taylor, L. (2012). The effect of a hospital nurse staffing mandate on patient health outcomes:
Evidence from California's minimum staffing regulation. Journal of Health Economics, 31(2), 340-348.
64
Olley, R., Edwards, I., Avery, M., & Cooper, H. (2018). Systematic review of the evidence related to mandated nurse staffing ratios in acute
hospitals. Australian Health Review, 43(3), 288-293.
65
Twigg, D. E., Whitehead, L., Doleman, G., & El‐Zaemey, S. (2021). The impact of nurse staffing methodologies on nurse and patient
outcomes: A systematic review. Journal of Advanced Nursing, 77(12), 4599-4611.

Future of Oregon’s Nursing Workforce
46
Another more limited regulatory approach, which California has had in place since before it established
its minimum staffing regulations, is to require health care organizations have formal acuity systems to
rate patients’ care needs at the beginning of each shift and staff nurses accordingly. Massachusetts
utilizes an acuity tool as well.
66
Oregon’s nurse staffing law requires that nurse staffing plans account
for differences in patient acuity, but does not require a formal shift-by-shift acuity rating system. There
has not been any research on the effectiveness of requirements that hospitals have formal acuity
systems to determine nurse staffing.
Several studies find that hospitals with proactive hiring and staffing strategies can reduce costs and
improve quality. Predictive hiring strategies can reduce expensive overtime pay and agency nurse use,
leading to notable cost savings.
67
Moreover, an analysis of United Kingdom hospital data reported that
staffing approaches that relied more on permanent staff than contingent/flexible staff were better for
costs and quality of care.
68
Oregon’s 2015 Nurse Staffing Law
In Oregon, hospitals are required to develop and implement a nurse staffing plan approved by the
hospital nurse staffing committee that establishes minimum numbers of RNs, LPNs, and CNAs required
on specified shifts. That minimum number may not be less than one RN and one other nursing staff
member (RN, LPN, or CNA) when a patient is on the unit, and the nurse staffing plan must clearly
identify the number of RNs, LPNs, and CNAs required at any particular patient census. The hospital is
required to meet the minimum number established in the nurse staffing plan any time a patient is
present on the unit, including times when nurses are on meal or rest breaks (OAR 333-510-
0110(2)(f)(h)).
It is important to recognize that Oregon’s requirement for minimum numbers on a shift is not the same
as requiring the staffing plan to set minimum ratios. Oregon’s nurse staffing rules do not have
requirements for the ratio of staff to patients. For example, RN Binh may have a ratio of 1:3 while RN
Sara has a ratio of 1:5, but RN Binh’s patients have high acuity and/or nursing care intensity, while RN
Sara’s five patients have low acuity and/or nursing care intensity.
Oregon’s hospital nurse staffing law was first enacted in 2001. It was intended to ensure patients
receive safe nursing care and appropriate levels of nurse staffing in acute care hospital settings. The
law was amended with minor changes in 2005, however, it was substantially expanded with the
passage of SB 469 in 2015. Key changes to the law concerned the structure and responsibilities of the
Hospital Nurse Staffing Committee (HNSC), a requirement that the HNSC develop and implement a
detailed nurse staffing plan, and the structure of the audit process.
It is beyond the scope of this report to inventory the full extent of the changes brought about by SB 469.
However, some of the most important effects of its implementation included enlarging the
66
Required Elements of the Acuity Tool, Massachusetts Regulations 958 CMR 8.07. Adopted by Mass Register Issue 1290, eff. 7/3/2015.
67
Potts, J., Brouder, P., Helm, S., & Leach, K. (2020). Predictive hiring to maintain excellence in patient care. The Journal of Nursing
Administration, 50(4), 232-236.
68
Saville, C., Monks, T., Griffiths, P., & Ball, J. E. (2021). Costs and consequences of using average demand to plan baseline nurse staffing
levels: a computer simulation study. BMJ Quality & Safety, 30(1), 7-16.

Future of Oregon’s Nursing Workforce
47
responsibilities of the HNSC, increasing the number and type of nurses who must be represented on
the committee, defining new administrative requirements, and creating a mechanism for nursing staff to
report perceived violations of rules concerned with mandatory overtime. With respect to the actual
nurse staffing plan, the 2015 statutory changes created detailed and specific requirements with respect
to the qualifications and competencies of all nursing staff, requirements for measuring the activities of
each nursing unit (i.e., how many discrete tasks were completed and how long did each take), and
accounting for all patient diagnoses in each nursing unit and the variation in patient acuity. It also
established that staffing plans must specify the minimum number of nurses and mix of nursing staff for
each unit, based on patient census and acuity, and account for required meal and rest breaks.
The 2015 changes to Oregon’s hospital nurse staffing law also expanded the scope and structure of the
audit process conducted by staff within the Health Facility License and Certification (HFLC) Program,
which is housed within the OHA and is responsible for monitoring compliance with the law. Prior to
2015, HFLC needed to audit seven percent of Oregon’s hospitals annually; SB 469 increased the
number of annual audits, effectively, to 33 percent of all hospitals and special inpatient care facilities,
such as inpatient hospices. Additional changes to the audit process enacted in 2015 included requiring
that HFLC staff interview each of the co-chairs of the hospital’s nurse staffing committee (the HNSC),
provide a written report of the audit’s findings to the HNSC co-chairs, and conduct a second survey to
determine compliance.
Interviews with key informants revealed that SB 469 significantly increased the workload of HFLC staff
responsible for monitoring compliance, while only providing limited funding for this increased regulatory
work. In recognition of the need for increased funding for the nurse staffing program, the Oregon State
Legislature appropriated additional funding during the 2021 legislative session to support the ongoing
implementation of Oregon’s nurse staffing law. HFLC has begun the process of expanding the nurse
staffing team to facilitate improved implementation of the law.
Interviewees noted it has been very challenging to effectively monitor compliance issues, evaluate
actions taken to remedy those issues, and provide technical assistance to hospitals and staffing
committees that continue to struggle to maintain compliance with the law. Moreover, the increased
workload associated with the audit process has caused delays in conducting complaint investigations.
Key informants noted there is a general lack of understanding of what the law requires, who is covered
by the law, how the audit process works, and what information is needed to ensure compliance, despite
substantial efforts of HFLC staff to communicate on these topics and make themselves available to
answer questions.
Results of the first three-year audit cycle (2017-2019) confirmed that hospitals are struggling to comply
with the nurse staffing law. According to interviews, there were violations at every hospital that was
surveyed; the average number of citations was 18 out of a possible 34 violations. The lack of
understanding about what the law requires, who is covered by the law, how the survey process works,
and what information is needed to ensure compliance has also had the effect of making it very
challenging for hospitals to develop a “Plan of Correction,” which outlines in detail how the hospital will
return to compliance. Improvements to the survey process were introduced for the second survey cycle
(2021-2024), including the use of new tools designed to streamline the survey process and focus
attention on critical elements of compliance.

Future of Oregon’s Nursing Workforce
48
Key informants emphasized hospital nurse staffing is inherently complicated and dynamic. The breadth
and specificity of the hospital nurse staffing law may add additional challenges to ensure staffing is in
accordance with the law. While the nurse staffing law has safe patient care as its focus, interviewees
suggested the law’s requirements may not always be helpful in terms of having the right staff at the
right time for the right unit to take care of patients.
Nurse burnout
National estimates of nurse burnout
Prior to the COVID-19 pandemic, national studies estimated that 35 to 45 percent of U.S. nurses
reported experiencing burnout.
69,70
In 2018, 31.5 percent of nurses across the nation reported leaving
their employment due to burnout.
71
Since the onset of the COVID-19 pandemic, multiple studies have
reported significant increases in self-reported nurse burnout. Between July 2020 and August 2021, the
American Nurses Foundation reported a 350 percent increase in the level of self-reported burnout.
Three additional studies conducted between May and December 2020 reported 54-64 percent of
nurses experiencing burnout,
72,73
with one study reporting 76 percent of critical care nurses
experiencing burnout.
74
Factors contributing to nurse burnout
Studies documenting the various factors contributing to burnout have existed long before the COVID-19
pandemic. These factors include insufficient or inadequate staffing, unmanageable work schedules,
repeated exposure to facing death and loss, administrators who do not respond to concerns, increased
threats of physical or psychological harm, pressures to adapt to new technologies, and performing non-
nursing tasks – all issues that only heightened during the COVID-19 pandemic.
69,69,75,76,77
Multiple
studies and literature reviews also document structural organizational issues that lead to nurse burnout,
including a perceived lack of organizational support, perceived negative practice environment,
69
National Academies of Sciences, Engineering, and Medicine. (2019). Taking Action Against Clinician Burnout A Systems Approach to
Professional Well-Being. Washington, DC: The National Academies Press.
70
French, R., Aiken, L. H., Rosenbaum, K. E. F., & Lasater, K. B. (2022). Conditions of Nursing Practice in Hospitals and Nursing Homes
Before COVID-19: Implications for Policy Action. Journal of Nursing Regulation, 13(1), 45-53.
71
Shah, M. K., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse
burnout in the US. JAMA network open, 4(2), e2036469-e2036469.
72
Prasad, K., McLoughlin, C., Stillman, M., Poplau, S., Goelz, E., Taylor, S., ... & Sinsky, C. A. (2021). Prevalence and correlates of stress and
burnout among US healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine, 35,
100879.
73
Sinsky, C. A., Brown, R. L., Stillman, M. J., & Linzer, M. (2021). COVID-related stress and work intentions in a sample of US health care
workers. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 5(6), 1165-1173.
74
LeClaire, M., Poplau, S., Linzer, M., Brown, R., & Sinsky, C. (2022). Compromised Integrity, Burnout, and Intent to Leave the Job in Critical
Care Nurses and Physicians. Critical care explorations, 4(2).
75
Jun, J., Ojemeni, M. M., Kalamani, R., Tong, J., & Crecelius, M. L. (2021). Relationship between nurse burnout, patient and organizational
outcomes: Systematic review. International Journal of Nursing Studies, 119, 103933.
76
Shin, S., Park, J. H., & Bae, S. H. (2018). Nurse staffing and nurse outcomes: A systematic review and meta-analysis. Nursing outlook,
66(3), 273-282.
77
Simpson, K. R., Lyndon, A., & Ruhl, C. (2016). Consequences of inadequate staffing include missed care, potential failure to rescue, and
job stress and dissatisfaction. Journal of Obstetric, Gynecologic & Neonatal Nursing, 45(4), 481-490.

Future of Oregon’s Nursing Workforce
49
organizational culture, or ethical climate, and negative perceptions of staffing, management, and
resources
69,78,79
Effect of Nurse Burnout on Patient and Organizational Outcomes
Abundant studies have documented the negative impact of burnout. Burnout lowers nurses’ quality of
care, organizational commitment, and increases their intention to leave the job. Multiple systematic
reviews document that nurse burnout is associated with decreased quality of care, patient safety,
patient satisfaction, nurses’ job satisfaction, organizational commitment, and productivity.
69,80
In direct
patient care, nurse burnout is associated with higher odds of patient mortality, failure to rescue, and
prolonged hospital stay.
81
Many nurses who are experiencing burnout choose to leave their positions or the nursing field
altogether.
69,71,73,74,82
Those who continue working amidst burnout are more likely to rate care quality at
their workplace as less than excellent and give their hospital an unfavorable patient safety rating.
70
In
addition to the disruption to patient care, the loss of a nurse leaving their position is also associated
with significant financial costs, estimated from $11,000 to $90,000 per nurse with up to $8.5 million in
associated wider costs (e.g., unfilled vacancies, patient deferment, training, and orientations).
83
Evidence for mitigating burnout
One study found evidence that hospitals with good work environments as well as American Nurses
Credentialing Center Magnet Recognition Program
84
status attenuated the effect of nurse burnout on
poor patient outcomes.
81
Additional studies report positive nurse work environments have positive
effects on burnout, job satisfaction, and intention to leave,
85,86
while electronic health records can have
negative impacts on nurse satisfaction and stress.
87
78
Sonis, J., Pathman, D. E., Read, S., & Gaynes, B. N. (2022). A national study of moral distress among US internal medicine physicians
during the COVID-19 pandemic. Plos one, 17(5), e0268375.
79
Squires, A., Clark-Cutaia, M., Henderson, M., Arneson, G., & Resnik, P. (2022). " Should I stay or should I go?” Nurses’ Perspectives About
Working During the Covid-19 Pandemic in the United States: A Summative Content Analysis Combined with Topic Modelling. International
Journal of Nursing Studies.
80
Monsalve-Reyes, C. S., Luis-Costas, S., Gómez-Urquiza, J. L., Albendín-García, L., & Aguayo, R. (2018). Burnout syndrome and its
prevalence in primary care nursing: a systematic review and meta-analysis. BMC family practice, 19(1), 1-7.
81
Schlak, A. E., Aiken, L. H., Chittams, J., Poghosyan, L., & McHugh, M. (2021). Leveraging the work environment to minimize the negative
impact of nurse burnout on patient outcomes. International Journal of Environmental Research and Public Health, 18(2), 610.
82
Hendrickson, R. C., Slevin, R. A., Hoerster, K. D., Chang, B. P., Sano, E., McCall, C. A., ... & Raskind, M. A. (2022). The impact of the
COVID-19 pandemic on mental health, occupational functioning, and professional retention among health care workers and first responders.
Journal of general internal medicine, 37(2), 397-408.
83
Halter, M., Boiko, O., Pelone, F., Beighton, C., Harris, R., Gale, J., ... & Drennan, V. (2017). The determinants and consequences of adult
nursing staff turnover: a systematic review of systematic reviews. BMC Health Services Research, 17(1), 1-20.
84
ANCC Magnet Recognition Program®: https://nursingworld.org/organizational-programs/magnet/
85
Lake, E. T., Sanders, J., Duan, R., Riman, K. A., Schoenauer, K. M., & Chen, Y. (2019). A meta-analysis of the associations between the
nurse work environment in hospitals and 4 sets of outcomes. Medical care, 57(5), 353.
86
Brom, H., Carthon, J. M. B., Ikeaba, U., & Chittams, J. (2020). Leveraging electronic health records and machine learning to tailor nursing
care for patients at high risk for readmissions. Journal of nursing care quality, 35(1), 27.
87
Gephart, S., Carrington, J. M., & Finley, B. (2015). A systematic review of nurses' experiences with unintended consequences when using
the electronic health record. Nursing administration quarterly, 39(4), 345-356.

Future of Oregon’s Nursing Workforce
50
Multiple reports and articles offer recommendations on the individual, organizational, and policy or
community levels address nurse burnout, but the effectiveness of these recommendations and
programs have not yet been evaluated.
69,81,88,89
Oregon Center for Nursing’s Survey on Nurse Burnout
Survey and Demographics
In response to the evidence about nurse burnout, OCN created the RN Well-Being Project, an initiative
established in 2020 designed to provide research and resources on the mental and emotional well-
being for Oregon’s nurses, and to implement evidence-based interventions to positively impact nurse
mental health. This project has brought together nursing leaders from all areas of health care,
legislators, policy analysts, association representatives, research analysts, and mental health
professionals who created a multi-phase approach to address nurse well-being.
As part of the first phase of this project, OCN partnered with the OSBN in April 2022 to survey LPNs,
RNs, and APRNs licensed to practice in Oregon. The purpose of the survey was to better understand
the stressors licensed nurses experience in the work environment in the state of Oregon. The
respondents were not asked to identify themselves or their employer.
The survey was sent to more than 80,000 individuals, and OCN received 5,500 completed surveys. Of
those, 572 were located out of state, and were removed from the analysis. Table 16 provides
information about the numbers of each type of nurse represented in the data.
88
National Academies of Sciences, Engineering, and Medicine (2021). The Future of Nursing 2020-2030: Charting a Path to Achieve Health
Equity. Washington, DC: The National Academies Press. https://doi.org/10.17226/25982.
89
U.S. Department of Health and Human Services Office of the U.S. Surgeon General (2022). Addressing Health Worker Burnout: The U.S.
Surgeon General’s Advisory on Building a Thriving Health Workforce.

Future of Oregon’s Nursing Workforce
51
Table 16. Nurse Well-Being Mental Health Survey respondents.
LPN RN NP CRNA CNS Total
All Surveys Received 243 4,870 329 40 18 5,500
From Nurses Practicing in
Oregon
229 4,356 291 36 16 4,928
Note: Surveys were sent out to every licensed LPN, RN, NP, CRNA, and CNS, including to those working out-of-state. Only surveys received
from nurses practicing in Oregon were included in the analyses.
The overall demographics of the survey respondents reflected the Oregon nurse population. The
notable exceptions occurred in three areas: age, work setting, and years of experience. Respondents
tended to be older (Figure 25), over-represented in the hospital setting, and under-represented in the
public policy/regulator agency setting (Figure 26). In addition, a high proportion of respondents
indicated they have practiced as a nurse for more than 25 years (Figure 27).
Figure 25. Age of RN Well-Being Mental Health Survey respondents.
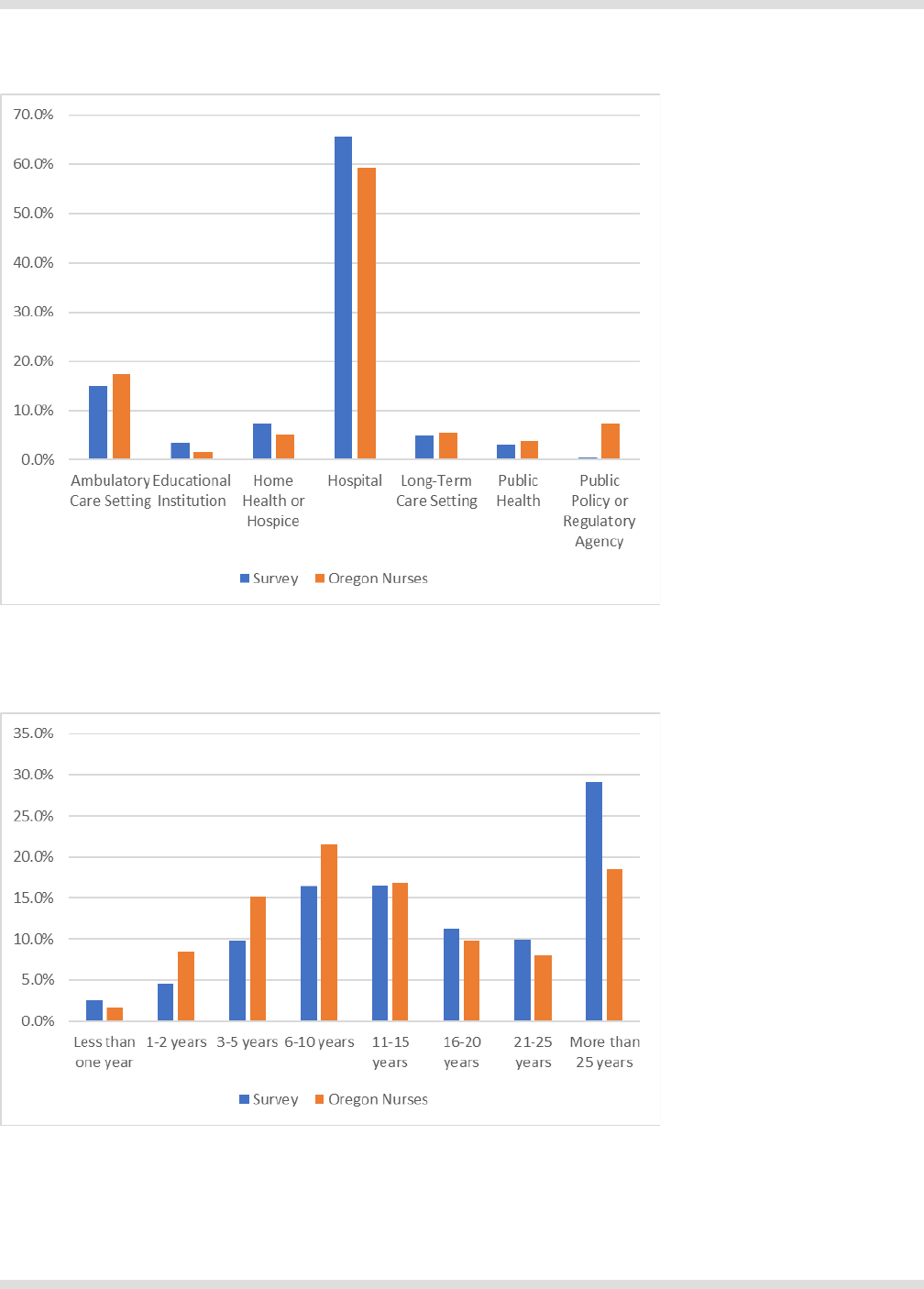
Future of Oregon’s Nursing Workforce
52
Figure 26. Work settings of RN Well-Being Mental Health Survey respondents.
Figure 27. Years of experience of RN Well-Being Mental Health Survey respondents

Future of Oregon’s Nursing Workforce
53
Most nurses surveyed reported working directly with COVID-19 patients, particularly in hospital, long-
term care, and home health or hospice settings. About 30 percent of respondents indicated they did not
work with COVID-19 patients. Of those, 23 percent indicated they had a risk of potential exposure to
COVID-19 despite not working directly with patients.
Results
The sample collected indicated that, despite mental and emotional health supports implemented by
employers and state agencies, Oregon nurses continue to report severe mental suffering and
exhaustion. In this unpublished study, 83 percent of nurses reported increased feelings of stress, 80
percent reported increased feelings of frustration, and 68 percent reported increased feelings of anxiety
in the last three months (see Figure 28). About 97 percent of nurses reported experiencing a work-
related stressor, such as a heavy workload, uncertainty about the future, and burnout (Figure 29).
Figure 28. Feelings regularly experienced at work.
Figure 29. Top five workplace stressors.
60%
62%
68%
80%
83%
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
Unappreciated
Being Overwhelmed, Undervalued
Anxiety, Exhaustion, & Burnout
Frustration
Stress
45%
47%
63%
69%
70%
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
Working with Colleagues w/ Mixed
Competencies
Insufficient Communition w/ Leadership
Burnout
Uncertainty About Return to Normal
Heavy or Increased Workload

Future of Oregon’s Nursing Workforce
54
These stressors are impacting nurses both physically and mentally. Nurses from all settings report
feelings of emotional exhaustion, work-related dread, difficulty falling or staying asleep, and physical
exhaustion (Figure 30). An alarming one in four nurses reported having upsetting thoughts, images,
and/or dreams with 22 percent stating they are more likely to smoke, drink, and/or use substances to
cope with their symptoms. Of nurses who work in ambulatory care, hospitals, home health or hospice,
or public health, 50 percent or more reported questioning their career path.
Figure 30. Symptoms experienced recently by respondents.
Despite increased services offered by employers to provide mental and emotional health services to
their employees, almost half of respondents said they do not receive adequate support at work (Figure
31). Two out of five nurses reported actively seeking out mental health services, but only 15 percent
utilized work-provided employee assistance plans (EAP), and about 12 percent utilized work-provided
aps and training. Overwhelmingly, nurses report receiving most of their emotional support from home
and personal sources (Figure 32).
52%
54%
55%
56%
59%
66%
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
Compassion Fatigue
Questioning Career Path
Physical Exhaustion
Trouble Sleeping
Work-Related Dread
Emotional Exhaustion

Future of Oregon’s Nursing Workforce
55
Figure 31. Do nurses receive adequate emotional support at work?
Figure 32. Do nurses receive adequate emotional support at home?
Despite the mental health challenges nurses are experiencing, 95 percent of the respondents indicated
a belief that workplaces could change to support mental and emotional well-being. As presented in
Figures 33 and 34, nurses reported changes they both need and want their employers to take to
improve their mental health, including hiring more nurses and support staff, engaging in meaningful
employee recognition, providing more flexibility with work schedules and opportunities for learning, and
more support from managers.
Yes
33%
No
49%
Unsure
18%
Yes
71%
No
20%
Unsure
9%

Future of Oregon’s Nursing Workforce
56
Figure 33. Changes in work environment nurses say they need.
Figure 34. Changes in work environment nurses say they want.
The findings of the RNWB Mental Health survey indicate there is a gap in prevention measures that
consider the individual area of practice, organization, environment, and culture of the workplace to
support mental health.
Burnout reported in interviews
In interviews, key informants noted that prior to the COVID-19 pandemic, some hospitals had begun to
emphasize moving patients to sub-acute settings as rapidly as possible, to admit higher acuity patients
with more intense care needs. This was already a source of concern regarding potential burnout among
nurses. The experience of caring for patients throughout the pandemic, however, was unprecedented in
terms of the psychological effect on hospital nursing staff. One interviewee characterized the
50%
59%
66%
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
Meaningful Recognition
More Support Staff
More Nurses
27%
27%
33%
35%
35%
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
Emotional Health Resources
Revisions to Policies & Procedures
More Supervisor Support
Flexible Work Schedules
Dedicated Time to Learn

Future of Oregon’s Nursing Workforce
57
phenomenon of burnout resulting from the pandemic as having two components: change fatigue and
mourning. The sheer number of changes in both the workplace and life outside of work were difficult to
cope with. There was also some sense of mourning for the loss of normal life, and anxiety stemming
from the realization that it may be gone forever. In this context, several key informants commented the
experience of the pandemic has caused both nursing education programs and employers to realize
how little focus has been given to preparing nurses to cope with stress and trauma.
One key informant, an RN who works in a medical intensive care unit for a large hospital system,
described how the intensity of patient care needs during the different waves of COVID-19 admissions
consumed resources across all nursing units. Nurses who were not trained to provide critical care, by
necessity, were doing so. It created a highly stressful environment for everyone. “We were so
consumed with caring for COVID-19 patients, and we knew that other patients were being denied beds
and weren’t getting care, and you felt so guilty. And then the patients you were caring for…so many of
them died. It was terrible,” she commented. The weight of these circumstances was very challenging to
process emotionally.
Another key informant, also a critical care nurse, described the experience of caring for a second wave
COVID-19patients who had refused to be vaccinated. It engendered feelings of anger and resentment,
she acknowledged nurses found it hard to be empathetic towards these patients. There was a
“collective feeling that we had given so much to get through the early days of COVID, before the
vaccine, and now we were going through it all over again, and we didn’t need to…it could have been
prevented,” she remarked. She said the experience was demoralizing, and she described it as a
watershed moment, after which nurses began leaving the hospital.
The experience of burnout brought about by the experience of caring for patients throughout the
COVID-19 pandemic appears to be a critical factor contributing to a nursing shortage in Oregon. The
nursing shortage, in turn, is contributing to feelings of anxiety, stress, and burnout. As experienced
nurses have left, their positions are being filled with inexperienced nurses or traveler nurses. “There is
always this sense that things are not safe,” commented one interviewee who works in a hospital ICU.
She added, “Our hospital acquired infection numbers are up, and regular staff resent the travelers who
are getting paid way more money.” She referenced the lack of cohesion in the unit culture, and
described how new hires are being trained by new hires, inexperienced nurses are being “thrown” into
preceptor and training roles. “There just aren’t enough experienced nurses to backstop, to stalk our
notes, to make sure things are being done safely,” she said.
Several key informants described how health care systems are adapting to nursing staff burnout. For
example, by creating more opportunities for nurses to work across different care settings or clinical
areas within the inpatient setting. Another interviewee noted hospitals are trying to be more flexible
around length of shift, the mix of days and nights, and the ability to work part-time. Key informants also
reported hospitals are reconfiguring patient care transitions to reduce the volume of “hand-offs”, and
instituting “respite” assignments that allow nurses to go and work in other areas of the hospital in a non-
patient care capacity. Several key informants talked about the importance of strong shared governance
– giving nurses more ownership over decisions that directly affect them – as part of any strategy to
create a healthier workplace environment. Some interviewees acknowledged that health care systems
aren’t sure what to do to support their nursing staff, who are trying to process the trauma of the past
several years. Some interviewees believe there needs to be a “cultural shift”; some employers are

Future of Oregon’s Nursing Workforce
58
experimenting with “mindfulness-based stress reduction” and “cognitive behavioral therapy groups.”
There was a view that repeating the “same old mantras” of exercise, wellness, nutrition was insufficient,
and that deeper and concerted programs were required to address burnout. However, one interviewee,
a critical care nurse, emphasized that there was a collective sense among nurses that “there is no end
in sight.”
“I feel like the past two years have been spent growing apart from most everybody else’s point
of view. When you spend so much time, years, trying to keep people alive, and so many of them
die, and it feels like it was preventable…it makes it hard to have conversations with people
about anything else. But you realize that if you are real with people, you freak them out, so you
downplay it and so they don’t get it. I don’t know if there is a way to communicate what
happened over the past two years, and have people really understand, but also be okay with
you telling them. I don’t know how we are going help nurses be okay. We haven’t figured out
how to help people who experience war, the trauma of war. I just don’t think we’re going to
figure this out either.”
Nursing education capacity in Oregon
An important consideration for ensuring an adequate nursing workforce is how to expand nursing
program capacity. If schools can graduate more students, employers would have a larger pool of
candidates from which to hire. However, there are two major limitations to growing nursing education
programs: the lack of nurses who wish to work as nurse faculty, and challenge of identifying clinical
placement experiences for student training.
Faculty shortages
Key informants and research from OCN emphasized that the inability to expand capacity Oregon’s
nursing education programs to increase the number of new graduates is a major factor contributing to
an inadequate supply of new entrants to workforce. A principal factor limiting nursing programs’
expansion is their inability to recruit and hire for open nurse faculty positions. The shortage of nursing
faculty was described as a “crisis” by multiple interviewees.
The challenge of finding nurses to serve as faculty has been an ongoing problem in the state of Oregon
for more than 15 years. Much literature has been published both nationally and from OCN describing
the factors discouraging nurses from becoming faculty. According to a 2017 study by OCN
90
, the main
factors contributing to difficulties in recruiting faculty include:
• Faculty salaries: According to the Oregon Employment Department, nurse teachers and instructors
in Oregon make an average of $91,042 annually, while the average registered nurse salary is
$102,180.
91
Most nurse educators must have higher education (master’s level or higher), which they
must obtain often at their own expense, to work as faculty at an ADN or BSN program. This means
many nursing students leave the classroom with positions where they make more than the faculty
who taught them. Among those interviewed for this study, noncompetitive pay was uniformly reported
as the main reason why it is so hard to attract nurse faculty.
90
Oregon Center for Nursing (2017). Oregon’s Nursing Faculty: Why Are They Leaving? Portland, OR.
91
Oregon Employment Department (2022). 2022 Oregon Wage Information. Salem, OR.

Future of Oregon’s Nursing Workforce
59
• Workload: Nurse faculty are required to fulfill all responsibilities of higher education (publishing,
participating in academic committees, spending extra hours with students), but also often supervise
experiential learning (clinical placements) as part of their job description.
• Work environment: Oregon nurse faculty report difficult work environments, with conflict among
managers and co-workers to be a main factor in job dissatisfaction.
Despite these challenges, nursing education programs appear to have been able to increase the
number of faculty they employ. As seen in Figure 35, the number of faculty in Oregon’s RN education
programs grew between 2018 and 2020; although the number decreased between 2020 and 2021, it
remained higher than in 2018.
Figure 35. Number of faculty at Oregon’s RN programs.
Source: OSBN, Nursing Program Annual Report, 2012-2021
Note: The OSBN Nursing Program Annual Report did not collect data for number of faculty at Oregon’s RN programs in 2020, but resumed
this data collection in 2021.
Lack of Clinical Placements
All nursing students must engage in clinical experiences as part of their education. Clinical experiences
are provided at hospitals, long-term care facilities, and other community-based locations, and rely on
the shared agreements between facilities and schools. While placements can be completed at almost
any health care facility where students can be supervised, there is a preference for placements to be
held in hospital settings. Admitting more students to nursing schools without identifying clinical
placement experiences for students will delay education and strain relationships. Moreover, it increases
strain on nurse preceptors who support newly graduated nurses during the onboarding process
because preceptors must compensate for graduates limited clinical experiences. This, in turn, reduces
the availability of clinical placements because hospitals often use the same pool of expert nurses as
preceptors for both new graduate onboarding and student placements.
The challenges associated with clinical placements existed prior to the COVID-19 pandemic, however
the restrictions of in-person clinical training for nursing students exacerbated the problem. OCN
250
263
233
202
232
212
242
285
243
406
376
381
426
412
387
371
493
467
0
100
200
300
400
500
600
2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
ADN Programs
BSN Programs

Future of Oregon’s Nursing Workforce
60
conducted a study among healthcare agencies and nursing programs at the onset of the pandemic, and
found the current model of clinical education to be sorely lacking, particularly in collaboration among
facilities and programs, and the full acceptance of nursing students as functional members of the
healthcare team.
92
For decades, Oregon has attempted to address clinical placement shortages with
consortiums, shared databases, and alternate placement models, and still the challenges with clinical
placement restricts nursing school capacity and Oregon’s ability to produce more graduates.
However, the availability of clinical placements is now threatened by the acute shortage of experienced
nurses. This is having an impact on clinical training across all types of care settings, acute, sub-acute,
and community-based. One key informant noted that nursing students in her local program cannot
access clinical training outside the hospital setting, as there are no training spots available. In locations
with more than one nursing education program, there is an insufficient number of clinical spots to meet
demand.
An important ramification of this reduction in capacity to provide clinical training to nursing students is
that new graduates are entering the workforce with little hands-on experience working with patients.
Employers are trying to address this by recalibrating their transition-to-practice programs. But it remains
a significant challenge. Key informants described efforts by nursing education programs to adapt to the
lack of clinical placements. One example was to have a faculty member placed at a clinical site to
precept students directly during their clinical rotations. In this case, the faculty member was an NP with
experience in ambulatory care. The nursing program was able to structure an agreement with a local
outpatient clinic whereby the program covered the malpractice insurance for the faculty member, and
that NP billed for services through the clinic site. Key informants emphasized that nursing education
programs will need to be creative in finding solutions to the issue of “missing” clinical spots, part of
which will be to exhibit flexibility and develop new kinds of partnerships with health care systems.
Transition into Practice for New Nurse Graduates
When nurses complete their RN education, they have the knowledge and skills required to work as
licensed nurses. Nurse researchers and educators refer to these new nurses as “novices” who will
acquire skills over the course of their careers.
93
The novice nurse needs experience and mentoring to
develop skills to make decisions when unusual circumstances arise. As the nurse encounters more
complex situations, he or she develops competency as a nurse – typically requiring two or three years
of work. With continued practice, the nurse becomes proficient and advances to the expert level of
nursing. The expert nurse has an intuitive grasp on most situations and can rapidly make decisions in
the face of complexity.
During early independent practice, many new graduate nurses face challenges due to a discrepancy
between demonstrated knowledge and competent practice. The disparity between new graduate
nurses’ academic knowledge and their ability to provide basic or complex nursing care in various health
care settings has long been documented. Multiple national systemic reviews and studies have
documented the challenges during the transition-to-practice from new graduate nurse to accomplished
92
Oregon Center for Nursing. (2020). Not Working Well: Clinical Placement for Nursing Students in an Era of Pandemic. Portland, OR.
93
Benner, P. (1982). From novice to expert. American Journal of Nursing, 82(3):402-407.

Future of Oregon’s Nursing Workforce
61
practitioner. New nurses often identify their initial professional adjustment in terms of the feelings of
anxiety, insecurity, inadequacy, and instability it produces.
94,95
A large contributor of stress comes from
knowledge insecurity, or not feeling adequately prepared or confident in their skill performance. New
nurses often experience a fear of “missing something,” making mistakes, or asking questions, and
especially feel that they do not have enough time to apply careful assessment and critical thinking to
new situations.
96,97,98,99
New graduate nurses are also navigating new roles and tasks during this time, and stress related to
time management, organization, priority-setting, and personal accountability arises while they delegate
and supervise unlicensed assistive personnel or when they through different work units during their
orientation.
100
Systemic organizational issues such as inadequate staffing patterns, redundant and
unnecessary paperwork, delayed and arbitrary work schedules, and problems accessing vital policies
and procedures also add to new nurses’ daily operational burdens.
93
Multiple studies have also found
new nurses often feel unsupported by their work environments when preceptors, physicians, or other
team members are perceived to be disinterested, unprofessional, or inconsistent in their
communication. Many new nurses feel a lack of career development opportunities, dissatisfaction with
salary, and dissatisfaction with schedules.
93,94,95
For the academic years 2020 and 2021, clinical hours requirements were waived; ultimately, OSBN
made several of the pandemic-related changes to clinical hours requirements permanent (e.g. no
minimum hours, increased the number of hours completed as simulation, lowered NCLEX cohort, pass-
rate threshold). The long-term effect of these changes on nurse readiness for practice are unknown.
Strategies to address transition-to-practice challenges
Today, the transition of new nurses to practice is even more important due to health care systems
becoming increasingly complex, changes in health services, such as decreased length of hospital stay,
and advanced technologies. Whereas these challenges have been documented since the early 1970s,
there is renewed urgency to examine new graduate nurse perceptions of the initial practice experience
due of concerns about retention.
Many hospitals and health care employers provide orientation, residency, preceptorships, or transition-
to-practice programs to bridge this knowledge and practice gap. These programs often address
transition-to-practice challenges with two areas of focus. The first area of focus addresses nurse
competency for safe practice. This is often accomplished by increasing new graduate nurses’ clinical
94
Spector, N., Blegen, M. A., Silvestre, J., Barnsteiner, J., Lynn, M. R., Ulrich, B., Fogg, L. & Alexander, M. (2015). Transition to practice study
in hospital settings. Journal of Nursing Regulation, 5(4), 24-38.
95
Duchscher, J. B. (2008). A process of becoming: The stages of new nursing graduate professional role transition. The Journal of Continuing
Education in Nursing, 39(10), 441-450.
96
Aukerman, R., White, L., Gierach, M., Miller, T., & Wolles, B. (2022). The lived experience of nurses transitioning to professional practice
during the COVID‐19 pandemic. Nursing Forum 57(5), 756-764.
97
Casey, K., Fink, R. R., Krugman, A. M., & Propst, F. J. (2004). The graduate nurse experience. The Journal of Nursing Administration,
34(6), 303-311.
98
Clark, C. M., & Springer, P. J. (2012). Nurse residents' first-hand accounts on transition to practice. Nursing Outlook, 60(4), e2-e8.
99
Urban, R. W., & Barnes, D. M. (2020). Transition to practice: The lived experience of new graduate nurses in early solo flight. Journal for
Nurses in Professional Development, 36(2), 74-81.
100
Hampton, K. B., Smeltzer, S. C., & Ross, J. G. (2021). The transition from nursing student to practicing nurse: An integrative review of
transition to practice programs. Nurse Education in Practice, 52, 103031.

Future of Oregon’s Nursing Workforce
62
knowledge through structured programming and simulations for development of technical skills,
101,102
as
well as increasing professional socialization through simulations for care prioritization, managing clinical
dilemmas, communication, and clinical decision skills; implementation of Dedicated Education Units or
immersion programs prior to graduation.
100,101,103
The second area of focus addresses the stress experienced by new nurses during the transition period.
Health care organizations employing new nurses are increasingly requiring preceptor training, offering
mentorship through an evidence-based practice program, providing resources to manage stress,
transition shock, and mental wellness, and building new nurse confidence with supportive staff,
inclusion as a vital member of the organization, and time to familiarize oneself to organizational
policies, procedures, and routines.
100,101,102,104
Multiple systematic reviews and studies find interventions to ease the transition-to-practice experience
are beneficial and can have a positive impact on job satisfaction and retention. However, these reviews
also suggest the need for greater standardization of concepts that should be evaluated and the
instruments used to determine if new nurses are successfully transitioning into professional
nursing.
98,100,102,103,104, 105
In interviews, key informants acknowledged robust transition-to-practice nursing programs have been
widely adopted by hospital-based employers. These include both general onboarding and orientation-
style programs as well as formal residency-style programs. Interviewees noted that health care system
leadership has come to understand that these programs are a necessary investment in supporting new
graduate nurses in the first year of employment. Key informants referred to the support nurses receive
in the first few years of employment as being correlated with remaining in the profession. Transition-to-
practice programs are an important part of any workforce retention strategy.
These types of programs are not limited to new graduate nurses. One interviewee described a
fellowship program his health care system has developed for experienced nurses who want to move
into specialty care areas. Eventually, all experienced nurses in this health care system who move from
general practice to specialty care will go through this inpatient fellowship training program. However,
key informants also acknowledged that rural hospitals, including critical access hospitals were less
likely to have well organized, transition-to-practice programs for either new graduate hires or
experienced nurses transitioning to a new area of clinical care. It was suggested state agencies could
offer targeted support to these rural sites to help develop and sustain these types of programs.
101
Halfer, D., & Benedetto, C. (2020). Evolution of a newly licensed RN transition-to-practice program: theory and development supporting
accreditation. JONA: The Journal of Nursing Administration, 50(1), 28-33.
102
Kenny, A., Dickson-Swift, V., McKenna, L., Charette, M., Rush, K. L., Stacey, G., ... & Phillips, C. (2021). Interventions to support graduate
nurse transition to practice and associated outcomes: A systematic review. Nurse education today, 100, 104860.
103
Dimino, K., Louie, K., Banks, J., & Mahon, E. (2020). Exploring the impact of a dedicated education unit on new graduate nurses’ transition
to practice. Journal for nurses in professional development, 36(3), 121-128.
104
Reebals, C., Wood, T., & Markaki, A. (2022). Transition to practice for new nurse graduates: Barriers and mitigating strategies. Western
Journal of Nursing Research, 44(4), 416-429.
105
Spector, N. (2015). The National Council of State Boards of Nursing’s Transition to Practice study: implications for educators. Journal of
Nursing Education, 54(3), 119-120.

Future of Oregon’s Nursing Workforce
63
OCN has identified about 15 nurse residency programs in the state, some of which have multiple sites
(~20 sites total).
106
There may be more programs, and some onboarding programs have characteristics
similar to nurse residencies. As seen in Figure 36, many of these programs are in rural and small
communities.
Figure 36. Known nurse residency programs in Oregon.
Source: Oregon Center for Nursing, 2022
Challenges with the LPN and CNA workforce
As previously discussed, Oregon’s LPN workforce is small, and are predominantly employed in
outpatient care settings, for example in long-term care sites (e.g., skilled nursing facilities or residential
care facilities) or ambulatory care clinics. Some key informants noted that LPNs once were employed in
acute care settings with greater frequency, and this may still be the case in rural areas of the state. It
was suggested that LPNs could play a role in addressing the current nursing shortage affecting so
many inpatient facilities. One interviewee stated, “I would love to hire LPNs into our system, but I don’t
even know where to source them.”
However, one interviewee who oversees workforce development and the nurse residency program for a
rural health care system reported having been consistently successful in recruiting LPNs to work in the
system’s acute care hospitals. This health system has historically employed LPNs in acute care, and
LPNs participate in the system’s nurse residency training program. It may be the case that health care
systems that have always utilized LPNs for inpatient settings may be in better position to recruit and
retain them. These systems have both the experience defining the scope and role of LPNs, and
106
Oregon Center for Nursing: https://oregoncenterfornursing.org/residency-transition-to-practice-programs/

Future of Oregon’s Nursing Workforce
64
documentation processes in place to ensure LPNs are meeting standards of patient care. This is
something other key informants acknowledged would be a challenge, with respect to integrating LPNs
into the acute care setting.
In contrast, some interviewees expressed the view that LPN education programs may not be equipping
graduates with the skills needed to work in inpatient settings, even though many inpatient procedures
and related skills are within their scope. One key informant, whose health care system does employ
LPNs in acute care, acknowledged needing to establish a partnership with the local LPN education
program to help shape the curriculum to ensure graduates were exposed to the full scope of
competencies with the LPN scope of practice. LPN willingness to move from non-acute care settings
into acute care was perceived by some interviewees to be correlated with age and experience. A new
LPN graduate may be more willing to go into acute care relative to an LPN with many years of
experience in non-acute care settings. One interviewee referred to recent graduates as being “still in
the learning mode,” which may help them overcome any anxiety about developing additional skills.
Professional cultural issues may also be a factor in the willingness of LPNs to work in acute care, as
LPNs have historically been viewed by RNs as “less than” RNs in hospital settings. Finally, one key
informant expressed the view that hiring LPNs away from sub-acute care settings presented an ethical
issue, given that these settings are experiencing acute LPN and CNA staffing shortages.
Some of those interviewed expressed concern about training requirements for CNAs. OSBN requires
more than double the number of training hours than the federal standard. Some of those interviewed
thought that OSBN regulations that define skills and scope of practice for CNAs make it difficult to
define a clear career ladder from CNA to LPN to RN. The existence of two levels of CNA was perceived
by some as confusing; some believed that the intent of two categories was to define a CNA1 that would
work in long-term care settings and a CNA2 that would work in acute care settings, but thought that
OSBN “muddied the waters” by defining skills and scope for CNA1 that overlap with CNA2. This was
perceived as a challenge to the recruitment and retention of CNAs in long-term care. The OSBN
observed in our interview that many other states have more hours of training required for CNAs than
the federal standard, often justifying this by noting advances in care practices and technology and
require more training. OSBN also observed current regulations allow CNAs who were certified in other
states with fewer hours of training can have their certification endorsed into Oregon. Any change in the
number of hours required for certification must be proposed and established to the Board, as it is not
under the purview of the legislature.
Solutions Implemented and Considered in Oregon
Oregon Wellness Program
To address the immediate needs of nurse mental health, the state allocated $500,000 from OSBN to
support the Oregon Wellness Program, a nonprofit that promotes health care professionals’ well-being
through free counseling, education, and research. Originally designed to support the well-being of
physicians, physician assistants, advanced practice providers, nurse practitioners, and dentists, the
funding from OSBN expanded the reach to RNs, LPNs, and CNAs.

Future of Oregon’s Nursing Workforce
65
Temporary Licensure
New regulations were passed through HB 4003 that expanded the availability of temporary licenses to
all nurses endorsing into Oregon, regardless of clinical specialty; previously, the temporary license-
seeker had to be employed in specific clinical areas. This new regulation also extended the length of
time in which the temporary license was valid from 30 days to 60 days, with one renewal for another 30
days. The change was viewed as an important component of maintaining the inflow of nurses as
emergency authorization licenses (EAL) ended. In an interview, OSBN reported there are now
approximately 1000 people who have been allowed to continue to work while the OSBN clears a
backlog of applicants.
Nurse Intern Licensure
In addition, HB 4003 also created a “nurse intern” license for nursing students who are enrolled in a
nursing education program and employed in a hospital or other facility. The nurse intern role is like the
registered apprenticeship model, in which student nurses can be paid while they obtain clinical
experience. This approach can increase capacity at the hospital and provide access to clinical
education for nursing programs. OSBN is in the process of creating rules for how the nurse intern
license will be administered and regulated.
107
Nurse Licensure Compact
The Nurse Licensure Compact (Compact) is an interstate agreement that allows nurses to hold a single
license issued by a Compact member state, permitting them to practice in any other state that is also a
Compact member. While Oregon has discussed being a part of the Compact for many years, and no
legislation has been seriously considered.
A Compact license enables nurses to provide care to patients in person or via telehealth to patients in
any Compact state, subject to each state’s practice laws and subject to continued residency in the
issuing state (i.e., the nurse’s primary state of residence). States that participate in the Compact can
choose to offer both single-state licenses and multi-state licenses.
The NCSBN and state Compact administrators describe the following benefits of the Compact:
108
• expands access to care;
• enables telehealth practice (including triage, call centers, case managers);
• facilitates disaster relief;
• provides support for nurse spouses in military families
• facilitates online nursing education;
• is cost effective for nurses and employers;
107
Oregon State Board of Nursing. (Sept. 30, 2022). Adopt rules related to nurse intern licensure and practice per HB 4003 – 2022. Retrieved
October 18, 2022 from https://www.oregon.gov/osbn/Documents/Notice_Div41_RuleHearing.pdf.
108
https://nursecompact.com/Updated_onepaged_NLC.pdf; https://www.ncsbn.org/NLC-Webinar-NewGrads-Jan2021.pdf; &
https://www.nursecompact.com/Updated_Legislator_FAQ.pdf

Future of Oregon’s Nursing Workforce
66
• addresses access for rural populations and areas of health care shortages;
• facilitates transport nursing;
• enables facility staffing – travel nursing;
• enhances mobility for nurses residing near borders and practicing in adjacent states;
• provides administrative efficiency; and
• offers flexible licensure (i.e., nurses may still obtain a single-state license, if ineligible for a multi-state
license).
There is limited academic literature published on the impact of the Compact. One study found no
impact of Compact adoption on labor force participation, employment levels, hours worked, or nurse
wages. It also found “little evidence that the labor supply or mobility of nurses increased following the
adoption of the Compact” in the nurses’ home state, even among nurses who lived in counties
bordering other Compact states who were potentially most affected by the Compact.
109
Another study
found an 11 percent increase in job-to-job movement (or “job flows”) upon joining the Compact from
Compact-to-Compact states and an 11 percent decrease in job flows from Compact-to-non-Compact
states.
110
It is generally recognized that the Compact does not increase the size of the overall nursing workforce,
but it is a policy solution that addresses short-term staffing needs and facilitates telehealth.
111
It also
could be beneficial during emergencies. Although nurses licensed in other states could practice in
Oregon through emergency provisions, those nurses were not under the supervision of the OSBN and
the OSBN could not initiate disciplinary processes. If those nurses had been practicing in Oregon
through the Compact, OSBN would have had authority to oversee their practice and initiate disciplinary
action if necessary.
Currently, there are 35 states that have implemented Compact legislation with more than two million
nurses living in these states.
112
Oregon, however, is not a Compact state. The main effect of the
Compact is that it addresses licensure portability issues; it removes the administrative barriers
associated with state boards of nursing having to adjudicate each application for licensure endorsement
from nurses licensed in another state. In interviews, key informants generally expressed support for
Oregon joining the Compact. However, there are several factors to consider when weighing the
decision to enact legislation to join the Compact:
109
DePasquale, C., & Stange, K. (2016). Labor supply effects of occupational regulation: Evidence from the nurse licensure compact (No.
w22344). Cambridge, MA: National Bureau of Economic Research.
110
Ghani, A. A. (2019). The impact of the nurse licensing compact on inter-state job mobility in the United States. In OECD economic survey
of the United States: Key research findings.
111
Lasater, K. B., Aiken, L. H., Sloane, D. M., French, R., Martin, B., Reneau, K., Alexander, M. & McHugh, M. D. (2021). Chronic hospital
nurse understaffing meets COVID-19: an observational study. BMJ Quality & Safety, 30(8), 639-647.
112
National Council of State Boards of Nursing. NLC Fact Sheets & Resources. https://www.ncsbn.org/compacts/nurse-licensure-compact/nlc-
toolkit/nlc-fact-sheets.page.

Future of Oregon’s Nursing Workforce
67
• There has been rising concern about fraudulent nursing education programs and false transcripts;
113
participation in the Compact may increase the risk of unqualified individuals practicing in Oregon.
• OSBN would lose approximately $700,000 in revenues from licensing fees that would no longer be
paid by nurses practicing under the Compact.
• OSBN may face higher administrative costs to manage two tracks of licensure (Oregon-only and
multi-state).
• OSBN and OHA would have less information about nurses practicing in the state because surveys
now conducted through the licensing and renewal process would not be completed by nurses with a
Compact license.
113
See, for example, https://www.fiercehealthcare.com/regulatory/doj-accuses-former-nursing-school-operators-selling-fraudulent-transcripts-
diplomas and https://www.cbs19news.com/story/44325901/nursing-school-operators-charged-with-selling-bogus-diplomas.

Future of Oregon’s Nursing Workforce
68
Conclusions and Recommendations
Conclusions
The capacity and resilience of Oregon’s nursing workforce have been severely stressed by the COVID-
19 pandemic, exacerbating pre-existing problems. Oregon is not alone in this experience; many of the
challenges observed in data and heard in interviews can be found in other states. Some of the most
important findings of this study include:
• Widespread nursing shortages are being reported, and there are multiple causes of these shortages.
There are reports of nurses retiring early, reducing their working hours, and seeking positions that
allow remote work, such as telehealth.
o Changes in nurse supply are linked to high rates of burnout among nurses, which was a
concern before the COVID-19 pandemic. Both nurses themselves and their employers have
concerns about nurse burnout and employers are deeply concerned about how to address the
situation.
o The main causes of nursing shortages differ across regions of the state and by type of health
care setting.
o There is little data available to assess the extent and depth of nursing shortages, or about the
extent to which nurses have left the profession.
• Nurse workload is a concern among both nurses and their employers. Oregon’s nurse staffing law
was intended to create collaborative processes to ensure adequate staffing for high quality patient
care. There was agreement that the regulations are not fully achieving their goal, but there were
differences in opinion about why this is the case.
o Some concerns were raised about the complexity of the survey process and perceptions that
enforcement was not as rigorous as desired.
o There has not been any objective evaluation of the effectiveness of the law’s impact on nurse
staffing, nurse workloads, or patient outcomes.
o Recent data indicate that nurse staffing in Oregon hospitals is higher than the national average,
but nurses nonetheless attribute a great deal of their stress and burnout to heavy workloads.
• Growth in new enrollments in Oregon RN education programs has slowed over the past three years
and LPN enrollments also have declined. Education programs struggle to grow due to difficulty
recruiting faculty and finding clinical placements for students.
o Faculty shortages were attributed by many people to low salaries paid to nursing faculty
compared with salaries that can be received for clinical work.
o Shortages of clinical placements were attributed to several factors, including general shortages
of nurses and the need to dedicate the time of experienced nurses toward onboarding newly-
hired new graduates.
o Applications to RN education programs have declined over the past four years; however, it is
not known why.

Future of Oregon’s Nursing Workforce
69
o Oregon is heavily reliant on nurses educated in other states because of its relatively limited
education capacity.
• Oregon’s licensed nurse workforce is not as diverse as the state’s population, although the current
nursing student population more closely resembles the racial/ethnic diversity of the state.
o The CNA and LPN workforces are somewhat more diverse than the total population in Oregon.
CNAs and LPNs have greater percentages of people who identify as Black/African-American
and CNAs also have a greater percentage of people who identifies as Hispanic/Latinx.
o The RN and NP workforces are less diverse than Oregon’s population, with under-
representation of people who identify as Hispanic/Latinx, Black/African-American, Asian, and
American Indian/Alaska Native.
o RN students have become more diverse over time, and recently-graduated RNs more closely
resemble Oregon’s population except for people who identify as Black.
o LPN students have also become more diverse over time, although people who identify as
Hispanic/Latinx remain under-represented.
Recommendations
The recommendations we offer will not provide immediate relief to the challenges Oregon now faces
with its nursing workforce. Multiple actions must be considered and simultaneously implemented to
make long-term progress toward a sustainable, skilled, and satisfied nursing workforce.
Our recommendations are organized by domain of concern.
1. Workforce retention. Health care organizations must take responsibility for retaining their
nursing workforce.
a. The mental health and well-being of nurses must be prioritized and supported. It is
essential that employers redouble their efforts to address nurse well-being and that they
create and maintain well-developed programs that create a culture of the well-being for
staff.
69
Employers can support the creation of peer support groups, provide training to
managers to recognize and address burnout among staff, and ensure that nurses take
all the paid time off they are allotted. There are numerous organizations that have
published guides and resources to help employers and educational institutions support
health care worker well-being. The National Academy of Medicine has published a
Resource Compendium for Health Care Worker Well-Being that includes evidence-
based resources to strengthen leadership behaviors, assess the well-being of staff,
assess the workplace’s wellness culture, and create a supportive culture.
114
The U.S.
Surgeon General published an Advisory on Building a Thriving Health Workforce that
provides detailed recommendations to address health care worker burnout.
89
The Joint
Commission has published several Safety Issues on increasing the resilience of the
114
National Academy of Medicine. (2022). Resource Compendium for Health Care Worker Well-Being. https://nam.edu/compendium-of-key-
resources-for-improving-clinician-well-being/.

Future of Oregon’s Nursing Workforce
70
nursing workforce.
115
OCN’s RN Well-Being Project provides links to resources for
nurses,
116
and the Oregon Wellness Program offers free counseling and education.
117
b. Employers must create healthy work environment interventions to support health and
well-being, and they need to address issues such as protection from workplace violence,
bullying, and racism head-on.
118
Components of a positive nursing work environment
include professional autonomy, adequate staff and resources, and good working
relationships with physicians and management.
81
There is a strong relationship between
nursing workload and burnout;
54,119
thus, employers need to address workload concerns
as part of the process of improving work environments to improve nurse retention and
the quality of patient care.
69
This includes staffing levels for both nursing and non-
nursing staff, as shortages of any staff lead to greater workloads for other staff. The
National Academy of Medicine’s Resource Compendium includes resources to assess
the healthiness of the work environment and advance organizational commitment to a
healthy work environment.
114
c. Oregon’s government can support employer efforts to improve employee well-being by
maintaining and expanding the Oregon Wellness Program, creating incentives for
workplace health programs, and providing resource guides and seed funding to support
development of new employer and educator programs.
2. Education pipeline. The growth of the nursing workforce begins before college and depends
on the success of nursing students in their education programs. Declines in the numbers of
applicants to RN and LPN education programs need to be reversed, and the commitment to
increasing the diversity of the nursing workforce needs to be reaffirmed.
a. Middle schools and high schools play an important role in preparing students to pursue
nursing education and diversifying the nursing workforce. A recent study of diversifying
the health professions recommended state policymakers prioritize K-12 resources for
students from socioeconomically disadvantaged backgrounds, support programs that
provide mentorship to aspiring health professionals, and create shadowing opportunities
for high school students to learn more about career opportunities in health care.
16
b. High schools and post-secondary education institutions should provide educational
resources to students to help them navigate pre-requisites and admission processes and
to help them be successful in their post-secondary education. Community colleges and
state agencies should create more pathways to leverage community colleges to offer
standardized pre-requisites. The Oregon Consortium of Nursing Education (OCNE)
115
The Joint Commission. (2019). Quick Safety Issue 50: Developing resilience to combat nurse burnout.
https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety-50-developing-resilience-
to-combat-nurse-burnout/#.Y0oZSUzMIaY.
116
Oregon Center for Nursing. (2022). RN Well-Being Project. https://oregoncenterfornursing.org/rn-well-being-project/.
117
Oregon Wellness Program. Oregon Wellness Program: Home. https://oregonwellnessprogram.org/.
118
American Nurses Association. (2022). Survey Shows Substantial Racism in Nursing. https://www.nursingworld.org/survey-on-racism.
119
Rafferty, A. M., Clarke, S. P., Coles, J., Ball, J., James, P., McKee, M., & Aiken, L. H. (2007). Outcomes of variation in hospital nurse
staffing in English hospitals: cross-sectional analysis of survey data and discharge records. International journal of nursing studies, 44(2), 175-
182.

Future of Oregon’s Nursing Workforce
71
framework should be leveraged to support standardization of pre-requisites and
streamlining RN-to-BSN education. This effort should actively engage private BSN
programs.
c. Educational institutions should develop diversity pathway programs, provide
racially/ethnically concordant mentoring, and explore holistic admissions practices. State
policymakers could provide funding to support the development, expansion, and
sustenance of these program. Moreover, there should be greater funding for direct
support to diverse students, including grants, scholarships, and stipends.
16
3. Education capacity. Oregon’s nursing education capacity does not produce all the nurses the
state needs, leaving Oregon dependent on inter-state migration. Oregon should strive to have
sufficient education capacity to meet its long-term nursing needs.
a. RN education capacity should be expanded in rural areas. Oregon’s RN education
programs should develop and expand distance-based LPN-to-RN programs and semi-
remote RN education programs. State government funds and grant programs could
facilitate this endeavor.
b. Colleges that want to have both ADN and LPN programs should consider sharing
faculty. In addition, schools should ensure their programs are structured to allow RN
students to take the LPN licensure exam while they are continuing in their RN education.
c. RN and LPN education programs should create and expand educational options and
supportive services. Many prospective students may prefer part-time programs; currently
employed CNAs and LPNs cannot easily advance their education if they must quit their
jobs for full-time education programs. In addition, education programs and other state
agencies should increase support services for RN students, particularly first-generation-
to-college and under-represented-in-health care populations.
d. The pay differential between clinical jobs and faculty positions should be redressed.
Nurses in academic roles earn up to 40 percent less than those in clinical roles.
Community college and OHSU pay scales need to ensure they pay nursing faculty
adequately. This may be challenging as these institutions value pay equity across faculty
categories; however, this goal is creating a significant barrier to growth of public nursing
programs, which are essential to serving low-income and under-represented-in-health
care students. Educational institutions should work closely with faculty unions and other
stakeholders to explore strategies to supplement nursing faculty salaries, such as
developing clinical revenue streams and pursuing grant or private sector funds. Oregon
policy makers can consider providing grant funds to support faculty hiring and
compensation.
e. State policymakers should consider providing financial incentives to faculty such as
expanded tax breaks and loan repayment.
4. Clinical experiences for students. More high-quality experiences are needed to enable the
expansion of the nurse workforce and support the education-to-practice transition.

Future of Oregon’s Nursing Workforce
72
a. Centralized clinical placement systems are needed to support nursing programs outside
the Portland area. One or more collaborative groups should be established to advanced
centralized systems statewide with local leadership and coordination.
b. Simulation laboratory facilities need expansion and educators need enhanced training to
optimize their use. Simulation facilities are difficult to access in rural areas and shared
facilities are needed. Nurse educators should receive opportunities for formal training
about the various simulation modalities and strategies, including the range from
simulation skills through clinical judgement. OSBN should collect data on simulation
offerings in Oregon nursing programs and support credentialing of faculty in simulation
modalities and technique.
c. Apprenticeships, internships, and/or residencies are needed to expand the nursing
workforce in both general nursing and specialized clinical fields. Oregon government
agencies and employers should explore strategies to fund these types of programs.
d. The “nurse intern” licensure regulations should be evaluated and the innovation be
encouraged to optimize its use. Employers and educational institutions should seek to
take full advantage of the nurse intern role.
e. Education programs should establish elective courses in specialties as partnerships
between employers and educational institutions, including community colleges.
Establishment of these programs could be incentivized with start-up funds and grants.
5. Certified Nursing Assistant education and scope of practice. CNAs provide important
services in the health care system. More can be done to advance their skills and develop career
pathways in other health occupations.
a. CNA1 vs CNA2 categories have created confusion around career pathways. OSBN
should work with employers and other stakeholders to assess whether two CNA
categories are needed and, if they are, define them as a continuous career pathway
pointing toward LPN and/or other health professions education.
b. OSBN should continue its assessment of the length of training required for CNA
certification in Oregon and provide evidence-based justification for the number of hours
required. Input from employers, including long-term care, hospitals, and ambulatory
care, should be solicited in this process.
6. Nurse Licensure Compact. OSBN and the Legislature should explore joining the Nurse
Licensure Compact with a realistic understanding of its benefits and with strategies to mitigate
its costs. If Oregon joins the Compact, it needs to identify strategies to track information about
Compact nurses working in the state. Additional funds may need to be allocated to OSBN to
ensure it can adapt to the higher administrative costs of managing two types of licenses while
losing revenue from licensing fees.
7. Nurse staffing regulations. Oregon was one of the first states in the U.S. to enact staffing
regulations that require collaborative committees to develop staffing plans in hospitals. There

Future of Oregon’s Nursing Workforce
73
are opportunities to refine Oregon’s regulations to more effectively advance the goals of high-
quality patient care and manageable nurse workloads.
a. Oregon’s Nurse Staffing Law needs to be evaluated, as there has not yet been an
objective analysis of whether the 2015 changes have achieved improvements in nurse
staffing, nurse workload, patient safety, and nurse satisfaction.
b. Revisions to the Nurse Staffing Law should aim to increase clarity, support effective
partnerships between nurse staff and management, and reduce unnecessary regulatory
burden. Enforcement of the Law should be consistent.
c. Oregon health care leaders should explore whether requirements that staffing plans
consider acuity would benefit from more structure, such as defining specific
requirements for acuity systems.
d. Exploration of establishing fixed minimum staffing requirements should be considered
with a realistic understanding of both the benefits and drawbacks. Any new staffing
regulations should consider health care staffing holistically, as nurses’ ability to practice
to the highest level of their knowledge and skill depends on having adequate support
and collaborative staff.
8. Local solutions to shortages. All strategies undertaken to address nursing shortages should
address the need for localized solutions to shortages. Recruiting and retaining nurses requires
different strategies depending on where nurses are needed in the state. Incentives to recruit
nurses to urban areas are different than those needed to recruit nurses to rural areas, and these
incentives may be related more to economic development and community building than health
care industry-specific solutions. A complete understanding of local conditions is critical to
identifying solutions to local nursing workforce needs.
a. Oregon’s policymakers and health care employers should support market research to
understand local barriers to nurse recruitment and retention.
b. Rural communities can explore developing economic opportunities for partners or
spouses of nurses, as well as invest in high-quality K-12 education and internet
infrastructure.
c. Both rural and urban communities must explore reducing the cost and increasing the
supply of housing to incentivize nurses to stay in those areas to practice.
9. Anticipating nurse shortages as a path for effective action. OSBN, OHA, HECC, OCN and
others should collaborate to advance strategies to track and predict nursing shortages and to
track the diversity of the nursing workforce. These approaches can include:
a. Regularly collecting data on employer vacancies and perceptions of the local labor
market. For example, Oregon could adopt the Sentinel Network developed by the
University of Washington, which surveys a panel of employers at frequent intervals to
measure vacancies and identify emerging shortages on a rapid basis.

Future of Oregon’s Nursing Workforce
74
b. Developing data systems that support more detailed projections of future nurse supply
and demand. Forecasting models used by other states such as California could be
adapted for Oregon, but current OSBN data systems do not generate many of the
necessary parameters for such models. The supply of licensed nurses can be modeling
using a stock-and-flow approach that accounts for different employment behaviors
across age groups. The demand for licensed nurses should be assessed using multiple
strategies, because competing conceptual frameworks exist for forecasting demand and
there is no evidence that one framework is more valid than another.
c. Investment in identifying and understanding the root causes of racial disparities in the
nursing workforce through research. This work should emphasize identifying successful
strategies to expand opportunities for marginalized populations to enter the nursing
workforce in Oregon and should involve workers from those communities in identifying
root causes and crafting solutions.
