
October 2018 (revised)
NHS Continuing Healthcare
Checklist
October 2018 (Revised)
Published March 2018

October 2018 (revised)
DH ID box
Title: NHS Continuing Healthcare Checklist
Author:
SCLGCP-SCP 25370
Document Purpose:
Guidance
Publication date:
1 March 2018
Target audience:
Health and social care professionals
Public
Contact details:
NHS Continuing Healthcare and NHS-funded Nursing Care team
Department of Health and Social Care
39 Victoria Street
London SW1H 0EU
You may re-use the text of this document (not including logos) free of charge in any format or
medium, under the terms of the Open Government Licence. To view this licence, visit
www.nationalarchives.gov.uk/doc/open-government-licence/
© Crown copyright 2016
Published to gov.uk, in PDF format only.
www.gov.uk/dh

NHS Continuing Healthcare Checklist
3
What is the Checklist and why is it used?
1. The Checklist is a screening tool which can be used in a variety of settings to help
practitioners identify individuals who may need a referral for a full assessment of eligibility for
NHS Continuing Healthcare.
2. All staff who complete the Checklist should be familiar with the principles of the National
Framework for Continuing Healthcare and NHS-funded Nursing Care and also be familiar
with the Decision Support Tool for NHS Continuing Healthcare.
3. The Checklist threshold at this stage of the process has intentionally been set low, in order
to ensure that all those who require a full assessment of eligibility for NHS Continuing
Healthcare have this opportunity.
4. There are two potential outcomes following completion of the Checklist:
a negative Checklist , meaning the individual does not require a full assessment of
eligibility and they are not eligible for NHS Continuing Healthcare; or
a positive Checklist meaning an individual now requires a full assessment of eligibility for
NHS Continuing Healthcare. It does not necessarily mean the individual is eligible for
NHS Continuing Healthcare.
When should the Checklist be completed?
5. Where there may be need for NHS Continuing Healthcare, the Checklist should normally be
completed.
6. There will be many situations where it is not necessary to complete the Checklist. See
paragraphs 91 of the National Framework and page 7 below.
7. Screening and assessment of eligibility for NHS Continuing Healthcare should be at the right
time and location for the individual and when the individual’s ongoing needs are known. This
may be in a variety of settings, although the full assessment of eligibility should normally
take place when the individual is in a community setting, preferably their own home. The
core underlying principle is that individuals should be supported to access and follow the
process that is most suitable for their current and ongoing needs. This will help practitioners
to correctly identify individuals who require a full assessment of eligibility for NHS Continuing
Healthcare.
8. To understand how NHS Continuing Healthcare interacts with hospital discharge, please
refer to paragraphs 109-117 of the National Framework.
Note:
All these tools are available electronically (as Word documents) and pages or boxes
can be expanded as necessary.
It is important to note that these are national tools and the content should not be
changed, added to or abbreviated in any way. However, CCGs may attach their logo
and additional patient identification details if necessary (e.g. adding NHS number,
etc.).
NHS Continuing Healthcare Checklist
4
Who can complete the Checklist?
9. The Checklist can be completed in by a variety of health and social care practitioners, so
long as they have been trained in its use.
What is the role of the individual in the screening process?
10. The individual should be given reasonable notice of the intention to undertake the Checklist
and have the process explained to them. They should normally be given the opportunity to
be present when the Checklist is completed, together with any representative they may
have, so that they can contribute their views about their needs.
11. Where the individual concerned has capacity, their informed consent should be obtained
before completion of the Checklist. It should be made explicit to the individual whether their
consent is being sought specifically for the completion of the Checklist and the sharing of
information for this, or for the full process, including the completion of the DST (where the
Checklist is positive). It is generally good practice to obtain consent that is valid for the whole
process, bearing in mind that the individual must be told that they can withdraw their consent
at any time. Please refer to paragraphs 72-72 of the National Framework which gives
detailed guidance on what is required for consent to be valid.
12. If there is a concern that the individual may not have capacity to give consent to the
assessment process or to the sharing of information, this should be determined in
accordance with the Mental Capacity Act 2005 and the associated code of practice. It may
be necessary for best interests decisions to be made, bearing in mind the expectation that
all who are potentially eligible for NHS Continuing Healthcare should have the opportunity to
be considered for eligibility. Guidance on the application of the Mental Capacity Act in such
situations is provided in paragraphs 74-81 of the National Framework.
How should the Checklist be completed?
13. Completion of the Checklist is intended to be relatively quick and straightforward. It is not
necessary to provide additional detailed evidence along with the completed Checklist.
14. Practitioners should compare the domain descriptors to the needs of the individual and
select level A, B or C, as appropriate, choosing whichever most closely matches the
individual. If the needs of the individual are the same or greater than anything in the A
column, then ‘A’ should be selected. Practitioners should briefly summarise the individual’s
needs which support the level chosen, recording references to evidence as appropriate.
15. A full assessment for NHS Continuing Healthcare is required if there are:
two or more domains selected in column A;
five or more domains selected in column B, or one selected in A and four in B; or
one domain selected in column A in one of the boxes marked with an asterisk (i.e.
those domains that carry a priority level in the Decision Support Tool), with any number
of selections in the other two columns.
NHS Continuing Healthcare Checklist
5
16. There may very occasionally be circumstances where a full assessment of eligibility for NHS
Continuing Healthcare is appropriate even though the individual does not apparently meet
the indicated threshold as set out above. A clear rationale must be given in such
circumstances and local protocols followed.
17. The principles in relation to ‘well-managed need’ (outlined in the Assessment of Eligibility
section of the National Framework, paragraphs 142-146) apply equally to the completion of
the Checklist as they do to the Decision Support Tool.
What happens after the Checklist?
18. Whatever the outcome of the Checklist – whether or not a referral for a full assessment of
eligibility for NHS Continuing Healthcare is considered necessary – the outcome must be
communicated clearly and in writing to the individual or their representative, as soon as is
reasonably practicable. This should include the reasons why the Checklist outcome was
reached. Normally this will be achieved by providing a copy of the Checklist.
What happens following a negative Checklist?
19. A negative Checklist means the individual does not require a full assessment of eligibility
and they are not eligible for NHS Continuing Healthcare
20. Where it can reasonably be anticipated that the individual’s needs are likely to increase in
the next three months (e.g. because of an expected deterioration in their condition), this
should be recorded and a decision made as to whether the checklist should be reviewed
within a specified period of time.
21. If an individual has been screened out following completion of the Checklist, they may ask
the CCG to reconsider the Checklist outcome. The CCG should give this request due
consideration, taking account all of the information available, and/or including additional
information from the individual or carer, though there is no obligation for the CCG to
undertake a further Checklist.
What happens following a positive Checklist?
22. A positive Checklist means that the individual requires a full assessment of eligibility for NHS
Continuing Healthcare. It does not necessarily mean that the individual will be found eligible
for NHS Continuing Healthcare (refer to paragraphs 104-107 of the National Framework).
23. An individual should not be left without appropriate support while they await the outcome of
the assessment and decision-making process.

NHS Continuing Healthcare Checklist
6
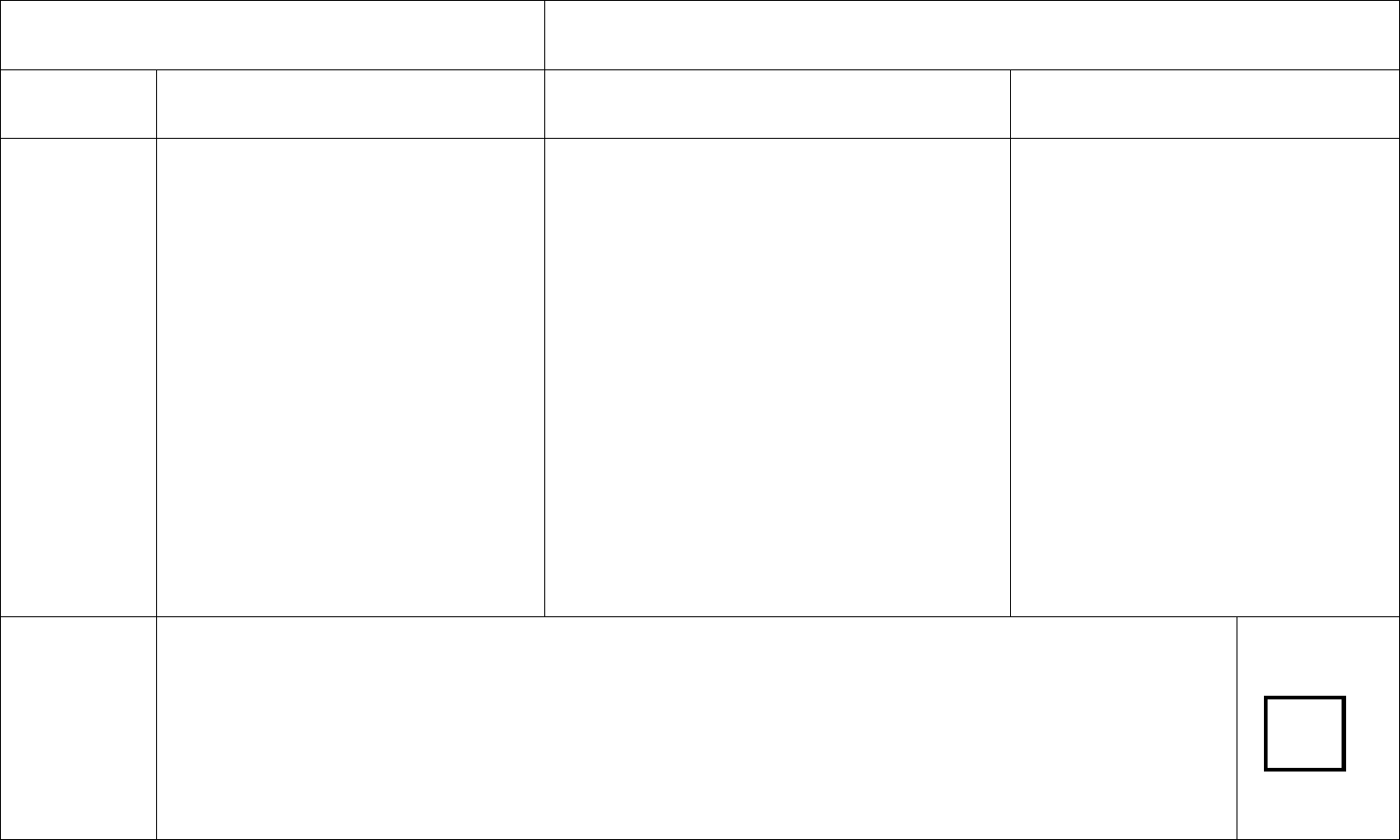
NHS Continuing Healthcare Needs Checklist
Date of completion of Checklist _____________________________
Name D.O.B.
NHS number and GP/Practice:
Permanent address and Current location (e.g. name of
telephone number hospital ward etc.)
Gender _____________________________
Please ensure that the equality monitoring form at the end of the Checklist is completed
Was the individual involved in the completion of the Checklist? Yes/No (please delete
Yes/No as appropriate)
Was the individual offered the opportunity to have a representative such as a family
member or other advocate present when the Checklist was completed? Yes/No
(please delete as appropriate)
If yes, did the representative attend the completion of the Checklist? Yes/No (please
delete as appropriate)
Please give the contact details of the representative (name, address and telephone
number).
Did you explain to the individual how their personal information will be shared with the
different organisations involved in their care, and did they consent to this information
sharing? Yes/No (please delete as appropriate)

NHS Continuing Healthcare Checklist
7
When not to screen
There will be many situations where it is not necessary to complete the Checklist.
Practitioners should review the statements below on when it may not be appropriate to screen for NHS Continuing Healthcare before
they start the process of completing the Checklist.
The situations where it is not necessary to complete the Checklist include:
a) It is clear to practitioners working in the health and care system that there is no need for NHS Continuing Healthcare at this point in
time. Where appropriate/relevant this decision and its reasons should be recorded. If there is doubt between practitioners the
Checklist should be undertaken.
b) The individual has short-term health care needs or is recovering from a temporary condition and has not yet reached their optimum
potential (although if there is doubt between practitioners about the short-term nature of the needs it may be necessary to complete
the Checklist). See paragraphs 109-117 of the National Framework for how NHS Continuing Healthcare may interact with hospital
discharge.
c) It has been agreed by the CCG that the individual should be referred directly for full assessment of eligibility for NHS Continuing
Healthcare.
d) The individual has a rapidly deteriorating condition and may be entering a terminal phase – in these situations the Fast Track
Pathway Tool should be used instead of the Checklist.
e) An individual is receiving services under Section 117 of the Mental Health Act that are meeting all of their assessed needs.
f) It has previously been decided that the individual is not eligible for NHS Continuing Healthcare and it is clear that there has been no
change in needs.
If upon review of these statements, it is deemed that it is not necessary to screen for NHS Continuing Healthcare at this time,
the decision not to complete the Checklist and its reasons should be clearly recorded in the patient’s notes.
NHS Continuing Healthcare Checklist
8
Name of individual
Date of completion
C
B
A
Breathing*
Normal breathing, no issues with shortness
of breath.
OR
Shortness of breath or a condition, which
may require the use of inhalers or a nebuliser
and has no impact on daily living activities.
OR
Episodes of breathlessness that readily
respond to management and have no impact
on daily living activities.
Shortness of breath or a condition, which may require
the use of inhalers or a nebuliser and limit some daily
living activities.
OR
Episodes of breathlessness that do not consistently
respond to management and limit some daily activities.
OR
Requires any of the following:
- low level oxygen therapy (24%);
- room air ventilators via a facial or nasal mask;
other therapeutic appliances to maintain airflow where
individual can still spontaneously breathe e.g. CPAP
(Continuous Positive Airways Pressure) to manage
obstructive apnoea during sleep.
Is able to breathe independently through a
tracheotomy that they can manage
themselves, or with the support of carers or
care workers.
OR
Breathlessness due to a condition which is
not responding to therapeutic treatment and
limits all daily living activities.
OR
A condition that requires management by a
non-invasive device to both stimulate and
maintain breathing (non-invasive positive
airway pressure, or non-invasive ventilation)
Brief
description of
need and
source
of evidence to
support the
chosen level
Respiratory rate/type. Cough/expectoration. Smoker/non smoker. Oxygen therapy/nebulisers/inhalers. BIPAP/CPAP.
Infections/pneumonia
Does the person have needs in relation to this domain?
Details of needs in relation to this domain
Details of any ventilators, inhalers, or specialist equipment
Details of any specialist involved and any advice given
Write A, B or C
below:

NHS Continuing Healthcare Checklist
9
How do breathing symptoms impact on day to day activities
Details of medications to manage symptoms – effectiveness of medications

October 2018 (revised)
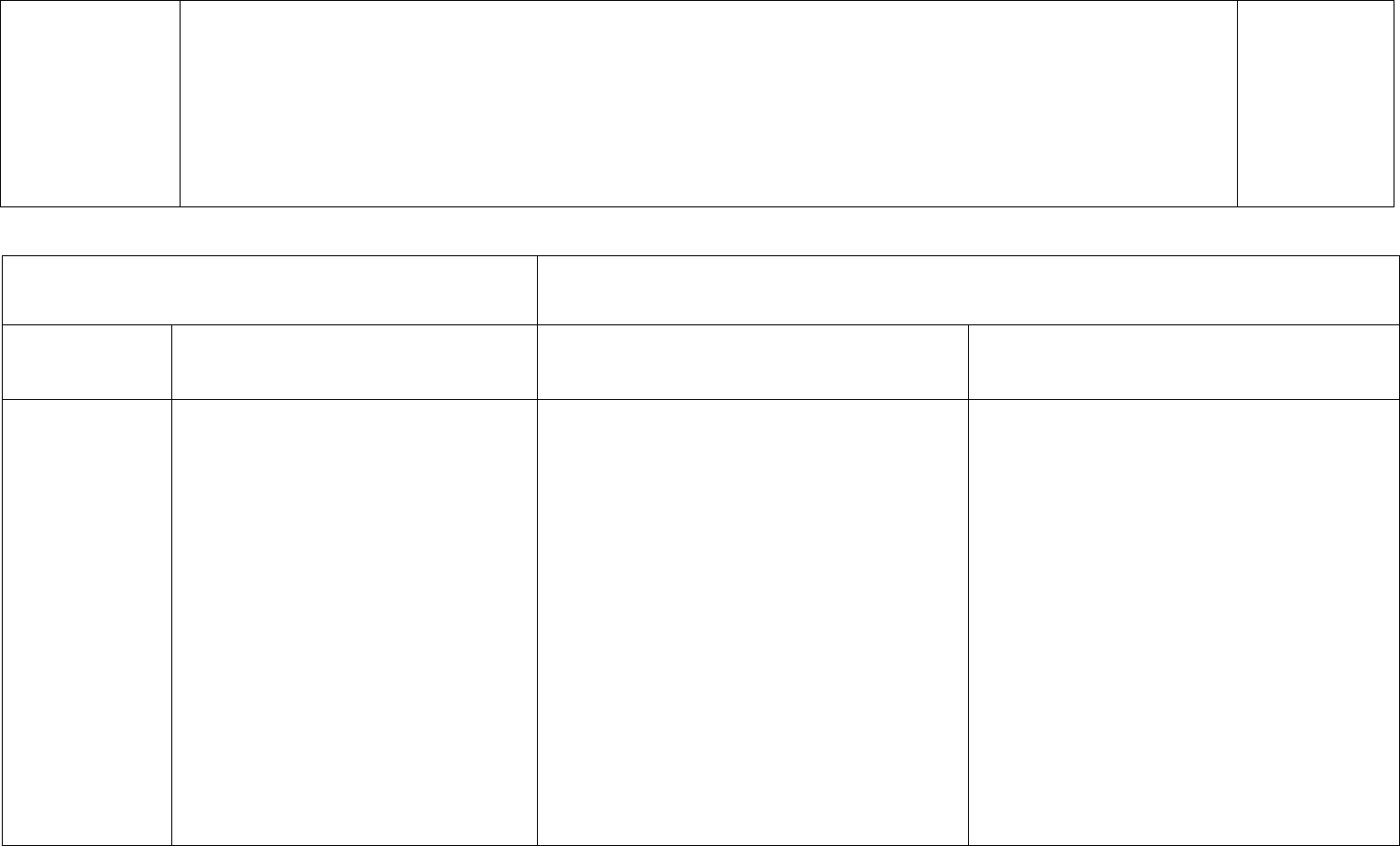
Name of individual
Date of completion
C
B
A
Nutrition
Able to take adequate food and drink by
mouth to meet all nutritional requirements.
OR
Needs supervision, prompting with meals, or
may need feeding and/or a special diet (for
example to manage food
intolerances/allergies).
OR
Able to take food and drink by mouth but
requires additional/supplementary feeding.
Needs feeding to ensure adequate intake of
food and takes a long time (half an hour or
more), including liquidised feed.
OR
Unable to take any food and drink by mouth,
but all nutritional requirements are being
adequately maintained by artificial means, for
example via a non-problematic PEG.
Dysphagia requiring skilled intervention to ensure
adequate nutrition/hydration and minimise the risk
of choking and aspiration to maintain airway.
OR
Subcutaneous fluids that are managed by the
individual or specifically trained carers or care
workers.
OR
Nutritional status ‘at risk’ and may be associated
with unintended, significant weight loss.
OR
Significant weight loss or gain due to an identified
eating disorder.
OR
Problems relating to a feeding device (e.g. PEG)
that require skilled assessment and review.
Brief description
of need and
source
of evidence to
support the
chosen level
Nutritional risk assessment, identified weight loss, ability to take diet and fluids. SALT/Dietician involvement.
PEG – Routine/Problematic
Are there any special (health related) special dietary requirements.
Is the person able to eat independently, or with assistance and do they take a long time to eat a meal?
Evidence of any changes in weight/BMI reasons for any changes in weight – eg lifestyle change/diet change
Malnutrition Universal Screening Tool (MUST) score if known
Is a specialist involved
Write A, B or C
below:

NHS Continuing Healthcare Checklist
11
What advice has been given by a specialist
What skilled interventions are required
Is PEG in use – who provides the care
Name of individual
Date of completion
C
B
A
Continence
Continent of urine and faeces.
OR
Continence care is routine on a day-to-day
basis.
OR
Incontinence of urine managed through, for
example, medication, regular toileting, use of
penile sheaths, etc.
AND
Is able to maintain full control over bowel
movements or has a stable stoma, or may
have occasional faecal
incontinence/constipation.
Continence care is routine but requires
monitoring to minimise risks, for example
those associated with urinary catheters,
double incontinence, chronic urinary tract
infections and/or the management of
constipation or other bowel problems.
Continence care is problematic and requires
timely and skilled intervention, beyond routine
care. (for example frequent bladder wash
outs/irrigation, manual evacuations, frequent re-
catheterisation).

NHS Continuing Healthcare Checklist
12
Brief description
of need and
source
of evidence to
support the
chosen level
Management of constipation/diarrhoea, stoma/catheter care – toileting needs
Does the person have needs in this domain?
Details of needs
Details of specialist continence management
Is there a catheter? (What type if known)
Frequency of constipation
details of any treatment for constipation
Use of medications for bladder control
History of UTI’s – frequency/management/severity
Write A, B or C
below:

NHS Continuing Healthcare Checklist
13
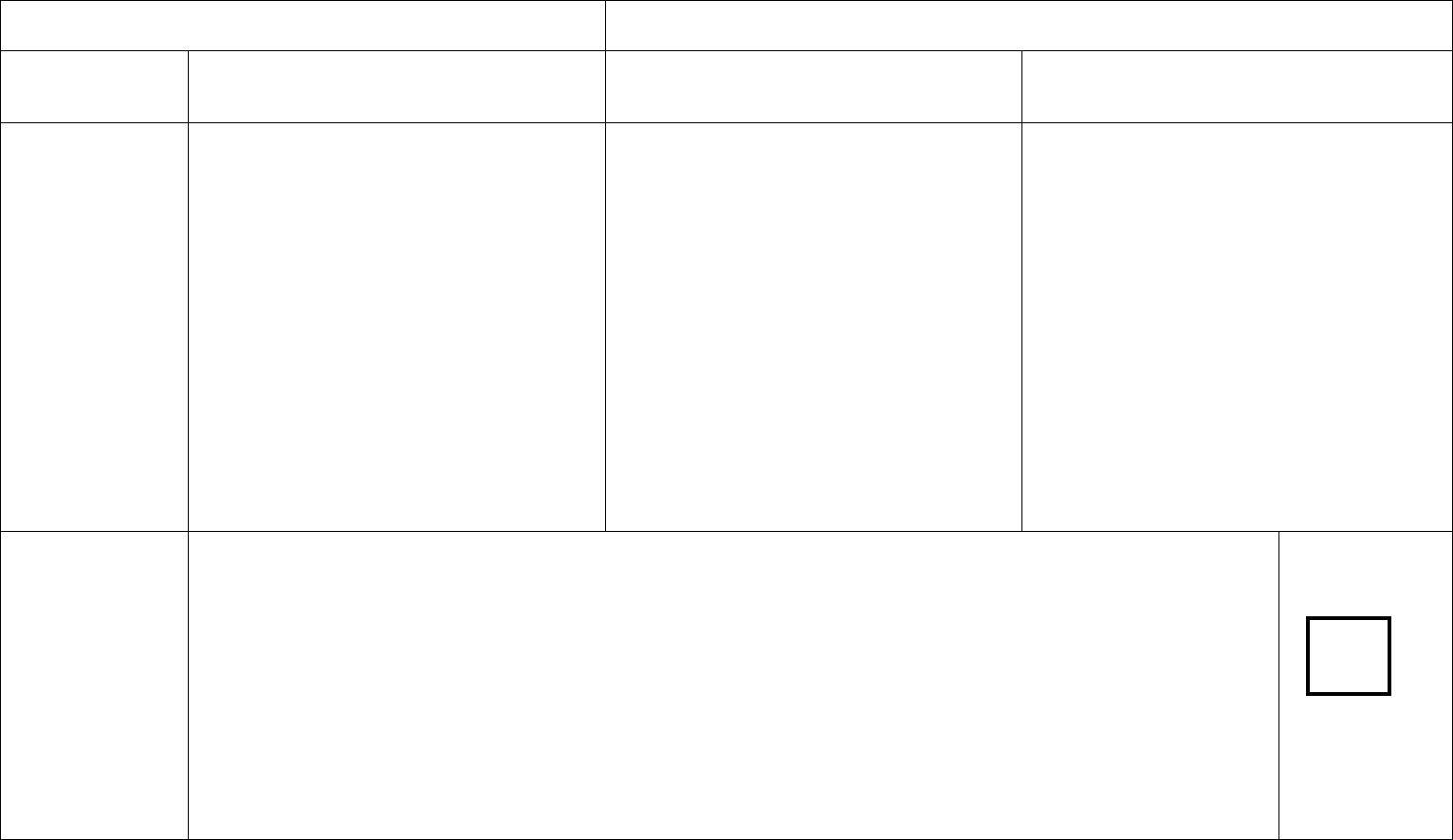
Name of individual
Date of completion
C
B
A
Skin integrity
No risk of pressure damage or skin condition.
OR
Risk of skin breakdown which requires
preventative intervention once a day or less than
daily, without which skin integrity would break
down.
OR
Evidence of pressure damage and/or pressure
ulcer(s) either with ‘discolouration of intact skin’
or a minor wound.
OR
A skin condition that requires monitoring or
reassessment less than daily and that is
responding to treatment or does not currently
require treatment.
Risk of skin breakdown which requires
preventative intervention several times each
day, without which skin integrity would break
down.
OR
Pressure damage or open wound(s), pressure
ulcer(s) with ‘partial thickness skin loss
involving epidermis and/or dermis’, which is
responding to treatment.
OR
An identified skin condition that requires a
minimum of daily treatment, or daily
monitoring/reassessment to ensure that it is
responding to treatment
Pressure damage or open wound(s),
pressure ulcer(s) with ‘partial thickness skin
loss involving epidermis and/or dermis’,
which is not responding to treatment.
OR
Pressure damage or open wound(s),
pressure ulcer(s) with ‘full thickness skin loss
involving damage or necrosis to
subcutaneous tissue, but not extending to
underlying bone, tendon or joint capsule’,
which is responding to treatment.
OR
Specialist dressing regime in place which is
responding to treatment.
Brief description
of need and
source
of evidence to
support the
chosen level
Waterlow/Braden score. Pressure relieving equipment, wound care, TVN involvement
Does the person have needs in relation to this domain?
Details of risk assessment
What are the preventative measures in place – ie repositioning (how frequent), pressure relieving
equipment
Write A, B or C
below:
NHS Continuing Healthcare Checklist
14
Details of wounds – ie grading of pressure sore, description of wound, wound care plan, what dressings
are used, is the wound showing signs of responding to treatment
Any specialist involvement – ie Tissue Viability Nurse –
Any other skin condition requiring treatment
Name of individual
Date of completion
C
B
A
Mobility
Independently mobile.
OR
Able to weight bear but needs some
assistance and/or requires mobility
equipment for daily living.
Not able to consistently weight bear.
OR
Completely unable to weight bear but is able to
assist or cooperate with transfers and/or
repositioning.
OR
In one position (bed or chair) for majority of the
time but is able to cooperate and assist carers or
care workers.
OR
At moderate risk of falls (as evidenced in a falls
history or risk assessment)
Completely unable to weight bear and is unable to
assist or cooperate with transfers and/or
repositioning.
OR
Due to risk of physical harm or loss of muscle
tone or pain on movement needs careful
positioning and is unable to cooperate.
OR
At a high risk of falls (as evidenced in a falls
history and risk assessment).
OR
Involuntary spasms or contractures placing the
individual or others at risk.

NHS Continuing Healthcare Checklist
15
Brief description
of need and
source
of evidence to
support the
chosen level
Use of mobility aids, FRASE score and recent falls with dates. Ability to assist with re
positioning/spasms/contractures
Does the person have mobility issues
Does the person use mobility aids, if so what
Does the person require hoisting or transfer aids, if so what?
What is the level and frequency of supervision required
What skill level is required
Is the person able to weight bear, reposition themselves or able to assist with transfers?
Details of level of assistance is required
Is there a risk assessment – if so what tool has been used and what is the identified level of risk
Falls risk assessment = frequency/nature of falls
Falls monitoring chart
Use of alarm/crash mats
Write A, B or C
below:

NHS Continuing Healthcare Checklist
16
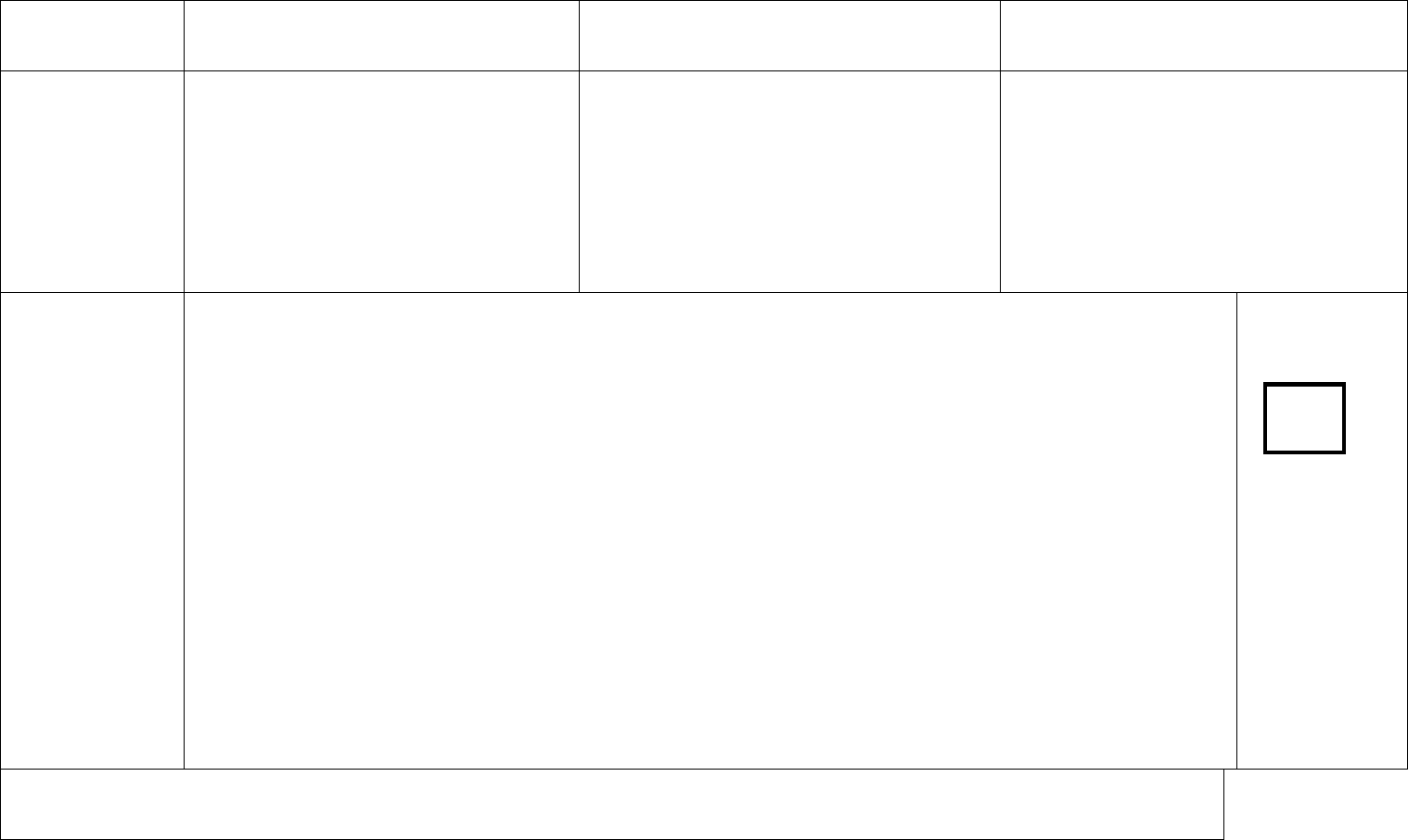
Name of individual
Date of completion
C
B
A
Communication
Able to communicate clearly, verbally or non-
verbally. Has a good understanding of their
primary language. May require translation if
English is not their first language.
OR
Needs assistance to communicate their
needs. Special effort may be needed to
ensure accurate interpretation of needs or
additional support may be needed either
visually, through touch or with hearing.
Communication about needs is difficult to
understand or interpret or the individual is
sometimes unable to reliably communicate,
even when assisted. Carers or care workers
may be able to anticipate needs through non-
verbal signs due to familiarity with the
individual.
Unable to reliably communicate their needs at
any time and in any way, even when all
practicable steps to assist them have been
taken. The individual has to have most of their
needs anticipated because of their inability to
communicate them.
Brief description
of need and
source
of evidence to
support the
chosen level
Social interaction, sensory impairment, ability to express basic needs verbally/non verbally
Are there needs in this
domain?
Can the person communicate? How? Verbally/non-verbally/hand gestures/assisted technology
Can they communicate their needs? What is the quality of their communication – is it coherent
Can they consistently communicate
Do they have cognitive impairment?
How does cognitive impairment impair their communication?
Can they communicate through non-verbal communication
Do they use communication aids
Do carers need to anticipate all needs due to communication difficulties /Details of advice from Speech and Language Therapy.
Write A, B or C
below:
NHS Continuing Healthcare Checklist
17
Name of individual
Date of completion
C
B
A
Psychological/
Emotional
Psychological and emotional needs are not
having an impact on their health and well-
being.
OR
Mood disturbance or anxiety symptoms or
periods of distress, which are having an impact
on their health and/or well-being but respond
to prompts, distraction and/or reassurance.
OR
Requires prompts to motivate self towards
activity and to engage them in care planning,
support and/or daily activities.
Mood disturbance, hallucinations or anxiety
symptoms or periods of distress which do not
readily respond to prompts, distraction and/or
reassurance and have an increasing impact on
the individual’s health and/or well-being.
OR
Due to their psychological or emotional state
the individual has withdrawn from most
attempts to engage them in support, care
planning and/or daily activities.
Mood disturbance, hallucinations or anxiety
symptoms or periods of distress that have a
severe impact on the individual’s health and/or
well-being.
OR
Due to their psychological or emotional state the
individual has withdrawn from any attempts to
engage them in care planning, support and/or
daily activities.
Brief description
of need and
source
of evidence to
support the
chosen level
Triggers, Responses, Frequency, Intervention.
Does the person have needs in this domain?
Does the person have a current diagnosis of depression or anxiety?
Does the person experience Hallucinations or Delusions?
Does the person have a mental disorder currently under treatment?
Does the person have psychological needs?
Does the person experience periods of distress?
Write A, B or C
below:

NHS Continuing Healthcare Checklist
18
If yes to one or more of the above
What is the frequency?
Are they able to be reassured
Are they withdrawn due to their psychological or cognitive state?
Are they on medication for this need?
Is there a risk assessment?
What risks have been as identified in care plans?
Is there a specialist involved (details)

NHS Continuing Healthcare Checklist
19
Name of individual
Date of completion
C
B
A
Cognition
No evidence of impairment, confusion or
disorientation.
OR
Cognitive impairment which requires some
supervision, prompting or assistance with
more complex activities of daily living, such
as finance and medication, but awareness of
basic risks that affect their safety is evident.
OR
Occasional difficulty with memory and
decisions/choices requiring support,
prompting or assistance. However, the
individual has insight into their impairment.
Cognitive impairment (which may include
some memory issues) that requires some
supervision, prompting and/or assistance with
basic care needs and daily living activities.
Some awareness of needs and basic risks is
evident.
The individual is usually able to make choices
appropriate to needs with assistance.
However, the individual has limited ability even
with supervision, prompting or assistance to
make decisions about some aspects of their
lives, which consequently puts them at some
risk of harm, neglect or health deterioration.
Cognitive impairment that could for example
include frequent short-term memory issues and
maybe disorientation to time and place. The
individual has awareness of only a limited range
of needs and basic risks. Although they may be
able to make some choices appropriate to need
on a limited range of issues, they are unable to
do so on most issues, even with supervision,
prompting or assistance.
The individual finds it difficult, even with
supervision, prompting or assistance, to make
decisions about key aspects of their lives, which
consequently puts them at high risk of harm,
neglect or health deterioration.
Brief description
of need and
source
of evidence to
support the
chosen level
Supporting evidence, identified need (awareness and understanding)
Does the person have needs related to this domain?
What are the needs?
Are they oriented to Time Place and Person?
What is their impairment in Short or long term memory and how does it affect them?
Do they recognise family and or carers
Do they have a formal cognitive test such as Mini Mental State Examination (MMSE)
Do they have a formal diagnosis relevant to cognitive issues if so what is it and when was it given
Write A, B or C
below:

NHS Continuing Healthcare Checklist
20
And by whom?
Do they have input from a specialist service?
Is there a DOL in place
What is the persons level of understanding regarding risk
Name of individual
Date of completion
C
B
A
Behaviour*
No evidence of ‘challenging’ behaviour.
OR
Some incidents of ‘challenging’ behaviour.
A risk assessment indicates that the
behaviour does not pose a risk to self,
others or property or create a barrier to
intervention. The individual is compliant
with all aspects of their care.
‘Challenging’ behaviour that follows a
predictable pattern. The risk assessment
indicates a pattern of behaviour that can be
managed by skilled carers or care workers who
are able to maintain a level of behaviour that
does not pose a risk to self, others or property.
The individual is nearly always compliant with
care.
‘Challenging’ behaviour of type and/or frequency
that poses a predictable risk to self, others or
property. The risk assessment indicates that
planned interventions are effective in minimising
but not always eliminating risks. Compliance is
variable but usually responsive to planned
interventions.

NHS Continuing Healthcare Checklist
21
Brief description
of need and
source
of evidence to
support the
chosen level
Supporting evidence, identified need (include trigger points, frequency, interventions, verbal/physical
aggression)
Are there any behavioural problems:
Describe the behaviours:
What problem do they pose:
How frequently does the behaviour occur ( evidence from incident forms, daily records and behaviour
management plans)
What is the duration of the behaviour:
How frequent is the behaviour:
How is the behaviour managed:
Is there any specialist involvement – ie psychiatrist
Details of section 117 if appropriate
What level of risk is identified:
What would happen if the behaviour was not managed
Include copies of:
Risk assessment
Behavioural charts
Use of prn/rescue medication – frequency of use
Write A, B or C
below:

NHS Continuing Healthcare Checklist
22
Name of individual
Date of completion
C
B
A
Drug therapies
and medication:
symptom control*
Symptoms are managed effectively and
without any problems, and medication is
not resulting in any unmanageable side-
effects.
OR
Requires supervision/administration of
and/or prompting with medication but
shows compliance with medication regime.
OR
Mild pain that is predictable and/or is
associated with certain activities of daily
living; pain and other symptoms do not
have an impact on the provision of care.
Requires the administration of medication (by
a registered nurse, carer or care worker) due
to:
– non-compliance, or
– type of medication (for example insulin); or
– route of medication (for example PEG).
OR
Moderate pain which follows a predictable
pattern; or other symptoms which are having a
moderate effect on other domains or on the
provision of care.
Requires administration and monitoring of
medication regime by a registered nurse, carer or
care worker specifically trained for this task
because there are risks associated with the
potential fluctuation of the medical condition or
mental state, or risks regarding the effectiveness
of the medication or the potential nature or
severity of side-effects. However, with such
monitoring the condition is usually non-
problematic to manage.
OR
Moderate pain or other symptoms which is/are
having a significant effect on other domains or on
the provision of care.

NHS Continuing Healthcare Checklist
23
Brief description
of need and
source
of evidence to
support the
chosen level
Administration of medicines/self medicating. Compliancy issues. Routine PEG, S/C, inhalers. Pain-
type/severity/treatment/effectiveness
.
Does the person have needs in relation to this domain
Details of medication
Can the person self-medicate?
Does the medication / route of medication administration require some training (eg PEG or insulin
injections) but can then be administered routinely in accordance with Medication Administration
Charts/prescription
Does the medication need to be administered by a registered nurse or carer specially trained due to the
complexity of the route or other factors (not relating to a registered requirement of a provider)
Who administers the medication
Is the client compliant with the regime
Any issues with pain –what is the nature of the pain/ what medication is used and details
What impact does pain have on day to day activities/ how is the pain managed/is pain relief effective
Write A, B or C
below:
Name of individual
Date of completion
NHS Continuing Healthcare Checklist
24
C
B
A
Altered states of
consciousness*
No evidence of altered states of
consciousness (ASC).
OR
History of ASC but effectively managed and
there is a low risk of harm.
Occasional (monthly or less frequently)
episodes of ASC that require the supervision of
a carer or care worker to minimise the risk of
harm.
Frequent episodes of ASC that require the
supervision of a carer or care worker to
minimise the risk of harm.
OR
Occasional ASCs that require skilled
intervention to reduce the risk of harm.
Brief description
of need and
source
of evidence to
support the
chosen level
Seizures – types/frequency. Effectiveness of medication. Hospital admissions. Coma – Glasgow coma
scale.
Does the person have needs in relation to this domain?
Details
Include seizure charts or care records
Is PRN medication required frequency of use and under what protocol
History of stroke would be included in C
What routine medication is given
Frequency of hospital admissions (due to seizures)
Write A, B or C
below:

NHS Continuing Healthcare Checklist
25
Please highlight the outcome indicated by the Checklist:
1. Referral for full assessment for NHS Continuing Healthcare is necessary.
or
2. No referral for full assessment for NHS Continuing Healthcare is necessary.
Rationale for decision
Please send this completed Checklist to the CCG without delay.
Name(s) and signature(s) of assessor(s) Date
Contact details of assessors (name, role, organisation, telephone number, email address)

NHS Continuing Healthcare Checklist
26
About you – equality monitoring
Please provide us with some information about yourself. This will help us to understand whether
people are receiving fair and equal access to NHS continuing healthcare. All the information you
provide will be kept completely confidential by the Clinical Commissioning Group. No identifiable
information about you will be passed on to any other bodies, members of the public or press.
1 What is your sex?
Tick one box only.
Male
Female
In another way
Prefer not to answer
2 Which age group applies to you?
Tick one box only.
18-24
25-34
35-44
45-54
55-64
65-74
75-84
85+
Prefer not to answer
3 Do you have a disability as defined by
the Disability Discrimination Act (DDA)?
Tick one box only.
The Disability Discrimination Act (DDA)
defines a person with a disability as someone
who has a physical or mental impairment that
has a substantial and long-term adverse
effect on his or her ability to carry out normal
day to day activities.
Yes
No
Prefer not to answer
4 What is your ethnic group?
Tick one box only.
A White
English/Welsh/Scottish/Northern
Irish/British
Irish
Gypsy or Irish Traveller
Any other White background, write below
B Mixed
White and Black Caribbean
White and Black African
White and Asian
Any other Mixed background, write below
C Asian, or Asian British
Indian
Pakistani
Bangladeshi
Chinese
Any other Asian background, write below
D Black, or Black British
Caribbean
African
Any other Black background, write below
E Other ethnic group
Arab
Any other ethnic group, write below
Prefer not to answer

NHS Continuing Healthcare Checklist
27
5 What is your religion or belief?
Tick one box only.
Christian includes Church of England/Wales/
Scotland, Catholic, Protestant and
all other Christian denominations.
6 Which of the following best describes your
sexual orientation?
Tick one box only.
Heterosexual or Straight
Gay or Lesbian
Bisexual
Prefer not to answer
Other, write below
None
Christian
Buddhist
Hindu
Jewish
Muslim
Sikh
Prefer not to answer
Any other religion, write below
