
AuduBon-Bons
Bite Sized
Learning for Clinic
BREAST EXAM:
DOCUMENTATION OF BENIGN EXAM
Week 26
Prepared by Stephanie Warsheski, MD
Homework Assignment:
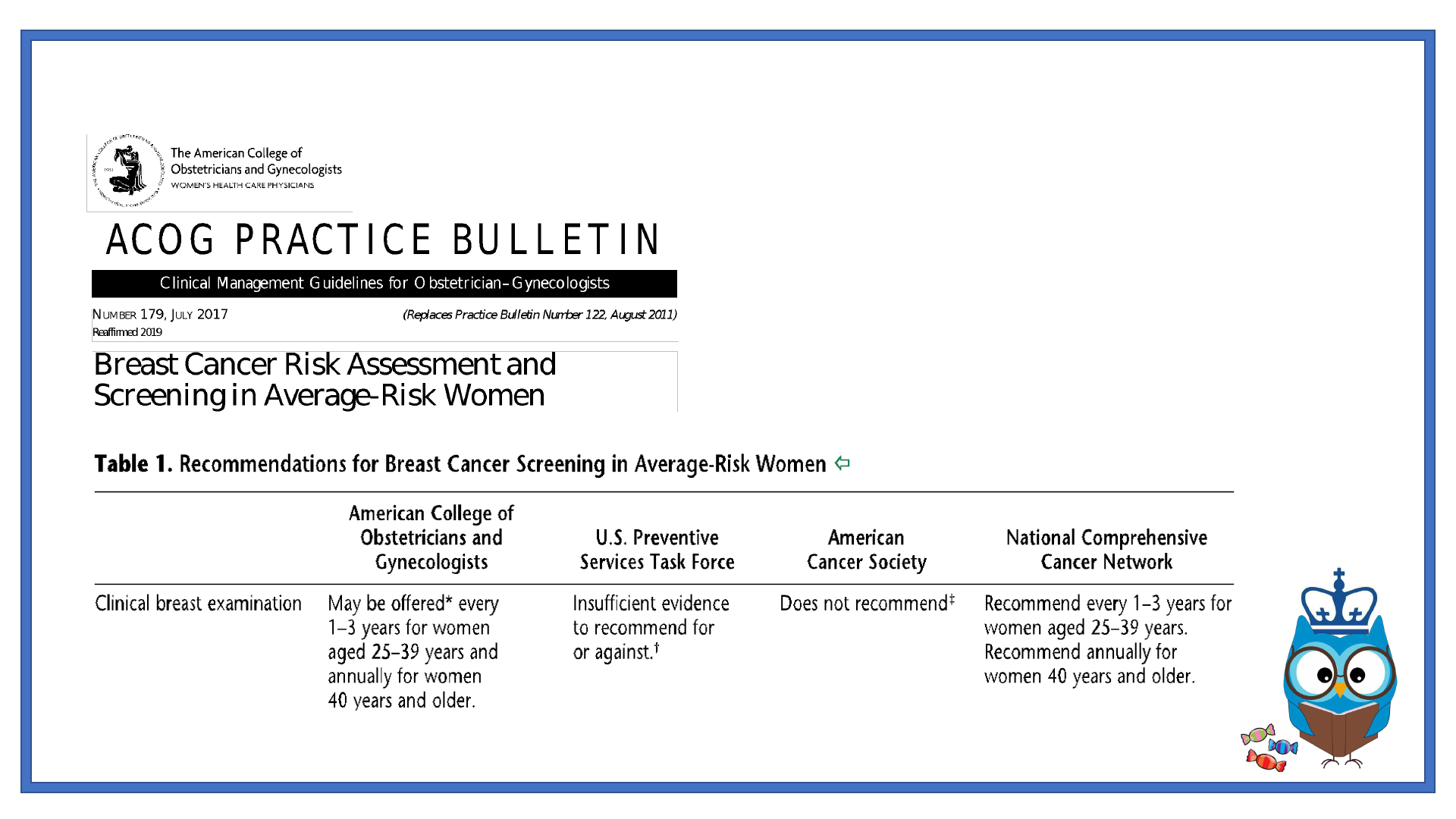
ACOG Practice Bulletin #179
Breast Cancer Risk Assessment and Screening in
Average-Risk Women
LEARNING OBJECTIVES
• To understand indications and guidelines for the clinical breast exam
• To review components of a complete clinical breast exam
• To effectively document a benign breast exam
CASE VIGNETTE
• A 38 y.o. G2P2 woman presents to clinic requesting a breast
examination. She states her friend was recently diagnosed with
breast cancer and she wants to make sure she doesn’t have it too.
• She has no complaints.

FOCUSED HISTORY
What elements of this patient’s history are most relevant?
• OBHx: FT NSVD x 2
• GYNHx: Menarche at 11 y.o., regular menses q month, lasting 4-5 days, LMP
1 week ago
• PMHx: Denies
• PSHx: Denies
• Meds: None
• All: NKDA
• SocHx: Denies use of tobacco, illicit drugs, + social ETOH
• FamHx: Denies h/o breast, ovarian cancer

Breast cancer risk assessment and screening in average-risk women. Practice Bulletin No. 179.
American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;130:e1–16.

CLINICAL ANATOMY
https://obgynkey.com/the-breast/
INDICATIONS

TECHNIQUE - INSPECTION
• Seated position facing examiner
• Hands on hips
• Hands raised above head
• Assess
• Size
• Shape
• Symmetry
• Nipples
• Size
• Shape
• Texture
• Color
https://obgynkey.com/breast-disorders-2/

TECHNIQUE - PALPATION
• Use pads of the middle 3 fingers
of one hand
• Press downward using circular
motions
• Apply steady pressure, pushing
down to the level of the chest
wall
• Start with breast followed by
axillary region
https://obgynkey.com/breast-disorders-2/

PHYSICAL EXAM, DOCUMENTATION
• Symmetry
• Symmetrical or asymmetrical
• Shape
• Ptotic, pendulous, presence of scars or deformities with description
• Texture
• Soft, nodular, fibrocystic, dense, presence of inframammary ridge in large breasts
• Masses
• Absent
• Present: size, consistency, distance from areolar edge, clock position
• Nipple-areolar complex
• Pink, brown, everted, inverted, discharge present/absent with description, presence of dry, scaly texture
concerning for Paget’s disease
• Skin
• Warm, dry, presence/absence of erythema, edema, peau d’orange appearance, open sores, draining fluid
collections

https://aestheticsjournal.com/feature/lifting-the-breast-with-pdo-threads
https://coremedicalclinics.co.uk/inverted-
nipple-correction/
Karakas C. Paget's disease of the breast. J Carcinog [serial online] 2011 [cited 2019 Sep 4];10:31.
Available from: http://www.carcinogenesis.com/text.asp?2011/10/1/31/90676
http://earthwidesurgicalfoundation.blogspot.com/20
12/01/what-is-diagnosis_25.html

Screening policies should be implemented and focus on high-risk populations that are less
likely to be screened for breast cancer by trained health care providers.
SOCIAL DETERMINANTS OF HEALTH
Lower
rates were
associated
with:
Race: Hispanic or Latino, Asian, Native Hawaiian or Other Pacific Islander, American Indian or Alaska
Native
Age: Women ≥ 75 years
Education: High school education or less
Income: Household income ≤ $25,000
Region of Residence: Midwest
Socio-demographic factors and region of residence are significantly associated with
disparities in receiving CBE in women ≥ 18 years in the United States.

Epic .phrase
BBonBreastExam
Description: Documentation of the breast exam
The patient was examined in 2 positions. The breasts were noted
to be symmetric/asymmetric***, ptotic/pendulous/presence of
scars or deformities***, soft/nodular/fibrocystic/dense/presence of
inframammary ridge***, no masses palpated/mass present (size,
consistency, distance from areolar edge, clock position)***. The
nipple-areolar complexes were pink***, everted/inverted***,
without discharge/discharge present (describe)***, with normal
texture/with presence of dry, scaly texture***. The skin was
warm/dry/with or without erythema/edema/peau d’ orange
appearance/open sores/draining fluid collections***.

CODING AND BILLING
• Diagnostic Codes (ICD-10)
• Z12.39 Encounter for other screening for malignant neoplasm of breast

HISTORY EXAM MEDICAL DIAGNOSIS MAKING CODE APPLICABLE GUIDELINES
Problem focused:
-
Chief complaint
-
HPI (1-3)
Problem focused:
- 1 body system
Straight forward:
-
Diagnosis: minimal
-
Data: minimal
-
Risk: minimal
99201
-
Personally provided
-
Primary care exception
-
Physicians at teaching hospitals
Expanded problem focused:
-
Chief complaint
-
HPI (1-3)
-
ROS (1-3)
Expanded problem focused:
- Affected areas and others
Straight forward:
-
Diagnosis: minimal
-
Data: minimal
-
Risk: minimal
99202
-
Personally provided
-
Primary care exception
-
Physicians at teaching hospitals
Comprehensive
-
Chief complaint
-
HPI (4)
-
ROS (2-9)
-
Past, family, social history (1)
Detailed:
- 7 systems
Low:
-
Diagnosis: limited
-
Data: limited
-
Risk: low
99203
-
Personally provided
-
Primary care exception
-
Physicians at teaching hospitals
Comprehensive
-
Chief complaint
-
HPI (4+)
-
ROS (10+)
-
Past, family, social history (3)
Comprehensive:
- 8 or more systems
Moderate:
-
Diagnosis: multiple
-
Data: moderate
-
Risk: moderate
99204
-
Personally provided
-
Physicians at teaching hospitals
Comprehensive
-
Chief complaint
-
HPI (4+)
-
ROS (10+)
-
Past, family, social history (3)
Comprehensive:
- 8 or more systems
High:
-
Diagnosis: extended
-
Data: extended
-
Risk: high
99205
-
Personally provided
-
Physicians at teaching
hospitals
CODING AND BILLING – NEW PATIENT

HISTORY
EXAM
MEDICAL DIAGNOSIS MAKING
CODE
APPLICABLE GUIDELINES
Expanded problem focused:
-
Chief complaint
-
HPI (1-3)
Problem focused:
-
1 body system
Straight forward:
-
Diagnosis: minimal
-
Data: minimal
-
Risk: minimal
99212
-
Personally provided
-
Primary care exception
-
Physicians at teaching hospitals
Expanded problem focused:
-
Chief complaint
-
HPI (1-3)
-
ROS (1)
Expanded problem
focused:
-
Affected area and others
Low:
-
Diagnosis: limited
-
Data: limited
-
Risk: low
99213
-
Personally provided
-
Primary care exception
-
Physicians at teaching hospitals
Detailed
-
Chief complaint
-
HPI (4+)
-
ROS (10+)
-
Past, family, social history (3)
Detailed:
-
7 systems
Moderate:
-
Diagnosis: multiple
-
Data: moderate
-
Risk: moderate
99214
-
Personally provided
-
Physicians at teaching hospitals
Comprehensive
-
Chief complaint
-
HPI (4+)
-
ROS (10+)
-
Past, family, social history (2)
Comprehensive:
-
8 or more systems
High:
-
Diagnosis: extended
-
Data: extended
-
Risk: high
99215
-
Personally provided
-
Physicians at teaching
hospitals
CODING AND BILLING – ESTABLISHED PATIENT

EVIDENCE
• References
• Breast cancer risk assessment and screening in average-risk women. Practice Bulletin No.
179. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;130:e1–16.
• Breast examination. UCSD’s Practical Guide to Clinical Medicine.
https://meded.ucsd.edu/clinicalmed/breast.htm (Accessed on August 20, 2019).
• Diagnosis and management of benign breast disorders. Practice Bulletin No. 164. American
College of Obstetricians and Gynecologists. Obstet Gynecol 2016;127:e141–56.
• Henderson JA, Ferguson T. Breast Examination Techniques. [Updated 2019 Jun 7]. In:
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK459179/ (Accessed on August 20, 2019).
• Mikayla Y. Charles, et al. Disparities in receiving clinical breast examination for early
detection of breast cancer among women aged 18 years and over in the United States.
[abstract]. In: Proceedings of the Eighth AACR Conference on The Science of Health
Disparities in Racial/Ethnic Minorities and the Medically Underserved; Nov 13-16, 2015;
Atlanta, GA. Philadelphia (PA): AACR; Cancer Epidemiol Biomarkers Prev 2016;25(3
Suppl):Abstract nr B95.
