
https://doi.org/10.1177/87564793231191506
Journal of Diagnostic Medical Sonography
2023, Vol. 39(6) 561 –567
© The Author(s) 2023
Article reuse guidelines:
sagepub.com/journals-permissions
DOI: 10.1177/87564793231191506
journals.sagepub.com/home/jdm
Original Research
Biliary disorders associated with a biliary system obstruc-
tion can affect a significant portion of the world’s popula-
tion. Most biliary diseases result in the dilation of
intrahepatic and extrahepatic bile ducts. The diameter of
the common bile duct (CBD) is an important factor used
to differentiate obstructive (dilated CBD) from non-
obstructive causes of jaundice.
1
Sonography is a well-
established method for evaluating the extrahepatic biliary
system and serves as a major diagnostic tool in suspected
bile duct obstruction. To better understand the signifi-
cance of a dilated CBD, it is essential to establish the nor-
mal diameter.
1
However, establishing an accurate
reference range for the diameter of the CBD remains a
topic of debate. A reference range is needed to determine
the significance of spontaneous abnormalities or atypical
dilation. CBD diameters exceeding the upper limit of this
range can be classified as abnormal.
Traditionally, using sonography, the CBD diameter’s
upper limit is determined as 6–7.0 mm, in those individu-
als without cholecystectomy and 10 mm in post-chole-
cystectomy patients.
2
However, contrast-enhanced
abdominal computed tomography (CT) has yielded a
more prominent upper limit for diameter of the CBD. In a
1191506JDM
XXX10.1177/87564793231191506Journal of Diagnostic Medical SonographyKheiridoost Langroudi et al
research-article2023
1
Department of Radiology, Modarres Hospital, Shahid Beheshti
University of Medical Sciences, Tehran, Iran
2
Department of Radiology, Hillcrest Hospital, University of California
San Diego, San Diego, CA, USA
3
Amirkabir University of Technology, Tehran, Iran
Received January 20, 2023, and accepted for publication July 13, 2023.
Corresponding Author:
Neda Akhoundi, MD, Department of Radiology, Hillcrest Hospital,
University of California San Diego, San Diego, CA 92093-0602, USA.
Email: [email protected]
The Association Between Common
Bile Duct Diameter and the Severity
of Coronary Artery Atherosclerosis,
Based on Calcium Score
Fatemeh Kheiridoost Langroudi, MD
1
,
Taraneh Faghihi Langroudi, MD
1
, Neda Akhoundi, MD
2
,
and Alireza Siami, MSc
3
Abstract
Objective: The aim was to assess the relationship between the coronary calcium score and the common bile duct
(CBD) diameter, to determine whether the increase in CBD diameter in patients without hepatobiliary disease could
represent cardiovascular disease, or the extent of atherosclerosis in coronary arteries.
Materials and Methods: The study cohort consisted of 103 patients referred for computed tomographic angiography
(CTA) for coronary artery assessment. None of the patients had a gallbladder, biliary, or pancreatic disease or surgery
history. The Agatston score determined the rates of arterial calcification. The diameter of the CBD was measured
for a sonogram.
Results: There was a statistically significant relatively strong correlation between calcium score and CBD diameter
(r = 0.44, P = .001), independent of baseline variables, such as demographics and cardiovascular risk profiles. In the
multivariable regression model, advanced age (beta = 0.825, P = .005), history of hypertension (beta = 0.591, P =
.034), and history of coronary stenting (beta = 1.339, P = .001) were shown to be the main determinants of CBD
dilatation.
Conclusion: A statistically significant correlation existed between the CBD diameter and calcium score, within the
coronary arteries and this could represent a shared pathophysiology between CBD dilatation and the severity of
coronary atherosclerosis.
Keywords
common bile duct diameter, extrahepatic bile duct, Agatston score, calcification

562 Journal of Diagnostic Medical Sonography 39(6)
sample of 604 asymptomatic subjects, the largest diame-
ter reported ranged from 1.8 to 11.8 mm.
1
The diameter of
the CBD can change in response to various factors,
including age, cholecystectomy, sphincterotomy, certain
drugs, such as methadone, measurement location, respi-
ration, and body mass index (BMI).
3–9
Among these fac-
tors, age has been a focus of many studies. Although the
results of these studies have been controversial, and a
strong correlation between age and CBD diameter has not
been established, some considerations have been sug-
gested for evaluating the normal CBD width with aging.
For example, adding 0.2–1.0 mm to the normal upper
limit of the CBD diameter, for each increased decade of
age, starting at age 40 or 60.
10
Since the increased diam-
eter of the CBD in the elderly is associated with reduced
blood flow to the CBD, it could be inferred that the CBD
diameter changes may indicate atherosclerosis in arteries.
In this regard, the relationship between the calcium aortic
score and CBD diameter was investigated, and a moder-
ate relationship between these two parameters was
reported.
10
This study was the first to determine the rela-
tionship between CBD diameter and coronary artery cal-
cium score using a 64-slice abdominal CT examination.
If a significant relationship is observed between these
two variables, it could be concluded that changes in CBD
diameter may not only represent cardiovascular disease
but also indicate the extent of atherosclerosis in the coro-
nary arteries. Furthermore, considering the non-invasive
nature of sonography, in measuring CBD diameter, this
could be used as a primary diagnostic test for estimating
the severity of coronary artery atherosclerosis, based on
patients’ calcium score without known biliary disease.
Materials and Methods
Study Setting and Participants
The current study was completed with a prospective cohort
and conducted at a teaching hospital in Tehran, Iran, between
May 2018 and September 2019. The study received approval
from the hospital’s local ethics committee (IRB# IR.SBMU.
REC.9716). The study’s objectives were explained to the
patients, and written informed consent was obtained from all
participants. The study recruitment included individuals
with coronary artery disease (CAD) and referred for coro-
nary artery computed tomographic angiography (CTA). The
exclusion criteria included a history of liver, gallbladder,
biliary, or pancreatic disease or surgery, such as patients with
cholelithiasis or any gallbladder or pancreatic abnormality.
Before the examination, serum bilirubin levels, alkaline
phosphatase, and liver transaminases were measured and
reported as within normal reference ranges for all patients.
Patients taking medications that caused smooth muscle
relaxation (e.g., calcium blockers and papaverine hydro-
chloride) and patients with a BMI of more than 25 kg/m
2
were also excluded from the study. In addition, patients with
a history of coronary artery stent implantation or coronary
artery bypass grafting (CABG) were evaluated separately
based on their history of atherosclerosis.
Coronary Artery CTA
CTA was performed with a 64-slice device (Siemens Co.,
Germany), at least 6 hours after the patient’s last meal, and
two board-certified radiologists examined the images
obtained in all patients. Each patients’ heart rates were
evaluated, and a rate of 65 beats per minute was consid-
ered appropriate for starting imaging. If necessary, Metoral
tablets were used to lower those patients with an elevated
heart rate. The patient’s coronary CTA images were
assessed to find any stenosis or plaques (See Figure 1).
The rates of calcification of plaques were given a number
called an Agatston score. Based on the total calcium score,
grading of coronary artery disease was done as below:
No evidence of CAD: 0 calcium score
Minimal: 1–10 calcium score
Mild: 11–100 calcium score
Moderate: 101–400 calcium score
Severe: > 400 calcium score
Sonography of the CBD
Sonography was performed on patients after a fasting
period of 6–12 hours by a diagnostic radiologist with 15
years of experience, in conducting sonography. The radi-
ologist was blinded to each patient’s Agatston score. A
Samsung WS80A ultrasound equipment system (Samsung
Figure 1. An axial image from the cardiac computed
tomogram that shows calcified plaques in the left circumflex
and left anterior descending artery (indicated with white
arrows).

Kheiridoost Langroudi et al 563
Healthcare.com) equipped with a curvilinear transducer
(2.5–3.5 MHz) was used for the examination. Patients
were examined supine or in the left lateral oblique posi-
tion and during a deep inspiration, using a right subcostal
approach. The CBD was measured below the cystic duct
and closely associated with the right hepatic artery.
Electronic calipers were used to measure the CBD diam-
eter from the outer to inner edges of the duct (See Figure
2). Three measurements were taken, and the average was
considered the CBD’s final diameter. A cut-off value of
7.0 mm was considered for CBD dilatation in this study.
In addition to the CBD sonographic findings and the
calcium score of each patient, demographic characteris-
tics and clinical signs of patients were also recorded.
Statistical Analysis
Descriptive data were reported as a mean and ± standard
deviation (SD) for continuous variables. Numeric data
(percentage) were provided for categorical variables. The
Kolmogorov-Smirnov test was used to determine a nor-
mal distribution of continuous variables. The means of
continuous variables with normal distribution were com-
pared using an independent group t-test. Proportions for
categorical variables were compared using the chi-square
test. Pearson’s or Spearman’s correlation test, which
determines the association between quantitative vari-
ables. The multivariable linear regression model was
employed to determine the main factors correlating with
increased CBD diameter. All statistical analyses were
performed using SPSS version 22.0 software (IBM,
Armonk, New York), and a P-level of < .05 was deter-
mined a priori, as statistically significant.
Results
In this study, a total of 103 patients who were referred
for CTA and met inclusion criteria were enrolled, how-
ever, 21 patients had no evidence of CAD, 24 had mini-
mal CAD, and 22, and 23 had mild and moderate CAD
based on their Agatston score, respectively. Thirteen
patients had severe CAD (Agatston score > 400). The
mean age of participants was 53.79 ± 10.79 years and
ranged from 31 to 76 years. In this cohort, 28% were
male. Overall, 17.4% had diabetes, 40% were hyperten-
sive, 12% were current smokers, and 30% had hyperlip-
idemia (See Table 1).
The mean calcium score in men was 49.82 ± 11.74,
and in women was 47.32 ± 23.50, with no significant
difference (P = .920).
The mean CBD diameter according to the baseline
variables is summarized in Table 2. In this regard, the
mean CBD diameter was independent of gender, smok-
ing, or history of diabetes. In contrast, a higher mean
CBD diameter was found more in older patients than
younger patients, as well as those with hyperlipidemia
compared with cases without hyperlipidemia. Likewise,
a higher mean CBD diameter was found in patients with
hypertension compared with patients without, and in
patients with a history of coronary stenting than in those
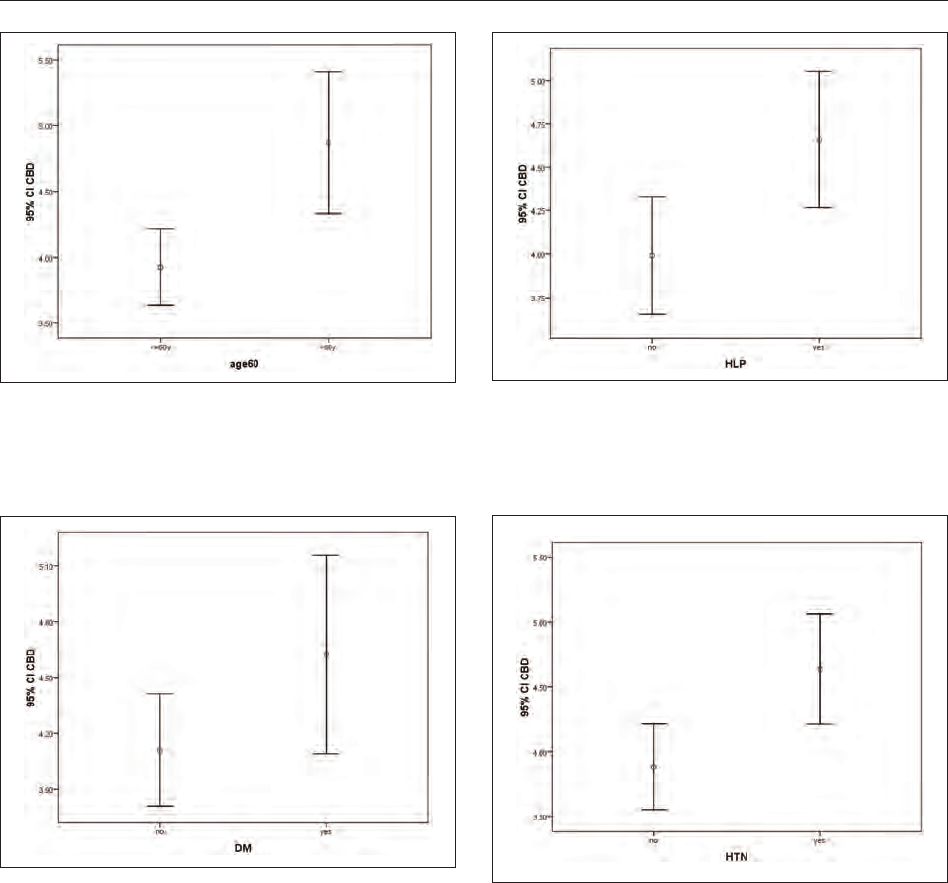
without this intervention (See Figures 3–8). In the mul-
tivariable regression model, advanced age (beta =
0.825, P = .005), history of hypertension (beta = 0.591,
P = .034), and history of coronary stenting (beta =
1.339, P = .001) were shown to be the main determi-
nants of CBD dilatation (See Table 3). A statistically
significant relatively strong positive correlation was
observed between calcium score and CBD diameter (r
= 0.444, P = .001). In addition, a similar association
was found between age and the Agatston score (r =
0.543, P = .014) (See Table 4).
Discussion
The role of CT and sonography in assessing various dis-
eases is well known.
11–19
This cohort study investigated
the potential association between coronary artery athero-
sclerosis, based on CT, and the diameter of the CBD,
which was measured during sonography. Therefore, the
Agatston calcium score method was utilized to assess the
level of coronary artery atherosclerosis. The findings
obtained in this study revealed a positive correlation
between CBD diameter and coronary Agatston calcium
score.
As discussed earlier, several factors can influence
CBD diameter, and radiologists need to consider these
factors when determining whether an observed increase
in diameter is pathological. This cohort of patients
Figure 2. A sonogram of the liver, which demonstrates the
method of measuring the diameter of the common bile duct.
The electronic calipers are used to measure the diameter
of the common bile duct and placed on the outer and inner
edges of the duct.

564 Journal of Diagnostic Medical Sonography 39(6)
demonstrated that in addition to factors, such as old age,
history of cholecystectomy, drug use, and high BMI, ath-
erosclerosis was also a variable that affected the size of
their CBD. Previous research has shown that connective
tissue fibers replace normal smooth myocytes as individ-
uals’ age, and tissue metabolism undergoes changes,
likely associated with decreased blood supply.
20
These
findings and evidence of hypoxia and smooth muscle
relaxation
21
suggest the need for further studies to deter-
mine the extent to which chronic hypoxia can impact the
diameter of the CBD.
Several recent studies have highlighted the susceptibility
of pathological changes in biliary dilatation following athero-
sclerotic changes in the bile ducts, particularly the CBD.
Moharramzad et al, found a close correlation between the
atherosclerotic score, based on the Agatston score, and the
diameter of the CBD.
9
This may suggest that the occurrence
of atherosclerosis, especially with age, leads to changes in the
vascular supply to the biliary system, particularly the bile
ducts. This diminished vascular supply may cause significant
changes in the muscles of these ducts and ultimately result in
changes to CBD diameter. However, histological evaluations
and pathological studies are required to prove such hypothe-
ses, and further research in this area is recommended.
Moreover, studies have suggested an association between
acute cholecystitis and choledocholithiasis with ischemic
heart disease. Salameh et al reported that one-fifth of patients
with angina pectoris that needed coronary angioplasty and
stenting also required CBD exploration.
21
That study would
support the findings of the current study regarding the asso-
ciation between a history of coronary stenting and CBD
diameter. In addition, Zheng et al found that patients with a
history of gallbladder disease had a 1.15-fold increased risk
of coronary heart disease compared with individuals without
gallbladder disease.
22
They observed increased intima-media
Table 2. The Mean Diameter of the Common Bile Duct
Based on the Baseline Variables.
Parameter Mean CBD P-value
Gender .444
Male 4.28 ± 1.41
Female 4.07 ± 1.28
Age group .001
≤ 60 years 3.92 ± 1.24
> 60 years 4.87 ± 1.41
Diabetes mellitus .155
Positive 4.62 ± 1.03
Negative 4.11 ± 1.40
Hyperlipidemia .022
Positive 4.65 ± 1.07
Negative 3.99 ± 1.42
Hypertension .005
Positive 4.63 ± 1.36
Negative 3.88 ± 1.27
Smoking .326
Positive 4.54 ± 1.77
Negative 4.14 ± 1.28
Coronary stenting .016
Positive 5.07 ± 1.01
Negative 4.08 ± 1.35
Figure 3. A box plot that compares the mean diameter of
common bile duct in men and women.
Table 1. The Study Patient’s Clinical Characteristics Based on Their Calcium Score.
No evidence of CAD:
0 calcium score
N = 21
Minimal: 1–10
calcium score
N = 24
Mild: 11–100
calcium score
N = 22
Moderate: 101–400
calcium score
N = 23
Severe: > 400
calcium score
N = 13
Total
N = 103
Gender (male) 2 8 14 3 2 29 (28%)
Age > 60 years 6 2 5 10 6 29 (28%)
Diabetes mellitus 0 4 8 4 2 18 (17.4%)
Hyperlipidemia 1 4 6 11 9 31 (30%)
Hypertension 2 8 18 4 10 42 (40%)
Smoking 1 2 8 1 1 13 (12%)
Coronary stenting 0 0 0 2 11 13 (12%)
Kheiridoost Langroudi et al 565
thickness, plaque formation, and calcification in the aorta and
iliac arteries, suggesting a link between biliary disease and
atherosclerosis.
23
The current study has revealed significant
findings regarding the association between CBD diameter
and cardiovascular risk factors, such as old age, hyperten-
sion, and previous history of coronary intervention. The
observed relationship between increased CBD diameter and
aging is consistent with findings from other published stud-
ies,
4,24,25
indicating that aging may lead to decreased flexibil-
ity and inflammation in the bile ducts. Similarly, the
association between hypertension and CBD diameter may
be related to biliary dysfunction and underlying hyperten-
sion, although further evaluation is needed to understand the
pathophysiology of this relationship.
Limitations
These results are limited by the non-randomized research
design with threats to internal and external validity. In
addition, the study was conducted at a single center with
a convenient sample of patients. The limited the sample
size and inability to utilize the full capacity of all univer-
sity hospitals, in the area, is an additional limitation. In
addition, extensive exclusion criteria were implemented
to control various factors affecting atherosclerosis and
CBD diameter, which further reduced the sample size.
Including patients with clinical atherosclerosis, such as
those with myocardial infarction, stroke, or peripheral
Figure 4. A box plot that compares the mean diameter of
the common bile duct in patients younger than 60 and those
older than 60.
Figure 5. A box plot that compares the mean diameter of
the common bile duct in diabetic and non-diabetic patients.
Figure 6. A box plot that compares the mean diameter
of the common bile duct in patients with and without
hyperlipidemia.
Figure 7. A box plot that compares the mean diameter
of the common bile duct in patients with and without
hypertension.

566 Journal of Diagnostic Medical Sonography 39(6)
arterial disease, could have increased the number of study
patients. However, ethical considerations and radiation
risks associated with abdominal CT for these patients
prevented their inclusion in the study. It is recommended
that future studies focus on investigating the association
between CBD diameter and the use of the atherosclerotic
cardiovascular disease (ASCVD) score to further enhance
our understanding of this possible association.
Conclusion
The findings of this study revealed a statistically signifi-
cant relatively strong correlation between CBD diameter
and the calcium score, within coronary arteries, which
may suggest a potentially shared pathophysiology
between CBD dilatation and the severity of coronary ath-
erosclerosis. It is important to note that this study had
inherent limitations, therefore, the results must be inter-
preted with caution, regarding the broader population.
Further studies with larger and more diverse cohorts are
needed to confirm these findings and establish a specific
diagnostic cut-off point for CBD diameter. Such a diag-
nostic cut-off point would be valuable in clinical practice,
as measurements exceeding this threshold in patients
without the known biliary disease could indicate higher
calcium scores in the coronary arteries. This could poten-
tially warrant further evaluation of these at risk patients
using more invasive imaging techniques, such as coro-
nary CTA or routine diagnostic angiography.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with
respect to the research, authorship, and/or publication of this
article.
Funding
The authors received no financial support for the research,
authorship, and/or publication of this article.
Ethics Approval
The study received approval from the hospital’s local ethics
committee (IRB# IR.SBMU.REC.9716).
Informed Consent
Informed consent was not sought for the present study because
all case data was de-identified and/or aggregated and followed
ethics committee or IRB guidelines (also referred to as the
Honest Broker System).
Animal Welfare
Guidelines for humane animal treatment did not apply to the
present study because no animals were used for the purpose of
this study.
Trial Registration
Not applicable.
ORCID iD
Neda Akhoundi https://orcid.org/0000-0002-5886-5897
Figure 8. A box plot that compares the mean diameter of
the common bile duct in patients with and without coronary
stenting.
Table 3. The Study Parameters That Were Tested for
Association With Dilatation of the Common Bile Duct.
Study parameters Beta
Standard
error
P-value
(P ≤ .05)
Gender –0.219 0.274 .427
Age 0.825 0.290 .005
Diabetes mellitus –0.378 0.415 .364
Hyperlipidemia 0.452 0.301 .137
Hypertension 0.591 0.275 .034
Smoking 0.438 0.389 .263
Coronary stenting 1.339 0.389 .001
Table 4. The Strength of Association Between Age,
Common Bile Duct (CBD) Diameter, and Agatston Score, for
This Study Cohort.
Study parameters
R
coefficient
P-value
(P ≤ .05)
Age and CBD diameter
a
0.493 .001
CBD diameter and Agatston score
b
0.444 .002
Age and Agatston score
b
0.543 .014
a
Pearson’s correlation test.
b
Spearman’s rank correlation test.

Kheiridoost Langroudi et al 567
References
1. Senturk S, Miroglu TC, Bilici A, et al: Diameters of the com-
mon bile duct in adults and postcholecystectomy patients: a
study with 64-slice CT. Eur J Radiol. 2012;81(1):39–42.
2. Kratzer W, Wahl S, Vonend C, et al: Caliber of the common
bile duct: effect of cholecystectomy and other factors in a
ultrasonographic study of 8534 patients. Z Gastroenterol.
2015;53(10):1161–1166.
3. Itoi T, Kamisawa T, Fujii H, et al: Extrahepatic bile
duct measurement by using transabdominal ultrasound
in Japanese adults: multi-center prospective study. J
Gastroenterol. 2013;48(9):1045–1050.
4. Bachar GN, Cohen M, Belenky A, Atar E, Gideon S: Effect
of aging on the adult extrahepatic bile duct: a sonographic
study. J Ultrasound Med. 2003;22(9):879–882.
5. Bucceri AM, Brogna A, Ferrara R: Common bile duct cali-
ber following cholecystectomy: a two-year sonographic
survey. Abdom Imaging. 1994;19(3):251–252.
6. Karincaoglu M, Yildirim B, Seckin Y, Kantarceken B,
Aladag M, Hilmioglu F: Common bile duct diameters after
endoscopic sphincterotomy in patients with common bile
duct stones: ultrasonographic evaluation. Abdom. Radiol.
2003;28(4):531–535.
7. Bates DDB, Tamayo-Murillo D, Kussman S, et al: Biliary
and pancreatic ductal dilation in patients on methadone
maintenance therapy. Abdom Radiol. 2017;42(3):884–889.
8. Peng R, Zhang L, Zhang X-M, et al: Common bile duct
diameter in an asymptomatic population: a magnetic reso-
nance imaging study. World J Radiol. 2015;7(12):501–508.
9. Moharamzad Y, Abbasi S, Sanei Taheri M, Faghihi
Langroudi T: Association between common bile duct diam-
eter and abdominal aorta calcium score. Abdom Radiol
(NY). 2018;43(8):2097–2102.
10. Paraham M, Moghadam AM, Akhoundi N, Haghi S:
An investigation of the relationship between Vitamin D
deficiency and carotid intima-media thickness (IMT) in
patients with Type 1 diabetes. J Pharmaceut Negat Res.
2022;13:8033-8039.
11. Akhoundi N, Langroudi TF, Rajebi H, et al: Computed
tomography pulmonary angiography for acute pulmonary
embolism: prediction of adverse outcomes and 90-day
mortality in a single test. Pol J Radiol. 2019;84:e436–e446.
12. Akhoundi N, Faghihi Langroudi T, Rezazadeh E, et al:
Role of clinical and echocardiographic findings in
patients with acute pulmonary embolism: prediction of
adverse outcomes and mortality in 180 days. Tanaffos.
2021;20(2):99–108.
13. Akhoundi N, Bozchelouei JK, Abrishami A, et al:
Comparison of MRI and endoanal ultrasound in assess-
ing intersphincteric, transsphincteric, and suprasphincteric
perianal fistula [published online ahead of print April 11,
2023]. J Ultrasound Med. doi:10.1002/jum.16225
14. Akhoundi N, Rezazadeh E, Siami A, Komijani Bozchelouei
J, Ramezani M, Nosrati M: The comparison of pulsatil-
ity index, resistance index, and diameter of the tempo-
ral, carotid, and vertebral arteries during active migraine
headaches to non-headache intervals [published online
ahead of print May 10, 2023]. J Diagn Med Sonograp.
doi:10.1177/87564793231165512
15. Haghi S, Kahkouee S, Kiani A, et al: The diagnostic accu-
racy of endobronchial ultrasound and spiral chest com-
puted tomography scan in the prediction of infiltrating and
non-infiltrating lymph nodes in patients undergoing endo-
bronchial ultrasound. Pol J Radiol. 2019;84:e565–e569.
16. Nosrati M, Akhoundi N, Ahmadzadeh Nanva AH, et al: The
role of lung ultrasonography scoring in predicting the need
for surfactant therapy in neonates, with respiratory distress
syndrome [published online ahead of print May 2, 2023]. J
Diagn Med Sonograp. doi:10.1177/87564793231167856
17. Akhoundi N, Faghihi Langroud T, Shafizadeh K,
Jabbarzadeh MJ, Talebi S: Incidental abdominal aortic
aneurysm in the psoriasis patient: a case report and review
of literature. Galen Med J. 2018;7:e1168.
18. Akhoundi N, Sedghian S, Siami A, et al: Does adding the
pulmonary infarction and right ventricle to left ventricle
diameter ratio to the Qanadli Index (A Combined Qanadli
Index) more accurately, predict short-term mortality in
patients with pulmonary embolism? [published online
ahead of print June 16, 2023]. Indian J Radiol Imaging.
doi:10.1055/s-0043-1769590
19. Kialian GP, Aznaurian AV: The age-related characteris-
tics of the muscular layer of the common bile duct in man.
Morfologiia. 1995;108(1):10–12.
20. Veith C, Schermuly RT, Brandes RP, Weissmann NM:
Molecular mechanisms of hypoxia-inducible factor-
induced pulmonary arterial smooth muscle cell alterations
in pulmonary hypertension. J Physiol. 2016;594(5):1167–
1177.
21. Salameh JR, Franklin ME Jr: Acute cholecystitis and
severe ischemic cardiac disease: is laparoscopy indicated?
JSLS. 2004;8(1):61–64.
22. Zheng Y, Xu M, Li Y, et al: Gallstones and risk of coronary
heart disease: prospective analysis of 270 000 men and
women from 3 US cohorts and meta-analysis. Arterioscler
Thromb Vasc Biol. 2016;36(9):1997–2003.
23. Matcuk GR Jr, Grant EG, Ralls PW: Ultrasound measure-
ments of the bile ducts and gallbladder: normal ranges and
effects of age, sex, cholecystectomy, and pathologic states.
Ultrasound Q. 2014;30(1):41–48.
24. Daradkeh S, Tarawneh E, Al-Hadidy A: Factors affect-
ing common bile duct diameter. Hepatogastroenterology.
2005;52(66):1659–1661.
25. Horrow MM: Ultrasound of the extrahepatic bile duct:
issues of size. Ultrasound Q. 2010;26(2):67–74.

SDMS CME Credit – The Association Between
Common Bile Duct Diameter and the Severity of
Coronary Artery Atherosclerosis, Based on Calcium
Score
SDMS members can earn SDMS CME credit by successfully completing the complimentary online
CME test in the SDMS Learning Center at learn.sdms.org. Non-members may access the online CME
test for a fee. Note: questions may appear in random order online.
1. Traditionally, the upper limits of normal for a common
bile duct diameter in a patient that is post cholecystec-
tomy is _______.
A. 6.0 mm
B. 11.8 mm
C. 10.0 mm
D. 1.8 mm
2. Which of the following is not a factor that can change
common bile duct diameter?
A. Sphincterotomy
B. Splenectomy
C. Body Mass Index
D. Respiration
3. According to this study, which individual factor has a
larger common bile duct diameter?
A. Prior coronary stenting
B. Age less than 60 years old
C. Woman
D. Hypotension
4. The findings of this study showed a relationship
between ____________.
A. Common bile duct dilatation and coronary athero-
sclerosis
B. Biliary atresia and common bile duct dilatation
C. Hypertension and coronary atherosclerosis
D. Common bile duct dilatation and hypotension
5. Which modality was used to measure total calcium
score?
A. US
B. CTA
C. MRA
D. NM
1201586JDM
XXX10.1177/87564793231201586Journal of Diagnostic Medical SonographyMeeting-Report
meeting-report2023
Authors: Fatemeh Kheiridoost Langroudi, MD, Taraneh Faghihi Langroudi, MD, Neda Akhoundi, MD, and Alireza Siami, MSc
Category: Abdomen [AB]
Credit: 0.75 SDMS CME Credit
Objectives: After studying the article, you should be able to:
Discuss the difference in common bile duct diameter measurements.
Explain the relationship between common bile duct diameter and coronary artery atherosclerosis.
Describe the different modalities used to measure bile duct diameter and calcium scoring.

https://doi.org/10.1177/87564793231192831
Journal of Diagnostic Medical Sonography
2023, Vol. 39(6) 569 –574
© The Author(s) 2023
Article reuse guidelines:
sagepub.com/journals-permissions
DOI: 10.1177/87564793231192831
journals.sagepub.com/home/jdm
Original Research
In this recent decade, the mortality rate caused by cardio-
vascular diseases has increased drastically in Middle
Eastern countries compared with other parts of the world.
Studies have also revealed that the mortality caused by
cardiovascular disorders in the Middle East increased by
171% from 1990 to 2020. The epidemiological studies in
Iran and the United Arab Emirates reflect an estimated
prevalence of 5.9% for cardiovascular diseases in the
future.
1
In response to this rise in cardiovascular disease,
goal-directed, emergency medicine departments (EDs)
have used a point-of-care ultrasound (POCUS) curricu-
lum to try to increase a physician trainee’s self-confi-
dence and performance.
2
1192831JDM
XXX10.1177/87564793231192831Journal of Diagnostic Medical SonographyMohammadi et al
research-article2023
1
Emergency Medicine Management Research Center, Health
Management Research Institute, Iran University of Medical Sciences,
Tehran, Iran
2
Student Research Committee, School of Medicine, Iran University of
Medical Sciences, Tehran, Iran
3
Trauma and Injury Research Center, Iran University of Medical
Sciences, Tehran, Iran
Received February 11, 2023, and accepted for publication July 17, 2023.
Corresponding Author:
Samira Vaziri, Emergency Medicine Management Research Center,
Health Management Research Institute, Iran University of Medical
Sciences, Tehran 1449614535, Iran.
Email: [email protected]
Determining the Extent of Agreement
for Determining the Echographic
Ejection Fraction Determined by
Emergency Medicine Residents
Compared with a Cardiologist
Fatemeh Mohammadi, MD
1
, Seyedamir Tabibzadeh Dezfooli, MD
1
,
Babak Sadeghzadeh, PhD
2
, Mojtaba Chardoli, PhD
1
, Hamed Basir Ghafouri, PhD
3
,
Mahdi Rezai, PhD
1
, Reza Mosaddegh, PhD
1
, and Samira Vaziri, PhD
1
Abstract
Objective: The aim of this study was to determine the extent of agreement on the measured echographic ejection
fraction measured by emergency medicine (EM) residents compared with a cardiologist.
Materials and Methods: This study was conducted with cardiac patients admitted to a hospital emergency
department in Tehran, Iran. A total of 156 patient cases were reviewed. A group of trained EM residents evaluated
the ejection fraction (EF) of these patients utilizing three different methods: Simpson’s method (N = 50), E-Point
Septal Separation (EPSS, N = 56), and a visual technique (N = 50). A final assessment was made for all patients by a
cardiologist.
Results: In 69.3% of these patient cases, there was a significant correlation between the EM residents’ report and
the cardiologists, with Cohen’s Kappa coefficient of .746 (P < .001). The Kappa coefficient for the visual technique,
Simpson’s method, and EPSS was .697, .467, and .487, respectively. The sensitivity, specificity, positive and negative
predictive values of EF measurements, provided by the EM residents, were 0.89%, 64.2%, 81.6%, and 76.5% compared
with the cardiologist, respectively.
Conclusion: This description study was done to determine the agreement of echocardiographic measurement of
EF, assessed by trained EM residents, compared with a cardiologist’s review. In this case, the results demonstrated
moderate to good agreement.
Keywords
inter-rater reliability, ventricular ejection fraction reporting, echocardiography, emergency medicine cardiac evaluation

570 Journal of Diagnostic Medical Sonography 39(6)
As the most important indicator of cardiac function,
obtaining the cardiac ejection fraction (EF) is vital in
deciding on an at-risk patient’s clinical management,
daily clinical examinations, and ultimate prognosis.
3
The
cardiac EF serves as reliable evidence of total heart func-
tion, and changes in EF can indicate various congenital
and acquired heart disorders.
4
The advantages of obtain-
ing this measurement include easy implementation,
safety, the minimal need for preparing the patient, repeat-
ability, noninvasiveness, and cost-effectiveness. Hence,
physicians highly use echocardiography a noninvasive
diagnostic tool to measure EF.
5
A heart attack or other cardiac disease can negatively
influence the EF.
6
The accurate assessment of left ven-
tricular ejection fraction (LVEF) is essential for manag-
ing patients with acute diseases, such as those with chest
pain, cardiogenic shock, or severe respiratory distress.
7
Physicians who are not cardiologists can learn to conduct
a basic echocardiogram and assess cardiac EF.
8
An echo-
cardiogram allows emergency medicine (EM) physicians
to obtain diagnostic information on many acute cardio-
vascular diseases, such as tamponade, pulmonary embo-
lism (PE), cardiogenic shock, and cardiogenic pulmonary
edema.
9
Currently, the rapid ultrasound for shock and
hypotension (RUSH) examination can be conducted in
the ED, at the bedside of critically ill patients, to deter-
mine the cause of cardiogenic shock. This exam includes
an assessment of EF, while can assess cardiac function
and the probability of PE, tamponade, and pericardial
effusion.
8,10
However, only a few studies have been con-
ducted to validate the accuracy of EF calculations in the
ED. Therefore, this study was composed to determine the
reliability and potential accuracy of these measurements,
made in the ED. To this end, a reliability and accuracy
test was conducted, of the echographic EF measurements,
made by EM residents compared with a cardiologist.
Materials and Methods
Study Design
This study was designed to determine concordance
between diagnostic test results and a gold standard. The
study design was presented to the Ethics Committee of
Iran University of Medical Sciences and was approved
(ethics code: IR.IUMS.FMD.REC.1398.070). After pro-
viding a complete explanation of the study, informed
written consent was obtained from all patients. It was
important stress to the patients that participation in the
study was optional and medical services would still be
provided regardless of their willingness to participate in
the study. There were no additional expenses charged to
the patient for additional interpretations. The researchers
abided by the Helsinki Convention principles during this
study. Each patient provided verbal consent and was
assured of medical confidentiality.
Study Cohort and Sample Size
This study was conducted, in 2020, with qualified patients
between the ages of 18 and 80 years of age and presenting
with dyspnea, to the ED at Rasoul Akram Hospital.
Exclusion criteria included those patients who were intu-
bated, pregnant, elevated cardiac biomarkers, hemody-
namically unstable, and patients with atrial fibrillation.
These exclusions were made due to the possible influence
on echocardiographic EF measurements.
In this study, sample measurements were gathered
using a convenient sampling technique. A total of 156
participants were enrolled in the study.
Measurement Technique
In this study, five senior EM residents received theoretic
content (4 hours) and practical training (5 hours on 15
patients) from a skilled and experienced echocardiologist.
Following the referral of patients, eligible individuals
underwent an echocardiogram that was conducted on a
Samsung HM70A ultrasound equipment system
(Samsung Healthcare.com). Each EM resident measured
the LVEF using one of the following three diagnostic
methods: Simpson’s method, E-Point Septal Separation
(EPSS), and a visual assessment. Simpson’s method
requires tracking the endocardium in apical four-chamber
and two-chamber views, during end-systole and end-
diastole. The left ventricle’s end-diastolic volume (EDV)
and the end-systolic volume (ESV) were calculated.
Afterward, the left ventricular EF is calculated via the
following formula
EF
VolVol
Vol
ed es
ed
=
−
×100
Normal function is defined as an EF of more than
55%. Mild dysfunction is an EF between 45% and 54%.
Moderate and severe dysfunctions are considered 30%–
44% and less than 30%, respectively.
The EPSS is an M-mode method measured in the para-
sternal long-axis (PLAX) view. The shortest distance
between the apex of the anterior leaflet of the mitral valve
and the ventricular septum is measured in millimeters,
called EPSS. A distance less than 8.0 mm is defined as a
normal function (EF >55%), between 8 and 14 is mild
dysfunction (EF = 45%–54%), between 14 and 17 is
moderate dysfunction (EF = 30%–44%), and more than
17 is considered as severe dysfunction (EF <30%).
Using a visual method (sometimes referred to as “eye-
balling”), the EF was estimated based on personally
detecting LV contraction in the PLAX view.

Mohammadi et al 571
Each resident looked for an inward movement of the
endocardium, thickening of the myocardium, the motion
of the anterior mitral valve leaflet, and geometry of the
left ventricle (e.g., size and aneurysms). This method
classified dysfunction in comparison with Simpson’s and
EPSS method of measurement.
Finally, a cardiologist assessed all the patients using the
same offline approach and device to assess the LVEF. The
cardiologist’s report was considered the diagnostic gold
standard for interpretation. It is also worth noting that the
cardiologist was unaware of the results reported by the EM
residents. Also, one cardiologist conducted all the echocar-
diographic readings. There was a maximum interval of 1
hour between two echocardiography examinations con-
ducted by the EM resident and the cardiologist. As men-
tioned, all patients were in stable condition, and two
echocardiograms did not hinder or postpone the diagnostic
or therapeutic measures. All the cardiac function informa-
tion was recorded as well as their age, gender, blood pres-
sure, heart rate, respiratory rate, and body mass index (BMI).
These data were all collected on a predesigned checklist.
Finally, all data points were analyzed statistically.
Data Analysis
The analysis was conducted using SPSS statistical soft-
ware (IBM Corp., Armonk, NY, USA). The quantitative
data were descriptively defined by the mean and standard
deviations. The qualitative data were described using per-
centages and frequency. Cohen’s Kappa coefficient,
Mann-Whitney U test, and Spearman’s correlation tests
were performed on this data set. The diagnostic sensitiv-
ity, specificity, positive and negative predictive values of
the resident’s measured EF were preformed (See Table
1). As previously mentioned, the reported measurements
made by the cardiologist were considered the diagnostic
gold standard. The statistical significance was set a priori
at P < .05.
Results
The aim of this study was to determine the extent of
agreement on the measured echographic EF measured by
EM residents compared with a cardiologist. The study
participants included 156 patients. According to the car-
diologist’s report, 57 patients had normal cardiac func-
tion based on their EF measurement. Demographic
characteristics are provided in Table 2. The mean blood
pressure, respiratory rate, and heart rate values are also
provided (See Table 3).
As shown in Table 4, the comparison between the EF
measurements made by the EM residents and the cardi-
ologist was analyzed qualitatively and quantitatively.
In the qualitative section, the agreement between the
EM resident and the cardiologist reports was at 69.3% for
all the cases. A moderately strong Cohen’s Kappa coeffi-
cient of .746 (P < .001) was statistically significant. The
results of the quantitative analysis were also compared
with moderately strong comparison between the EM resi-
dents’ reports and the cardiologist’s reports (P < .001).
The Kappa contingency coefficient and Spearman’s
coefficient for each diagnostic method are shown
Table 1. Evaluation of Sensitivity, Specificity, Positive Predictive Value, and Negative Predictive Value of the Measured Ejection
Fraction by Emergency Medicine Residents.
Groups Sensitivity Specificity Positive Predictive Value Negative Predictive Value
Visual technique 94.8% 72.7% 92.5% 80.0%
E-Point Septal Separation 85.1% 65.5% 69.6% 82.6%
Simpson’s method 85.2% 56.2% 80.5% 64.2%
Total 89.0% 64.2% 81.6% 76.5%
Table 2. The Study Cohort’s Demographic Characteristics.
N
% of the
Total Sample
Sample size 156 100
Male 69 44.2
Female 87 55.8
Minimum Maximum M SD
Age 18 80 65.14 14.70
Body mass
index
17 31 24.74 6.96
Abbreviations: M, mean; SD: standard deviation.
Table 3. The Mean Blood Pressure, Heart Rate, and
Respiratory Rate for the Study Cohort.
Variables M ± SD Minimum Maximum
Systolic blood
pressure in mmHg
128.49 ± 23.49 80 190
Diastolic blood
pressure in mmHg
75.51 ± 9.10 60 110
Heart rate 80.50 ± 12.83 45 110
Respiratory rate 17.39 ± 1.78 12 25
Abbreviations: M, mean; SD: standard deviation.

572 Journal of Diagnostic Medical Sonography 39(6)
separately in Table 5. In this cohort of patients, there were
significant Cohen’s Kappa coefficient and high correla-
tion between the EM residents and the cardiologist based
on all the diagnostic techniques to measure EF.
Based on these reported findings, the highest agree-
ment and correlation between the EM residents and the
cardiologist’s measurements, as well as the highest speci-
ficity, sensitivity, and positive and negative predictive
values, were reported when using the person visualiza-
tion technique. In addition, investigating the agreements
between EM residents and cardiologists indicated that for
all five trained EM residents, the agreements were sig-
nificant and very similar (81.3%, 80.6%, 83.8%, 77.4%,
and 77.4%, respectively).
Discussion
Based on the findings of this study, the overall agreement
between the EM residents and the cardiologists was
69.3%, which was significant. Besides, the sensitivity,
specificity, and positive and negative predictive values of
the EF measurements by the EM resident were 89.0%,
64.2%, 81.6%, and 76.5%, respectively, compared with
the cardiologist’s report, which was considered the gold
standard.
In an investigation, Unlüer et al. studied the visual
(eyeballing) technique for assessing echocardiographic
EF. In that study, the sensitivity, specificity, and positive
and negative predictive values of the patient’s bedside EF
measurements, made by an EM specialist compared with
a cardiologist, were 98.7%, 86.2%, 90.4%, and 90.4%,
respectively. In the Unlüer et al., study, the reported val-
ues were also higher than the total values in this study.
However, Unlüer et al.
11
only used the visual technique
for assessment and used EM physicians to provide the
reporting. The sensitivity, specificity, and positive and
negative predictive values resulting from the visual tech-
nique in this study were 94.8%, 72.7%, 92.5%, and
80.0%, respectively. These values are almost similar to
the values reported by Unlüer et al.
11
Similar to the study
by Unlüer et al., the lowest value reported in this study
was the specificity of the bedside EF calculation. In both
studies, the highest level of disagreement was in patients
with a normal left ventricular EF diagnosed with dys-
function or low EF by the EM residents/specialists.
In a study by Randazzo et al., the sensitivity of the left
ventricular EF in the EPSS method was 100%. However,
its specificity was below 51.6%.
12
Unlike this study,
Randazzo et al. observed the highest level of agreement
between the EM specialists and echocardiography spe-
cialists in the normal function category. This difference
between these studies could be attributed to the difference
between their inclusion and exclusion criteria and their
patient selection methods. In the study by Randazzo
et al.,
12
most participants were patients suffering from
low blood pressure, and only 5.7% of the 115 participants
had dyspnea. In contrast, one of the inclusion criteria in
this study was the presence of dyspnea.
A meta-analysis conducted by Albaroudi et al. assessed
the visual estimation technique by EM physicians, using
point-of-care echocardiography, compared with expert
Table 4. The Correlation Coefficient Between the Ejection Fraction Measured by Cardiologists and Emergency Medicine Residents.
N = 156
Cardiologists’ Report
Frequency (%)
Normal
Function
Mild
Dysfunction
Moderate
Dysfunction
Severe
Dysfunction
Qualitative Emergency medicine
residents’ report
Frequency (%)
Normal function 36 (23.1) 11 (7.0) 0 (0.0) 0 (0.0)
Mild dysfunction 19 (12.2) 42 (26.9) 5 (3.2) 1 (0.6)
Moderate dysfunction 1 (0.6) 5 (3.2) 16 (10.3) 5 (3.2)
Severe dysfunction 0 (0.0) 0 (0.0) 1 (0.6) 14 (9.0)
Result of statistical test Kappa contingency coefficient = .746
P = .000
Quantitative Result of statistical test Spearman correlation coefficient = .841
P = .000
Table 5. The Kappa Contingency Coefficient and Spearman
Correlation Coefficient for Each of the Diagnostic Methods
to Assess Cardiac Ejection Fraction.
Kappa
Contingency
Coefficient
Spearman
Correlation
Coefficient
Visual technique .697 .859
E-Point Septal Separation .487 .782
Simpson’s method .467 .847
Generally, a Kappa of less than .4 is considered poor (a Kappa of
0 means there is no difference between the observers and chance
alone). Kappa values of .4–.75 are considered moderate to good,
and a Kappa of >.75 represents excellent agreement. A Spearman’s
correlation is based on a perfect correlation approaching 1.0.

Mohammadi et al 573
sonographers. The sensitivity, specificity, and positive
and negative likelihood ratios of 89%, 85%, 5.98, and
0.13, respectively, were between clinician sonographers
and expert sonographers for normal and abnormal left
ventricular systolic function.
13
These findings compare
very nicely with the results of this study.
In comparison with this study, the work published by
Weekes et al.,
14
van Royen et al.,
15
and Amico et al.
16
demonstrated that the visual technique was superior to
the other relevant diagnostic methods in estimating the
EF. Jensen-Urstad et al.
17
and van’t Hof et al.
18
indicated
that the visual technique offered a high level of accuracy
in the estimation of EF. Gudmundsson et al. indicated that
the visual technique was like all the other EF calculation
methods, including Simpson’s method. None of these
evaluative methods for detecting EF is considerably
superior to the others.
19
In addition, a systematic review
by McGowan et al.
20
indicated that Simpson’s method,
EPSS, and the visual technique have similar advantages
and disadvantages.
In the study by McKaigney et al., they reported that
the visual technique has a weak correlation with the
actual output of the left ventricle. In contrast, the EPSS
method strongly correlates with the actual LVEF. Unlike
this study, in that report, the EPSS method was consider-
ably superior to the visual technique. They also referred
to its advantages, including faster deployment, less need
for the patient’s cooperation, and fewer views.
21
In another study, Rasooli et al. compared the echocar-
diography results between an EM resident and cardiolo-
gists. The study showed an acceptable agreement between
the results of the EM resident and cardiologists’ echocar-
diography in assessing regional wall motion abnormali-
ties in acute coronary syndrome.
22
One of the distinguishing features of this study was the
assessment of the EF by five different EM residents,
which indicated that well-trained EM residents could pro-
vide acceptable measurements of EF, within a short time
in the ED. As for all five trained residents, the agreements
between the residents and the cardiologists were signifi-
cant and almost similar.
Limitations
The major limitation to this study was the research design
and as such the pre-experimental nature and nonrandom-
ization of the patient’s evaluated hamper the results due
to threats to internal and external validity. These reliabil-
ity results are unique to these EM residents and the
patients that they examined. Another concern was that
this was a single-center trial that used convenience sam-
pling for patient selection. Future work in this area should
be conducted across multiple health care centers with a
variety of EM residents.
In addition, further limitations exist due to the difference
in the time of assessment by EM residents and cardiologists.
Although it is very unlikely, the patient’s systolic function
may change through long intervals in some cases and due to
changes in the patient’s condition, such as the development
of acidosis, electrolyte derangements, or the intake of vaso-
pressors. Therefore, future reliability studies should account
for the time interval between the bedside EF assessment and
the measurement by a cardiologist as a determining variable.
In addition, EPSS is an M-mode method that is no longer a
reliable measure to assess the EF. Although, in this study,
“eyeballing” provided the highest correlation between phy-
sicians, it is not considered a scientific method. Moreover,
the inclusion criteria of this study did not include a wide
range of patients with different conditions.
Conclusion
The results of this reliability study showed acceptable
agreement between the diagnostic measurement of EF by
trained EM residents and a cardiologist. Furthermore, this
study also revealed that that the visual technique had
more consistency between EM residents and a cardiolo-
gist. Thus, an effort should be considered to educate EM
residents on conducting cardiac sonogram and how to
make reliable measurements of EF in patients presenting
to the ED. Care should be taken in educating residents on
using the visual technique for assessing EF, as published
study results may not be generalizable or applicable in
certain patient populations. Although, in general, the goal
would be to promote Simpson’s method because of its
accuracy. Therefore, there may be value in instructing
and using different diagnostic methods for the measure-
ment of EF among EM residents and ED physicians.
Further research with more rigorous methodologies is
needed to confirm the results of this study.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect
to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research,
authorship, and/or publication of this article.
Ethics Approval
The study design was presented to the Ethics Committee of Iran
University of Medical Sciences and was approved (ethics code:
IR.IUMS.FMD.REC.1398.070).
Informed Consent
Informed consent was not sought for the present study because
all case data were de-identified and/or aggregated and followed

574 Journal of Diagnostic Medical Sonography 39(6)
ethics committee or IRB guidelines (also referred to as the
Honest Broker System).
Animal Welfare
Guidelines for humane animal treatment did not apply to the
present study because no animals were used during the study.
Trial Registration
Not applicable.
ORCID iDs
Seyedamir Tabibzadeh Dezfooli https://orcid.org/0000-0002-
4962-4223
Samira Vaziri
https://orcid.org/0000-0002-7556-6813
References
1. Yang E-S, Yeo W, Ko J-I, et al: Video clip training
improved emergency medicine residents’ interpretation
ability of visual ejection fraction. Hong Kong J Emerg
Med. 2020;27(1):15–23.
2. Shi D, Liu J, Xu J, Zhu H, Yu X: Evaluation of a new goal-
directed training curriculum for point-of-care ultrasound in
the emergency department: impact on physician self-con-
fidence and ultrasound skills. Eur J Trauma Emerg Surg.
2021;47(2):435–444.
3. Mansouri M, Kheyrollahi M, Mokhtari M: Comparison of
cardiac output measured by phonocardiography and trans-
thoracic echocardiography in patients with valvular dis-
ease and congenital heart anomalies. J Isfahan Med Sch.
2016;34(372):143–147.
4. Malakmohamadi M, Marage S: Echocardiographic versus
Fick method for determination of cardiac output in children
with various congenital heart diseases. J Shahrekord Univ
Med Sci. 2003;5(3):12–20.
5. Soroor-Azimzadeh B, Shamsadini S: Estimation of ejection
fraction with echocardiographic and cardioangiographic
methods in 50 cardiac patients. J Kerman Univ Med Sci.
2003;10(3):166–171.
6. Ünlüer EE, Karagöz A, Bayata S, Akoğlu H: An alternative
approach to the bedside assessment of left ventricular sys-
tolic function in the emergency department: displacement
of the aortic root. Acad Emerg Med. 2013;20(4):367–373.
7. Shahgaldi K, Gudmundsson P, Manouras A, Brodin L-Å,
Winter R: Visually estimated ejection fraction by two
dimensional and triplane echocardiography is closely cor-
related with quantitative ejection fraction by real-time
three dimensional echocardiography. Cardiovascular
Ultrasound. 2009;7:41.
8. Duvall WL, Croft LB, Goldman ME: Can hand-carried
ultrasound devices be extended for use by the noncardiology
medical community? Echocardiography. 2003;20(5):471–
476.
9. Nguyen N, Paschal G, Saul T, et al: Pilot study: ejection
fraction estimation by emergency medicine residents using
limited bedside echocardiography in the emergency depart-
ment. Ann Emerg Med. 2013;4(62):S80–S81.
10. Dresden S, Mitchell P, Rahimi L, et al: Right ventricu-
lar dilatation on bedside echocardiography performed by
emergency physicians aids in the diagnosis of pulmonary
embolism. Ann Emerg Med. 2014;63(1):16–24.
11. Unlüer EE, Karagöz A, Akoğlu H, Bayata S: Visual estima-
tion of bedside echocardiographic ejection fraction by emer-
gency physicians. West J Emerg Med. 2014;15(2):221–226.
12. Randazzo MR, Snoey ER, Levitt MA, Binder K: Accuracy
of emergency physician assessment of left ventricular ejec-
tion fraction and central venous pressure using echocar-
diography. Acad Emerg Med. 2003;10(9):973–977.
13. Albaroudi B, Hadda M, Albaroudi O, Abdel-Rahman M,
Jarman R, Harris T: Assessing left ventricular systolic
function by emergency physician using point of care echo-
cardiography compared to expert: systematic review and
meta-analysis. European J Emerg Med. 2022;29(1):18–32.
14. Weekes AJ, Tassone HM, Babcock A, et al: Comparison
of serial qualitative and quantitative assessments of caval
index and left ventricular systolic function during early
fluid resuscitation of hypotensive emergency department
patients. Acad Emerg Med. 2011;18(9):912–921.
15. van Royen N, Jaffe CC, Krumholz HM, et al: Comparison
and reproducibility of visual echocardiographic and quanti-
tative radionuclide left ventricular ejection fractions. Am J
Cardiol. 1996;77(10):843–850.
16. Amico AF, Lichtenberg GS, Reisner SA, Stone CK,
Schwartz RG, Meltzer RS: Superiority of visual versus
computerized echocardiographic estimation of radio-
nuclide left ventricular ejection fraction. Am Heart J.
1989;118(6):1259–1265.
17. Jensen-Urstad K, Bouvier F, Höjer J, et al: Comparison
of different echocardiographic methods with radionuclide
imaging for measuring left ventricular ejection fraction
during acute myocardial infarction treated by thrombolytic
therapy. Am J Cardiol. 1998;81(5):538–544.
18. van’t Hof AW, Schipper CW, Gerritsen JG, Reiffers S,
Hoorntje JC: Comparison of radionuclide angiography
with three echocardiographic parameters of left ventricular
function in patients after myocardial infarction. Int J Card
Imaging. 1998;14(6):413–418.
19. Gudmundsson P, Rydberg E, Winter R, Willenheimer R:
Visually estimated left ventricular ejection fraction by
echocardiography is closely correlated with formal quanti-
tative methods. Int J Cardiol. 2005;101(2):209–212.
20. McGowan JH, Cleland JG: Reliability of reporting left ven-
tricular systolic function by echocardiography: a systematic
review of three methods. Am Heart J. 2003;146(3):388–
397.
21. McKaigney CJ, Krantz MJ, La Rocque CL, Hurst ND,
Buchanan MS, Kendall JL: E-point septal separation:
a bedside tool for emergency physician assessment of
left ventricular ejection fraction. Am J Emerg Med.
2014;32(6):493–497.
22. Rasooli F, Bagheri F, Sadatnaseri A, Ashraf H, Bahreini
M: Comparison of emergency echocardiographic results
between cardiologists and an emergency medicine resi-
dent in acute coronary syndrome. Arch Acad Emerg Med.
2021;9(1):e53.

SDMS CME Credit – Determining the Extent of
Agreement for Determining the Echographic Ejection
Fraction Determined by Emergency Medicine
Residents Compared with a Cardiologist
SDMS members can earn SDMS CME credit by successfully completing the complimentary online
CME test in the SDMS Learning Center at learn.sdms.org. Non-members may access the online CME
test for a fee. Note: questions may appear in random order online.
1. Normal function is defined as an ejection fraction (EF)
of more than:
A. 55%
B. 50%
C. 75%
D. 45%
2. Jensen-Urstad et al. and van’t Hof et al. indicated that
the visual technique _______.
A. Was completely unreliable
B. Resulted in a low level of accuracy in the estima-
tion of EF
C. Was inconclusive
D. Offered a high level of accuracy in the estimation
of EF
3. The aim of this study was to ____________.
A. Determine the accuracy of EPSS measurement
B. Determine the extent of agreement on the mea-
sured echocardiographic EF measured by EM
residents compared to a cardiologist
C. Evaluate echocardiogram read times for critical
patients
D. Prove that visual assessment of EF is more accu-
rate than Simpson’s method
4. This study compared echocardiogram interpretations
from cardiologists and ________.
A. Emergency medicine residents
B. Cardiology fellows
C. General surgeons
D. Nurse practitioners
5. Based on the findings of this study, the overall agree-
ment percentage between the EM residents and cardi-
ologists was:
A. 90.3%
B. 70.5%
C. 69.3%
D. 89.0%
1201587JDM
XXX10.1177/87564793231201587Journal of Diagnostic Medical SonographyMeeting-Report
meeting-report2023
Authors: Fatemeh Mohammadi, MD, Seyedamir Tabibzadeh Dezfooli, MD, Babak Sadeghzadeh, PhD, Mojtaba Chardoli, PhD,
Hamed Basir Ghafouri, PhD, Mahdi Rezai, PhD, Reza Mosaddegh, PhD, and Samira Vaziri, PhD
Category: Cardiac (Adult) [AE]
Credit: 0.75 SDMS CME Credit
Objectives: After studying the article, you should be able to:
Define the method of measurement used: EPSS, Simpson’s method, or visual assessment.
Discuss the extent of agreement on the measured echocardiographic ejection fraction (EF) measured by emergency medicine
(EM) residents compared with a cardiologist.
Explain the value of educating EM residents to interpret echocardiographic ejection fraction.
