are located on the Carriers and Benefit Plans webpage.
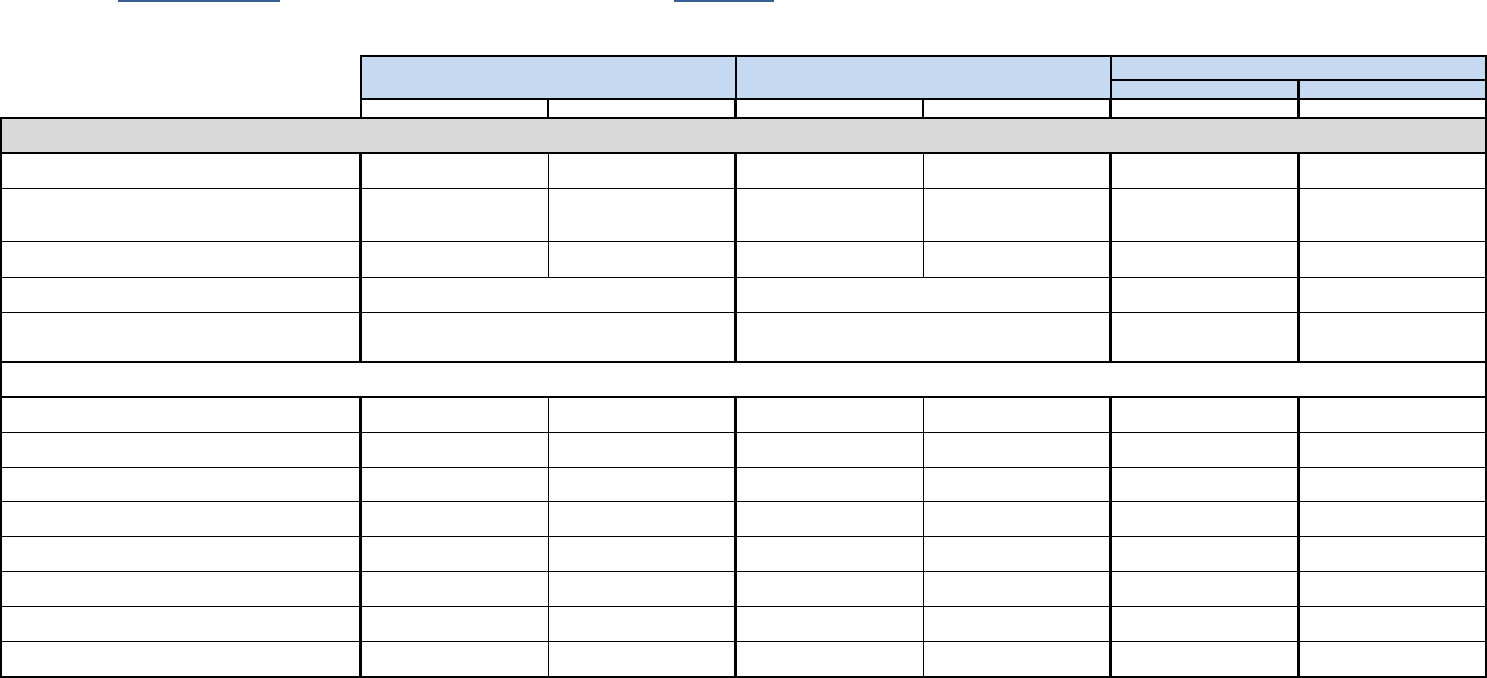
Blue Care Network Health Alliance Plan
In-Network Out-of-Network In-Network Out-of-Network In-Network In-Network
Deductible
3
$400/individual
4
$800/family
$800/individual
4
$1,600/family
$1,600/individual
5
$3,200/family
$3,200/individual
5
$6,400/family
$125/individual
6
$250/family
$125/individual
6
$250/family
Coinsurance
10% for most services.
20% for acupuncture
20% for most services
50% for mental health and
substance use disorder
20% for most services
40% for acupuncture
40% for most services N/A N/A
Out-Of-Pocket Maximum
7
$2,000/individual
$4,000/family
$3,000/individual
$6,000/family
$4,000/individual
$8,000/family
$8,000/individual
$16,000/family
$2,000/individual
$4,000/family
$2,000/individual
$4,000/family
Health Savings Account (HSA) Employer Annual Contribution N/A N/A
Annual gynecological exam, 1 per plan year Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Childhood Immunization (through age 16) Covered 100% Covered 80% Covered 100%
Covered 60%
after deductible
Covered 100% Covered 100%
Colonoscopy
12
Covered 100%
Covered 80%
after deductible
Covered 100%
Covered 60%
after deductible
Covered 100% Covered 100%
Fecal occult blood screening
12
Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Flexible sigmoidoscopy
12
Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Health maintenance exam, 1 per plan year Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Immunizations, annual flu shot, & Hepatitis C screening for
those at risk
Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Mammography
12
Covered 100%
Covered 80%
after deductible
Covered 100%
Covered 60%
after deductible
Covered 100% Covered 100%
State Health Plan PPO (80%)
State High Deductible Health Plan with HSA
1
HMOs (85%)
2
2
The State will pay up to 85% of the applicable HMO total premium, capped at the dollar amount which the State pays for the same coverage code under the SHP PPO.
3
Deductible amounts for all health plans are effective January 1 and renew annually on a calendar basis. The deductible for the HDHP is combined for medical and pharmacy.
4
The SHP PPO individual deductible is the maximum amount that applies to any one family member. The family deductible is the combined maximum deductible amount that applies to any combination of family members. One family member is not required to reach the
individual deductible before that family deductible can be met. Additionally, one family member cannot contribute in excess of the maximum amount of the individual deductible.
5
The HDHP Individual deductible only applies to employee only coverage. The HDHP Family deductible applies to the coverage of employee plus spouse and/or other dependents. The applicable deductible must be fulfilled prior to services being paid by the plan. Any one
member of the family or any combination of family members may fulfill the entire family deductible.
This comparison chart is intended as an easy-to-read benefit summary. Additional limitations, exclusions, and/or prior authorizations may apply to covered services. Payment amounts are based on the carrier's approved amount, less any
applicable deductible, copay amounts, and/or coinsurance. Pre-existing conditions are covered with the applicable deductibles and copays for the covered benefit. Contact information, websites, plan booklets and Summary of Benefits
2024 Comparison of PPO, State HDHP, and HMO Plans
Blue Cross Blue Shield of Michigan
Blue Cross Blue Shield of Michigan
Retail-$10/$30/$60
Mail Order-$20/$60/$120
$750/individual
8
$1,500/family
After deductible is met, the following copays apply
10
:
Retail-$10/$30/$60
Mail Order-$20/$60/$120
Deductible, Copays, Out-of-Pocket Maximum, and Prescription Drugs
Retail-$10/$30/$60
Mail Order-$20/$60/$120
Preventive Services
11
6
The HMO individual deductible is the maximum amount that applies to any one family member. The family deductible is the combined maximum deductible amount that applies to any combination of family members. One family member is not required to reach the individual
deductible before that family deductible can be met. Additionally, one family member cannot contribute in excess of the maximum amount of the individual deductible. Check with your HMO to see if any Out-of-Network services are covered and the applicable Out-of-Network
deductible that would apply.
Prescription Drug copays
9
1
MSP DROP employees (bargaining unit T01 and Command Officers) and OEAIs are excluded from enrollment in the State HDHP with HSA.
7
Out-Of-Pocket Maximum amounts for all health plans are effective January 1 and renew annually on a calendar basis. Only In-Network deductibles, fixed-dollar copayments, prescription drug copayments,
and coinsurance apply toward the out-of-pocket maximum.
9
The SHP PPO and State HDHP with HSA only allow a 30-day supply at a retail pharmacy and 90-day supply through mail order. BCN allows up to a 90-day supply of non-specialty medications at both retail and mail order. HAP allows a 30-day supply at a retail pharmacy and
90-day supply through mail order. HAP allows select medications as a 90-day supply at retail.
Premiums for each benefit plan are located on the Insurance Rates webpage.
N/A
Retail-$10/$30/$60
Mail Order-$20/$60/$120
8
Funded 100% on the 1st pay period of each plan year. The State will make a contribution of $750 for an individual employee or $1,500 for employees who enroll effective January 1st with one or more dependents. This contribution will be prorated for employees who enroll mid-
year based on the number of pay periods remaining in the plan year at the time of enrollment in the HDHP.
10
The deductible does not apply to certain preventive medications under the State HDHP with HSA.
11
Preventive Services are not subject to the deductible.
12
Patient Protection and Affordable Care Act (PPACA) guidelines apply.

are located on the Carriers and Benefit Plans webpage.
Blue Care Network Health Alliance Plan
In-Network Out-of-Network In-Network Out-of-Network In-Network In-Network
State Health Plan PPO (80%)
State High Deductible Health Plan with HSA
1
HMOs (85%)
2
This comparison chart is intended as an easy-to-read benefit summary. Additional limitations, exclusions, and/or prior authorizations may apply to covered services. Payment amounts are based on the carrier's approved amount, less any
applicable deductible, copay amounts, and/or coinsurance. Pre-existing conditions are covered with the applicable deductibles and copays for the covered benefit. Contact information, websites, plan booklets and Summary of Benefits
2024 Comparison of PPO, State HDHP, and HMO Plans
Blue Cross Blue Shield of Michigan
Blue Cross Blue Shield of Michigan
Deductible, Copays, Out-of-Pocket Maximum, and Prescription Drugs
Premiums for each benefit plan are located on the Insurance Rates webpage.
Pap smear screening - laboratory services only
12
,
1 per plan year
Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Prostate specific antigen screening
12
,
1 per plan year
Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Well-baby and child care Covered 100% Not Covered Covered 100% Not covered Covered 100% Covered 100%
Office and Outpatient hospital visits, consultations, and urgent
care visits
$20 copay
(deductible not applicable)
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
$20 copay
(deductible not applicable)
$20 copay
(deductible not applicable)
Outpatient and home visits
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
$20 copay
(deductible not applicable)
$20 copay
(deductible not applicable)
Telemedicine (Medical) -
via the Carrier's online vendor
$0 copay
(deductible not applicable)
Not Covered
Covered 80%
after deductible
Not covered
$10 Copay
(deductible not applicable)
$10 Copay
(deductible not applicable)
Telemedicine (Behavioral Health) -
via the Carrier's online vendor
$0 copay
(deductible not applicable)
Not Covered
Covered 80%
after deductible
Not covered
$0 copay
(deductible not applicable)
$10 Copay
(deductible not applicable)
Telemedicine (Medical) -
via the Provider's online tool
$20 copay
(deductible not applicable)
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
$20 copay
(deductible not applicable)
$20 copay
(deductible not applicable)
Telemedicine (Behavioral Health) -
via the Provider's online tool
$20 copay
13
(deductible not applicable)
Covered 50% of allowed
amount or billed charges
(whichever is less)
Covered 80%
after deductible
Covered 60%
after deductible
$0 copay
(deductible not applicable)
$0 copay
(deductible not applicable)
Ambulance services - medically necessary
Covered 100%
after deductible
Covered 100%
after deductible
Hospital emergency room for medical emergency or
accidental injury
$200 copay
(Waived if admitted
as inpatient)
$200 copay
(Waived if admitted
as inpatient)
Diagnostic tests and x-rays
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
after deductible
(May require authorization)
Covered 100%
after deductible
Laboratory and pathology tests
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
(May require authorization)
Covered 100%
Radiation therapy
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
after deductible
(Requires authorization)
Covered 100%
after deductible
Delivery and nursery care
Covered 90%
after deductible
Covered 80%
after deductible
Covered 100%
after deductible
Covered 100%
after deductible
Prenatal care
11
Postnatal care
11
12
Patient Protection and Affordable Care Act (PPACA) guidelines apply.
Covered 100%
Covered 100%
Covered 100%
Covered 100%
Covered 90%
after deductible
$200 copay
(Waived if admitted as inpatient)
Covered 80%
after deductible
Covered 60%
after deductible
Maternity Services (Includes care by a certified nurse midwife SHP PPO Only)
Diagnostic Services
Covered 80%
after deductible
Emergency Medical Care
Physician Office Services
11
Preventive Services are not subject to the deductible.
Preventive Services
11
(continued)
13
$20 copay or 10% coinsurance (whichever is less) for Telemedicine via an in-network provider's online tool for Behavioral Health.

are located on the Carriers and Benefit Plans webpage.
Blue Care Network Health Alliance Plan
In-Network Out-of-Network In-Network Out-of-Network In-Network In-Network
State Health Plan PPO (80%)
State High Deductible Health Plan with HSA
1
HMOs (85%)
2
This comparison chart is intended as an easy-to-read benefit summary. Additional limitations, exclusions, and/or prior authorizations may apply to covered services. Payment amounts are based on the carrier's approved amount, less any
applicable deductible, copay amounts, and/or coinsurance. Pre-existing conditions are covered with the applicable deductibles and copays for the covered benefit. Contact information, websites, plan booklets and Summary of Benefits
2024 Comparison of PPO, State HDHP, and HMO Plans
Blue Cross Blue Shield of Michigan
Blue Cross Blue Shield of Michigan
Deductible, Copays, Out-of-Pocket Maximum, and Prescription Drugs
Premiums for each benefit plan are located on the Insurance Rates webpage.
Chemotherapy
Dialysis services
Inpatient consultations
Semi-private room, inpatient physician care, general nursing
care, hospital services, and supplies (unlimited days)
Covered 100%
after deductible
(Requires authorization)
Home health care
Covered 90%
after deductible
(participating providers
only; unlimited visits)
Not Covered
Covered 80%
after deductible
(participating providers only;
unlimited visits)
Not Covered
Covered 100%
After Deductible,
$20 Copay
Covered 100%
After Deductible,
$20 Copay
(Unlimited visits;
excludes PT/OT/ST)
Hospice care
Covered 100%
(participating provider only)
Not Covered
Covered 80%
after deductible
(participating provider only)
Not Covered
Covered 100%
After Deductible
(Inpatient care requires
authorization)
Covered 100%
after deductible
Skilled nursing care
(up to 120 days per confinement)
Covered 90%
after deductible
(Blue Cross approved facility)
Not Covered
Covered 80%
after deductible
(Blue Cross approved facility)
Not Covered
Covered 100%
after deductible
(Requires authorization)
Covered 100%
after deductible
Anesthesia
Covered 100%
After Deductible
Covered 100%
After Deductible
Female voluntary sterilization
12
Covered 100% Covered 100% Covered 100%
Male voluntary sterilization
Covered 100%
after deductible
Surgery - includes related surgical services
Covered 90%
after deductible
Covered 100%
after deductible
(Requires authorization)
Bone marrow-specific criteria applies
Covered 100%
(in designated facilities)
Not Covered
Covered 80%
after deductible
(in designated facilities)
Not Covered
Covered 100%
after deductible
(In designated facilities;
requires authorization)
Covered 100%
after deductible
(in designated facilities)
Kidney, cornea, and skin
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
after deductible
(Subject to medical criteria;
requires authorization)
Covered 100%
after deductible
(subject to medical criteria)
Alternative to Hospital Care
Human Organ Transplants
Covered 60%
after deductible
Covered 80%
after deductible
Covered 100%
Covered 80%
after deductible
Covered 100%
after deductible
12
Patient Protection and Affordable Care Act (PPACA) guidelines apply.
Hospital Care
Surgical Services
Covered 90% after deductible
Covered 80% after deductible
Covered 60%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 90%
after deductible
Covered 100%
after Deductible
Covered 100%
after deductible

are located on the Carriers and Benefit Plans webpage.
Blue Care Network Health Alliance Plan
In-Network Out-of-Network In-Network Out-of-Network In-Network In-Network
State Health Plan PPO (80%)
State High Deductible Health Plan with HSA
1
HMOs (85%)
2
This comparison chart is intended as an easy-to-read benefit summary. Additional limitations, exclusions, and/or prior authorizations may apply to covered services. Payment amounts are based on the carrier's approved amount, less any
applicable deductible, copay amounts, and/or coinsurance. Pre-existing conditions are covered with the applicable deductibles and copays for the covered benefit. Contact information, websites, plan booklets and Summary of Benefits
2024 Comparison of PPO, State HDHP, and HMO Plans
Blue Cross Blue Shield of Michigan
Blue Cross Blue Shield of Michigan
Deductible, Copays, Out-of-Pocket Maximum, and Prescription Drugs
Premiums for each benefit plan are located on the Insurance Rates webpage.
Liver, heart, lung, pancreas, and other specified organ
transplants
Covered 100%
(in designated facilities)
Not Covered
Covered 80%
after deductible
(in designated facilities)
Not Covered
Covered 100%
after deductible
(In designated facilities;
requires authorization)
Covered 100%
after deductible
(in designated facilities)
Acupuncture
Not Covered Not Covered
Allergy injections Covered 100% Covered 100%
Allergy testing and therapy (non-injection)
Covered 100%
after deductible
Autism - Spectrum Disorder Applied Behavioral Analysis
(ABA) treatment
Covered 100%
Bariatric Surgery
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
After Deductible
(Limited one per lifetime;
requires authorization)
Covered 100%
After Deductible,
$1,000 Copay per admission;
One procedure per lifetime
Cardiac Rehabilitation & Pulmonary Rehabilitation
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered, $20 Copay
(Limited to 36 visits per
plan year)
Covered 100%
after deductible
Chiropractic/spinal manipulation
$20 copay
(Up to 24 visits per
calendar year)
Covered 80%
after deductible
(Up to 24 visits per
calendar year)
Covered 80%
after deductible
(up to 24 visits per
calendar year)
Covered 60%
after deductible
(up to 24 visits per
calendar year)
Chiropractic spinal
manipulation when
referred by PCP,
Covered After Deductible,
$20 Copay. Deductible
applies to x-rays.
Covered
$20 Copay
(Manipulations only,
up to 24 visits per
plan year)
Durable medical equipment Covered 100%
Covered 80%
of the Blue Cross approved
amount plus, the difference
between charge and approved
amount
Covered 80%
after deductible
Covered 60%
after deductible
of the Blue Cross approved
amount plus, the difference
between charge and approved
amount
Covered 100%
(Must be authorized and
obtained from a BCN supplier)
Covered 100%
Hearing Aids
Covered 100%
(standard and binaural aids)
Not Covered
Covered 80%
after deductible
Not Covered
Covered (for conventional
standard hearing aids; Limited
to one monaural with a max
benefit of $654 or one binaural
with a max benefit of $1,177;
every 36 months)
Covered, copay based
on type of Hearing Aid.
Deductible does not
apply. Through a
NationsHearing provider
only. Limit of coverage is
one (1) Hearing Aid per
ear per plan year.
Hearing Care Exam
$20 copay
for office visit
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
(Performed in Physician's
Office, $20 copay may apply)
Covered 100%
($20 Office copay
may apply)
Infertility Counseling & Treatment Not Covered Not Covered Not Covered Not Covered
Covered 100%
After Deductible
(Excludes in-vitro fertilization)
Covered 100%
After Deductible;
(One attempt of artificial
insemination per lifetime)
Nutritional & Health education and counseling Covered 100% Not Covered Covered 100% Not Covered Covered 100%
Covered 100%
(Limitations apply)
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 60% after deductible
(if performed by a participating acupuncturist
or under the supervision of a M.D. or D.O.)
Human Organ Transplants (continued)
Covered 90%
after deductible
Covered 80% after deductible
(if performed by a participating acupuncturist
or under the supervision of a M.D. or D.O.)
Other Services
Covered 100%
After Deductible

are located on the Carriers and Benefit Plans webpage.
Blue Care Network Health Alliance Plan
In-Network Out-of-Network In-Network Out-of-Network In-Network In-Network
State Health Plan PPO (80%)
State High Deductible Health Plan with HSA
1
HMOs (85%)
2
This comparison chart is intended as an easy-to-read benefit summary. Additional limitations, exclusions, and/or prior authorizations may apply to covered services. Payment amounts are based on the carrier's approved amount, less any
applicable deductible, copay amounts, and/or coinsurance. Pre-existing conditions are covered with the applicable deductibles and copays for the covered benefit. Contact information, websites, plan booklets and Summary of Benefits
2024 Comparison of PPO, State HDHP, and HMO Plans
Blue Cross Blue Shield of Michigan
Blue Cross Blue Shield of Michigan
Deductible, Copays, Out-of-Pocket Maximum, and Prescription Drugs
Premiums for each benefit plan are located on the Insurance Rates webpage.
Orthognathic Surgery
Covered 90%
after deductible
(Limitations apply)
Covered 80%
after deductible
(Limitations apply)
Covered 80%
after deductible
(Limitations apply)
Covered 60%
after deductible
(Limitations apply)
Covered 100%
After Deductible
(Limitations apply)
Covered 100%
After Deductible
Oral Surgery
Covered 90%
after deductible
(Limitations apply)
Covered 80%
after deductible
(Limitations apply)
Covered 80%
after deductible
(Limitations apply)
Covered 60%
after deductible
(Limitations apply)
Covered 100%
After Deductible
(For accidental injury;
limitations apply)
Covered 100%
After Deductible
*Limited to emergency oral
surgery/dental services for the
prompt stabilization of
traumatic injury to natural
teeth or related body tissue
resulting from a
nonoccupational injury
Prosthetic and orthotic appliances Covered 100%
Covered 80%
of the Blue Cross approved
amount plus, the difference
between charge and approved
amount
Covered 80%
after deductible
Covered 60%
after deductible
of the Blue Cross approved
amount plus, the difference
between charge and approved
amount
Covered 100%
(Must be authorized and
obtained from a BCN supplier)
Covered 100%
Private duty nursing
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
After Deductible
(Requires authorization)
Covered 100%
Rabies treatment after initial emergency room visit
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Office visit $20 copay;
Injections Covered 100%
Office visit $20 copay;
Injections Covered 100%
Temporomandibular Joint Syndrome (TMJS)
Covered 90%
after deductible
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
After Deductible
(Limitations apply)
Covered 100%
After Deductible
Vision Screening (performed in a physician’s office, one exam
per plan year)
Covered 100% Not Covered Covered 100% Not Covered Covered 100% Covered 100%
Wig, wig stand, adhesives Not covered Not covered
Covered 100%
for hair prosthesis (wig or hair
piece) for hair loss due to a
medical condition or the
treatment of a medical
condition. One per calendar
year; max benefit $225 per
year.
Covered 100%;
$300 lifetime maximum
benefit
Alcohol & Chemical Dependency Benefits - Inpatient
Covered 100%
14
Halfway House 100%
(requires authorization)
Covered 50% of allowed
amount or billed charges
(whichever is less)
14
Halfway House 50% (requires
authorization)
Covered 80%
14
after deductible
(requires authorization)
Covered 60%
14
after deductible
(requires authorization)
Covered 100%
After Deductible
(Requires authorization)
Covered 100%
After Deductible
(Requires authorization)
Alcohol & Chemical Dependency Benefits - Outpatient
Covered 90%
of network rates
Covered 50% of allowed
amount or billed charges
(whichever is less)
Covered 80%
after deductible
Covered 60%
after deductible
Covered 100%
$20 Copay
(deductible not applicable)
Upon meeting medical conditions, eligible for a lifetime
maximum reimbursement of $300. (Additional wigs covered for
children due to growth).
Behavioral Health / Substance Use Disorder
Other Services (continued)
14
Two 28-day admissions per year with at least 60 days between admissions. Inpatient days may be utilized for Intensive Outpatient Program (IOP) treatment at 2:1 ratio. One inpatient day equals two IOP days.

are located on the Carriers and Benefit Plans webpage.
Blue Care Network Health Alliance Plan
In-Network Out-of-Network In-Network Out-of-Network In-Network In-Network
State Health Plan PPO (80%)
State High Deductible Health Plan with HSA
1
HMOs (85%)
2
This comparison chart is intended as an easy-to-read benefit summary. Additional limitations, exclusions, and/or prior authorizations may apply to covered services. Payment amounts are based on the carrier's approved amount, less any
applicable deductible, copay amounts, and/or coinsurance. Pre-existing conditions are covered with the applicable deductibles and copays for the covered benefit. Contact information, websites, plan booklets and Summary of Benefits
2024 Comparison of PPO, State HDHP, and HMO Plans
Blue Cross Blue Shield of Michigan
Blue Cross Blue Shield of Michigan
Deductible, Copays, Out-of-Pocket Maximum, and Prescription Drugs
Premiums for each benefit plan are located on the Insurance Rates webpage.
Behavioral Health Benefit - Inpatient
Covered 100%
(up to 365 days per year
15
;
requires authorization)
Covered 50% of allowed
amount or billed charges
(whichever is less); up to 365
days per year
15
; requires
authorization
Covered 80%
after deductible
(unlimited days
15
; requires
authorization)
Covered 60%
after deductible
(unlimited days
15
; requires
authorization)
Covered 100%
After Deductible
(Requires authorization)
Covered 100%
After Deductible
(Requires authorization)
Behavioral Health Benefit - Outpatient
Covered 90% of
network rates
Covered 50% of allowed
amount or billed charges
(whichever is less)
$20 Copay
(deductible not applicable)
Intensive Outpatient Program (IOP) - Behavioral Health and
Substance Use Disorder
Covered 100%
Covered 50% of allowed
amount or billed charges
(whichever is less)
$20 Copay
(deductible not applicable)
Outpatient Physical, Speech, Occupational, and Massage
therapy - facility and clinic services
17
Outpatient Physical therapy - physician's office
Covered 80%
after deductible
Covered 80%
after deductible
Covered 60%
after deductible
Covered 60% after deductible
Covered 80% after deductible
16
Massage therapy is not a covered benefit under the HMOs.
17
Massage therapy is performed by a massage therapist must be supervised by a chiropractor and be part of a formal course of physical therapy. Massage therapy is provided as part of a formal course of physical therapy treatment and when billed alone is not a covered
benefit.
Covered, $20 Copay
(Requires authorization;
unlimited visits for spectrum
disorder)
Covered 90%
after deductible
15
Inpatient days may be utilized for partial day hospitalization (PHP) at 2:1 ratio. One inpatient day equals two PHP days.
Behavioral Health / Substance Use Disorder (continued)
Outpatient Physical, Speech, Occupational, and Massage Therapy
15
(Combined maximum of 90 visits per calendar year)
Covered, $20 Copay
(Up to combined
max of 100 visits
per plan year)
Covered 100%
